15
Chronic pain
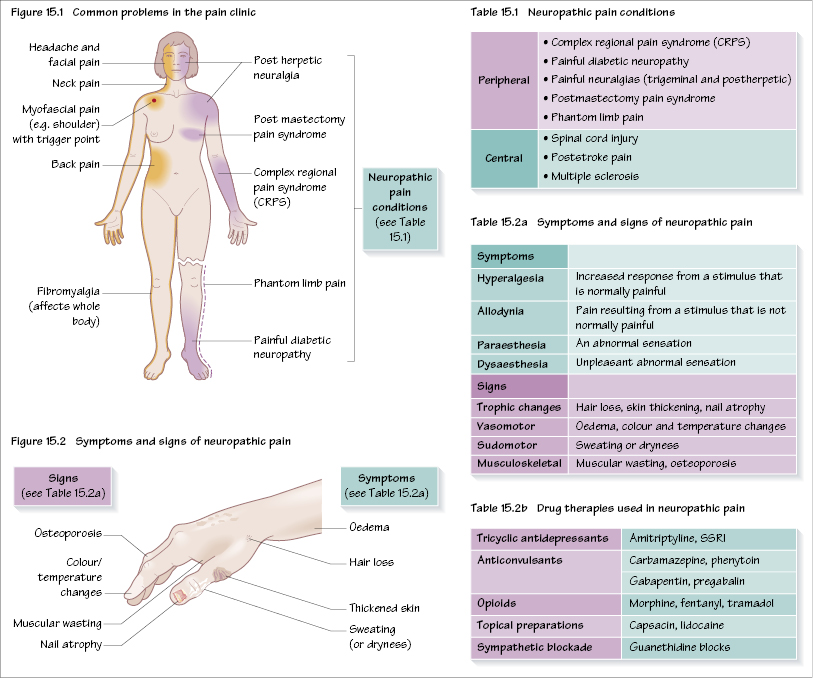
Whilst acute pain is a self-limiting process and is usually a clinical entity for only a few days, chronic pain persists longer than the expected time of healing and becomes the illness itself rather than a symptom of it. In addition there are other changes, particularly psychological. Chronic pain represents a wide spectrum of disease entities (Figure 15.1).
The mechanisms and pathways involved in chronic pain may be different to acute (nociceptive) pain. An important feature of some chronic pain syndromes is neuropathic pain, which is caused by central nervous system dysfunction, and often results in pain long after any painful stimulus has disappeared. There are many proposed mechanisms, including spontaneous activity within the dorsal root ganglion (DRG) and sympathetic nerve sprouting into the DRG. Within the dorsal horn, changes may also occur due to a reduction in inhibitory influences. In addition, there may be rewiring so that Aβ fibres (carrying touch) are synapsing on pain fibres. This different mechanism of pain gives rise to different treatments; indeed, conventional analgesics for acute pain may be ineffective for neuropathic pain.
Neuropathic pain
Neuropathic pain may be classified as either peripheral or central (see Table 15.1).
There are a number of features of neuropathic pain, which are shown in Figure 15.2. A classical type of neuropathic pain, complex regional pain syndrome (CRPS), typifies this clinical condition. It may follow an injury (e.g. Colles fracture) or there may be no injury. There may also be varying degrees of sympathetic nervous system involvement. With sympathetically maintained pain a sympathetic blockade will alleviate pain, whereas with sympathetically independent pain sympathetic blockade will have little effect.
Treatmen/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


