Treatment Strategies for Developing and Nondeveloping Class III Malocclusions
Peter W. Ngan, Jae-Hyun Sung
Class III malocclusions can be broadly divided into two categories: developing and nondeveloping malocclusions. A number of authors have recommended early treatment of developing Class III malocclusions to obtain growth modification. The validity of two-phase treatment is supported by studies that show greater orthopedic effects when treatment is started in younger patients.1,2 On the other hand, several investigators reported significant relapse for patients who resume the original growth pattern after treatment.3 The question is whether a two-phase Class III treatment is worth the burden. If so, is early treatment suitable for all types of Class III malocclusions? In this chapter we classify developing Class III malocclusions into four categories and discuss strategies for selecting appliances to treat the various types of developing Class III malocclusions.
For Class III patients with no remaining growth, the nondeveloping malocclusions can be camouflaged by dentoalveolar tooth movement. Different approaches to camouflage a Class III malocclusion have been suggested, ranging from extraction of premolars to en masse distalization of the entire lower arch.4 With the advent of micro-implants, it is possible to increase the range of orthodontic tooth movement without encountering the side effects associated with traditional treatment mechanics.5,6 This chapter suggests possible treatment strategies for patients with no remaining growth who require tooth movement to camouflage skeletal discrepancies.
Diagnosis and Classification of Class III Malocclusions
The prevalence of Class III malocclusion varies among different ethnic groups. The prevalence in Caucasians ranges between 1% and 4% depending on the method of studying the malocclusion and the age group evaluated.7–10 A high prevalence of Class III malocclusion has been observed in Asian populations such as Chinese (4% to 12%),11–14 Japanese (2.3% to 13%),15,16 and Koreans (9% to 19%).17 A relatively high prevalence of Class III malocclusion was also reported in countries such as Saudi Arabia (9.4%)18 and Sweden (6%).19 This was in contrast to African Americans (0.6% to 1.2%).20
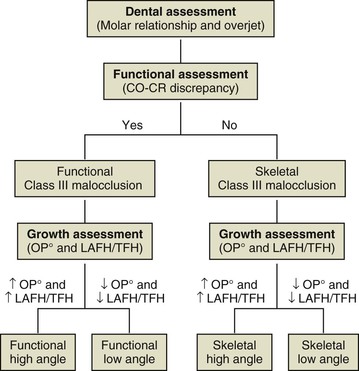
Individuals with Class III malocclusion and anterior crossbites may have combinations of skeletal and functional (dentoalveolar) components. Consideration of these components is essential so that the underlying cause of the discrepancy can be treated appropriately. To differentiate between skeletal and functional malocclusions, patients who present with Class III molar relationship and/or anterior crossbite should be checked for the presence of a functional shift (Fig. 14-1). First, clinicians should assess the relationship of the mandible to the maxilla to determine whether a centric relation–centric occlusion discrepancy exists. Anterior positioning of the mandible may result from abnormal tooth contact that forces the mandible forward. Patients who present with a forward shift of the mandible on closure may have a normal facial profile and Class I molar relationship in centric relation (CR) but a prognathic profile and Class III molar relationship in centric occlusion (CO), a situation referred to as “pseudo Class III malocclusion.” Elimination of CO-CR shift should reveal whether it is a simple Class I malocclusion or a compensated Class III malocclusion with lingual tipping of the lower incisors. On the other hand, a patient presenting with no shift on closure, a full-step Class III molar relationship, and a mesial occlusion of the lower to upper canines most likely has a skeletal Class III malocclusion. Second, Class III patients should be evaluated in the vertical dimension for vertical hypodivergent or hyperdivergent growth pattern. This can be achieved by measuring the inclination of the occlusal plane (OP°) and the ratio of lower anterior facial height (LAFH) to total facial height (TFH). The average occlusal plane inclination is 7 degrees. Patients with OP° greater than 7 degrees are considered to have a hyperdivergent growth pattern or be high angle cases and those with OP° less than 7 degrees are considered to have a hypodivergent growth pattern or be low angle cases. Similarly, patients with a ratio of LAFH/TFH greater than 0.55 are high angle cases and those with a ratio less than 0.55 are low angle cases. Class III patients can then be classified into four types: functional low angle, skeletal low angle, functional high angle, and skeletal high angle. The classification of malocclusion will aid in the selection of appliances for early orthopedic treatment, as discussed in the following section (see Fig. 14-1).
Treatment of Developing Class III Malocclusion
Expansion and Partial Fixed Appliance
Correction of multiple teeth in anterior crossbite is best accomplished with a fixed appliance. An expansion appliance or maxillary lingual arch in conjunction with a partial fixed appliance can be used to correct anterior crossbite in young Class III patients.
Treatment Effects
Figure 14-2 shows an 8-year-old patient who presented with multiple teeth in anterior crossbite. A Hyrax maxillary expansion appliance was fabricated to create arch length for the alignment of the maxillary incisors. After expansion, a sequence of three archwires (0.012-inch nickel-titanium [Ni-Ti], 0.018-inch Ni-Ti, and 0.018-inch stainless steel) was used to align the maxillary incisors. A coil spring can be inserted between the maxillary lateral incisors and the first primary molars to help in the correction of crossbite. The correction is usually accomplished within 6 months and retainers are usually not necessary if overbite is adequate after crossbite correction (see Fig. 14-2).

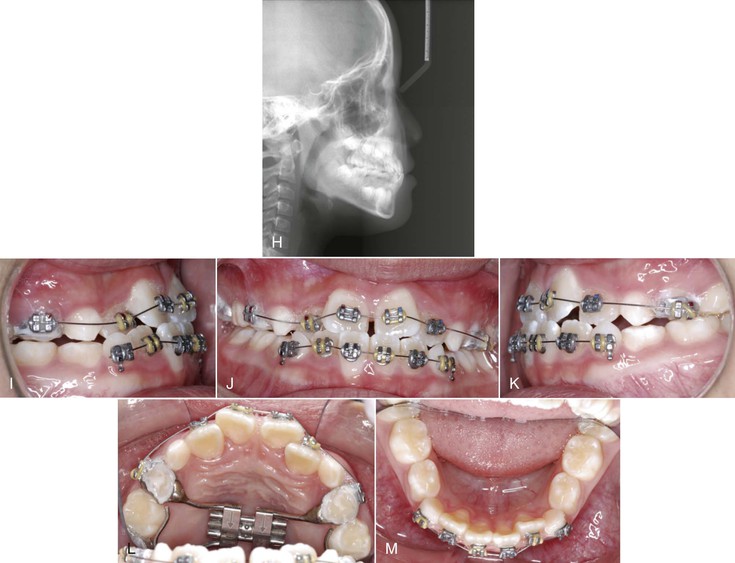
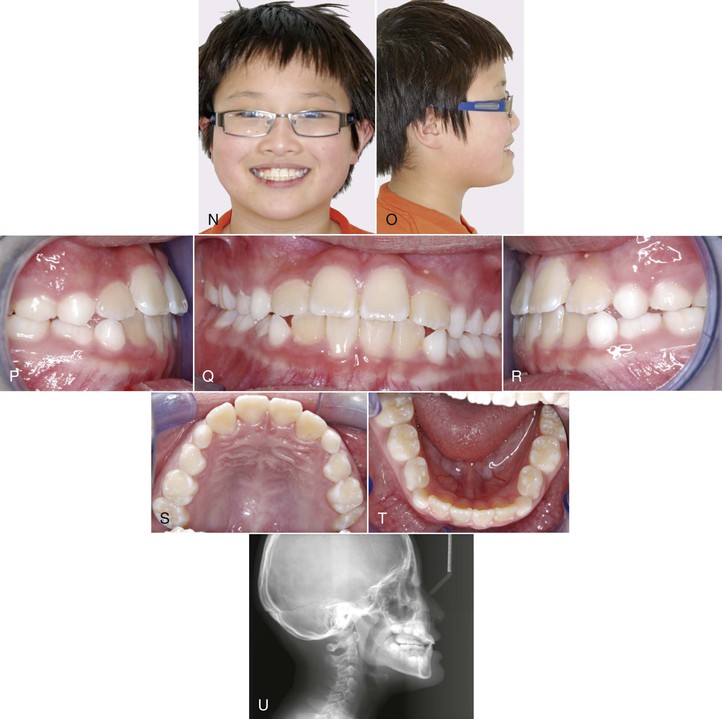
Figure 14-2 Pre-treatment (A and B) facial and (C–G) intraoral photographs of an 8-year-old patient who presented with multiple teeth in anterior crossbite. H, Cephalometric radiograph showing a mild skeletal growth pattern. I–M, A Hyrax maxillary expansion appliance was fabricated to create arch length for the alignment of the maxillary incisors. A sequence of three archwires (0.012-inch nickel-titanium [Ni-Ti], 0.018-inch Ni-Ti, and 0.018-inch stainless steel) was used to align the maxillary incisors. Post-treatment (N and O) facial and (P–T) intraoral photographs show the correction of anterior crossbite. U, Post-treatment cephalometric radiograph shows the crossbite was corrected by proclination of the maxillary incisors and retroclination of the mandibular incisors.
Limitations
Several investigators reported forward movement of the maxilla with maxillary expansion. However, the effect was not consistent and was rarely more than 1.5-mm. A rapid palatal expansion (RPE) appliance in conjunction with a protraction facemask is recommended for patients diagnosed with functional hypodivergent or hyperdivergent types of Class III malocclusions.
Protraction Facemask Therapy
Treatment Effects
Meta-analysis showed that the treatment effects of using protraction facemask to correct anterior crossbite are a combination of skeletal and dental changes of the maxilla and mandible.21 The maxilla moves downward and forward with a slight upward movement in the anterior and downward movement in the posterior palatal plane as the result of protraction force; at the same time posterior teeth extrude somewhat. As a consequence, downward and backward rotation of the mandible improves the maxillomandibular skeletal relationship in the sagittal dimension but results in an increase in lower anterior facial height. This rotation is a major contributing factor in establishing an anterior overjet improvement. A force exerted by the chin cup has been speculated to help in redirecting the mandibular downward and backward growth. Upper incisor labial inclination increased, although lower incisor inclination decreased. It is postulated that upper incisor proclination is due to mesial dental movement and lower incisor uprighting occurs as the result of pressure by the chin cup and soft tissue.
In the mixed dentition, a banded or bonded expansion appliance can be fabricated as anchorage for maxillary protraction. Patients with an increased lower face height can benefit from using a bonded expansion appliance, which provides a temporary biteplate effect. Additionally, a bonded maxillary appliance can be used in patients with a deep overbite and overclosure of the mandible to facilitate the jumping of the anterior crossbite. The expansion appliance is activated twice daily (0.25-mm per turn) by the patient or parent for 7 to 10 days. In patients with a more constricted maxilla, activation of the appliance is carried out for 2 weeks or longer.
Several facial sutures play an important role in the development of the nasomaxillary complex, including the frontomaxillary, nasomaxillary, zygomaticotemporal, zygomaticomaxillary, pterygopalatine, intermaxillary, ethmomaxillary, and lacrimomaxillary sutures.22 Animal studies have shown that the maxillary complex can be displaced anteriorly with significant changes in the facial sutures.23 However, maxillary protraction does not always result in forward movement of the maxilla. With the same line of force, different midfacial bones were displaced in different directions depending on the moments of force generated at the sutures. The center of resistance (CRES) of the maxilla was found to be located at the distal contacts of the maxillary first molars one-half the distances from the functional occlusal plane to the inferior border of the orbit. Protraction of the maxilla below the CRES produces counterclockwise rotation of the maxilla, which may not be favorable for patients with open-bite tendency.24 The facemask has an adjustable anterior wire that can accommodate a downward and forward pull on the maxilla with elastics. To minimize the tipping of the palatal plane, the protraction elastics are attached near the maxillary canines with a downward and forward pull of 30 degrees from the occlusal plane. Maxillary protraction usually requires 300 to 600 g of force per side, depending on the age of the patient. Patients are instructed to wear the appliance for 12 hours per day.
Sutural expansion and/or protraction induce new bone growth by mechanically stretching the sutures. Clinically, it has been shown that maxillary expansion can disarticulate the maxilla to allow a more favorable forward movement of the maxilla.25–27 A well-disarticulated maxilla seems to be critical when using tooth-borne devices for orthopedic effects. A protocol of repetitive weekly alternate rapid maxillary expansion and constriction of the maxilla to disarticulate it without overexpanding has been proposed.28 Usually it requires 7 to 9 weeks to loosen the maxilla. This protocol was modified to treat cleft lip and cleft palate patients using maxillary protraction in conjunction with Class III elastics.29 The sutures were loosened by alternating weekly expansion and constriction for 8 weeks, a facemask was used at night to “pull” the maxilla forward, and Class III elastics were used during daytime to “hold” the result of the protraction.
Figure 14-3 shows an 8-year-old female patient who presented with a chief concern of “my bite is not right.” Clinically, she presented with a concave facial profile, obtuse nasolabial angle, deficient (black) maxilla, and relatively normal mandible. Intraorally, she had an anterior crossbite and crowding in the upper arch. The upper left and right permanent canines were blocked out due to crowding. The maxillary incisors were proclined and the mandibular incisors were retroclined, compensating for the skeletal malocclusion. There was no family history of mandibular prognathism (see Fig. 14-3, A–D).
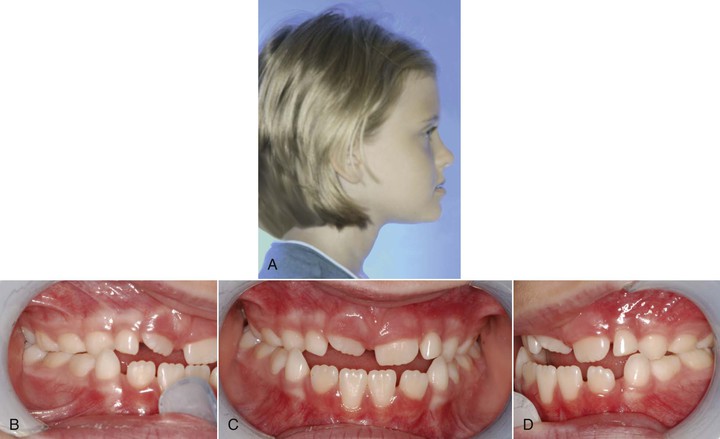
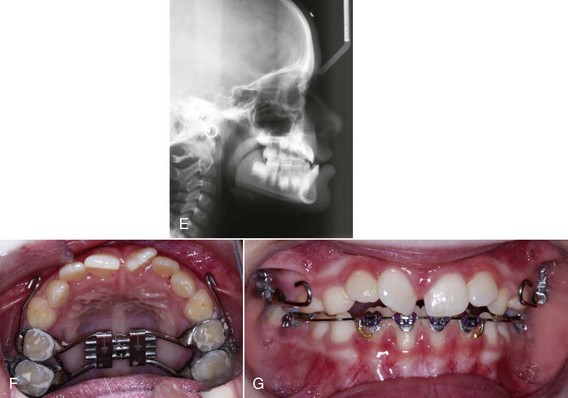
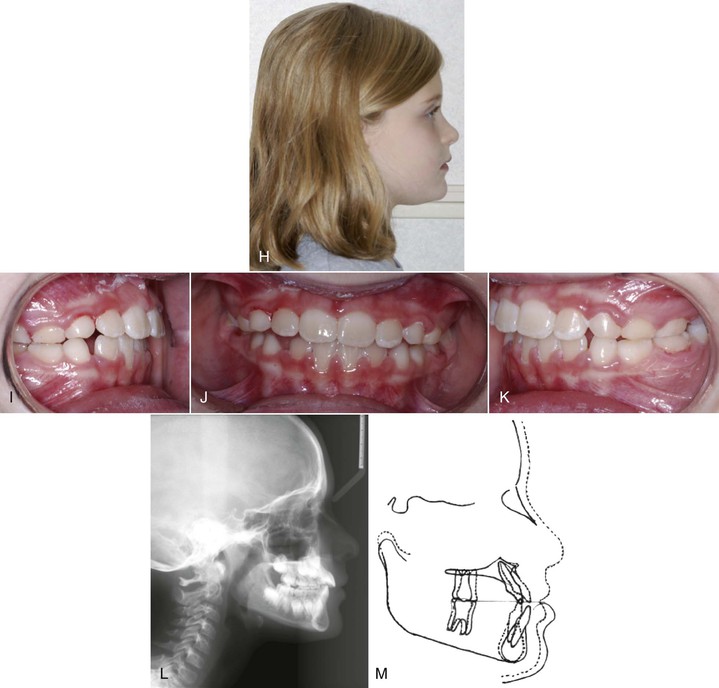
Figure 14-3 Pre-treatment (A) profile and (B–D) intraoral photographs of an 8-year-old patient who presented with a Class III malocclusion and a concave facial profile. E, Cephalometric radiograph shows a deficient maxilla and normal mandible. F and G, Patient was treated with the expansion and constriction protocol to loosen the facial sutures. This was followed by facemask treatment. Post-treatment (H) profile and (I–K) intraoral photographs show the improvement in overbite and overjet. L, Post-treatment cephalometric radiograph shows the improvement in skeletal relationship. M, Superimposition of pre-treatment and post-treatment radiographs shows forward movement of the maxilla and downward and backward rotation of the mandible, after facemask treatment.
The Hyrax RPE appliance was constructed by using bands on the posterior teeth. Bands were fitted on the upper deciduous second molars and on the upper permanent first molars. The bands were soldered to heavy wires (0.045-inch) that were connected to a jackscrew that centered along the midline of the maxillary palate. Bilaterally, a 0.045-inch wire was soldered to the buccal aspects of the molar bands and extended anteriorly to the canine area. This buccal wire had a curve at the canine area so that elastics could be used to connect the appliance to a protraction facemask. The alternate rapid maxillary expansion and constriction protocol was used to loosen the sutures that connect the maxilla to the surrounding bones via rapid expansion and contraction on an alternating weekly basis for 7 weeks.28 The maxilla was expanded or contracted 1-mm per day (two turns in the morning and two turns in the evening). The amount of expansion was checked after the first, second, and fifth week. The mobility of the maxilla was checked before proceeding to maxillary protraction. The maxilla could be clinically examined for mobility by holding the patient’s head with one hand and rocking the anterior segment of the maxilla up and down with the other hand.
The Petit protraction facemask (Ormco Corporation, Glendora, CA.) is a one-piece construction with adjustable forehead padding, an adjustable chin cup, and an adjustable anterior bar. The adjustable components of the protraction facemask and appropriate positioning of the anterior bar (to which elastics were attached to both right and left sides) allowed for proper positioning of the chin cup for comfort on both opening and closing of the mandible. To avoid an opening of the bite as the maxilla is protracted, the elastics were attached near the maxillary canines with a downward and forward pull of 30 degrees to the occlusal plane. A Correx gauge (Haag-Streit, Bern, Switzerland) was used to measure the elastic force between the expansion appliance and the facemask to ensure that approximately 450 g of force was generated on each side. The patient was instructed to wear the protraction facemask for 10 to 12 hours of nighttime wear. On the mandibular arch, bands were fitted on the mandibular first molars and brackets were placed on the mandibular four incisors. A 0.019-inch × 0.025-inch posted archwire with a stop loop in front of the mandibular first molar was placed so that the patient could wear Class III elastics during the day for 8 hours. Figure 14-3 shows the correction of the anterior crossbite after 4 months of maxillary protraction with the facemask at night and Class III elastics during the day. Superimposition of the pre-treatment and post-treatment radiographs shows a 4.5-mm forward movement of the A point. The patient was placed on retention with a Frankel III regulator for 1 year (see Fig. 14-3, E–M).
Treatment Timing
A question of clinical importance in maxillary protraction is when to start the facemask treatment. The main objective of early facemask treatment is to enhance forward displacement of the maxilla by sutural growth. Histological studies have shown that the midpalatal suture is broad and smooth during the “infantile” stage (8 to 10 years of age) and becomes more squamous and overlapping in the “juvenile” stage (10 to 13 years).30 Biologically, the circumaxillary sutures are smooth and broad before age 8 years and become more heavily interdigitated around puberty. These findings are related to observations in clinical studies that have shown that maxillary protraction is effective in the primary mixed as well as early permanent dentitions. Several studies have suggested that a greater degree of anterior maxillary displacement can be found when treatment is initiated in the primary or early mixed dentition. The optimal time to intervene in a Class III malocclusion is at the time of the initial eruption of the maxillary incisors. A positive overjet and overbite at the end of the facemask treatment appears to maintain the anterior occlusion.
An additional question worth addressing is whether the results of early protraction treatment can be sustained when subsequent mandibular growth occurs during the pubertal growth spurt. In a prospective clinical trial, protraction facemask treatment starting in the mixed dentition was found to be stable 2 years after the removal of the appliances.31 This probably resulted from overcorrection and the use of a functional appliance as retainer for 1 year. When these patients were followed for another 2 years, 15 of 20 patients maintained a positive overjet. In patients who relapsed to a negative overjet, the mandible outgrew the maxilla in the horizontal direction. When these patients were followed for another 4 years (8 years after treatment until about 17.5 years of age), 14 of 20 patients (67%) maintained a positive overjet. For the patients who relapsed into a reverse overjet, the mandible outgrew the maxilla by four times, compared with twice that in the stable group. These results suggest that in a random clinical trial when patients are followed until after completion of pubertal growth, two out of three patients (67%) will have a favorable outcome. About one-third of the patients might be candidates for orthognathic surgery later in life because of unfavorable growth pattern. Patients treated by protraction facemask either in the early mixed dentition or in the late mixed dentition and permanent dentition and followed up after a second phase of fixed appliance therapy demonstrated ongoing improvements in the former group but not in the latter group at the end of phase II treatment.32 Specifically, a 1.8-mm additional forward movement of the maxilla was noted in the early treatment group as compared to the control group. In the late mixed dentition group, no significant difference in forward movement of maxilla was found after puberty as compared to the control subjects.
Utility and Limitations
Clinically, anterior crossbite can be corrected with 3 to 4 months of maxillary expansion and protraction depending on the severity of the malocclusion. Improvement in overbite and molar relationship can be expected with an additional 4 to 6 months of treatment. In a prospective clinical trial, overjet correction was found to be the result of forward maxillary movement (31%), backward movement of the mandible (21%), labial movement of the maxillary incisors (28%), and lingual movement of the mandibular incisors (20%).31 Overcorrection of the overjet and molar relationship was highly recommended to anticipate unfavorable mandibular growth. Overbite was improved by eruption of the posterior teeth. The total facial height was increased by inferior movement of the maxilla and downward and backward rotation of the mandible. According to several clinical studies, the mean forward movement of the maxilla with 6 to 8 months of maxillary protraction is about 1- to 3-mm.21 A meta-analysis on the effectiveness of protraction facemask treatment found that the average change in Wits appraisal was 4- to 6-mm and the average horizontal A point movement was 1- to 3-mm. The average forward movement of the A point with 8 to 12 months of maxillary protraction was 2- to 4-mm. The increase in A point nasion B point (ANB) angle ranged from 0.9 to 4.4 degrees, with a mean value of 2.8 degrees. This is well over the expected growth changes for 1 year. Variability exists among individual subjects.
Chin Cap Appliance Therapy
Treatment Effects
The objective of early treatment with the use of a chin cap is to provide growth inhibition or to redirect mandibular growth. The short-term and long-term effects of chin cap have been reported extensively in the literature.33–37 The orthopedic effects of a chin cap on the mandible include downward and backward rotation of the mandible, closure of the gonial angle, shortening of the mandibular length, bending of the condylar neck, remodeling of the glenoid fossa, and opening of the cranial base angle. To date, there is no agreement in the literature as to whether chin cap may or may not inhibit the growth of the mandible long-term. However, Deguchi et al.36,37 reported that the long-term use of chin cap was effective in subjects with severe skeletal Class III abnormality.
To better understand the orthopedic effects of a chin cap, the treatment results of two sisters were compared (Fig. 14-4). The older sister, SH, received orthopedic treatment with an activator and a chin cap while the younger sister, SJ, did not receive any orthopedic treatment during the growing period. SH presented at the age of 6 years, 11 months with a significant reverse overjet while SJ presented at the age of 7 years, 9 months with a mild anterior crossbite. There was no difference in the cranial base length and angle for both sisters but SH had a larger maxilla and mandible and a more prognathic chin profile than SJ (Fig. 14-5).

Figure 14-4 Initial facial and intraoral photographs and cephalograms of two sisters. A, The older sister, SH, showed a more protruded lower lip and a more severe crossbite and deep bite. She began treatment at age 6 years, 11 months. B, The younger sister, SJ, showed a large lower facial height, a slight crossbite, and a shallow overbite. She began treatment at age 12.
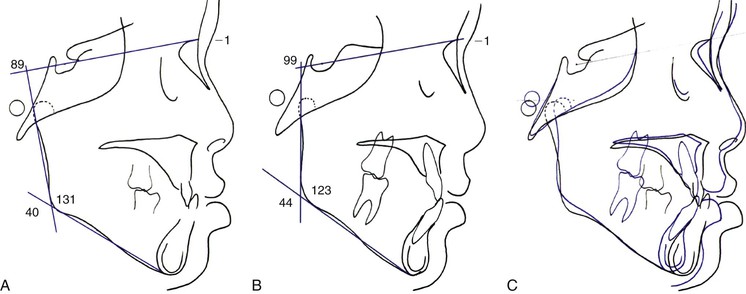
Figure 14-5 Initial cephalometric tracings and superimposition of the sisters. A, The older sister, SH, at the age of 6 years, 11 months: ANB angle –1, gonial angle 131, sella-nasion (SN) to mandibular plane angle 40, and SN to ramal angle 89. B, The younger sister, SJ, at the age of 7 years, 9 months: ANB angle –1, gonial angle 123, SN to mandibular plane angle 44, and SN to ramal angle 99. C, Pre-treatment cephalometric superimposition of the sisters. The black line is the older sister and the blue line is the younger sister. There is no difference in cranial base size and shape but the older sister shows a larger maxilla and mandible and a more prognathic chin than her younger sister.
SH received phase I orthopedic treatment together with partial fixed appliance to align her incisors. SJ was placed on observation until permanent dentition without any orthopedic treatment due to a shallow overbite and a long lower facial height. SJ received comprehensive orthodontic treatment at 12 years of age with extraction of the lower first premolars. Figure 14-6 shows the profile and dentition of the two sisters after treatment. SH showed a little lower lip protrusion whereas SJ showed a straight profile after extraction therapy.
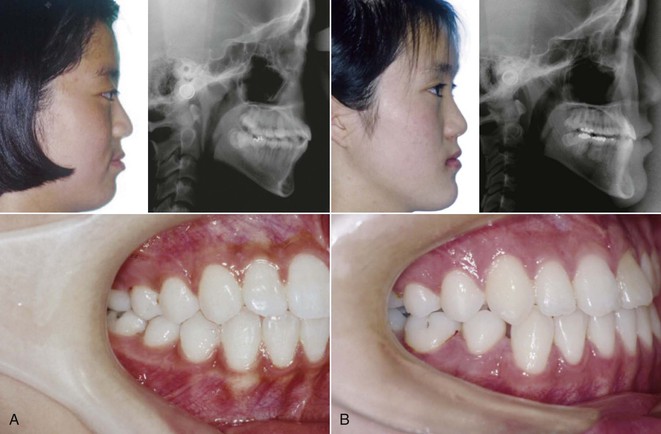
Figure 14-6 Post-treatment facial and intraoral photographs and cephalograms of two sisters. A, The older sister, SH, shows a slight protrusion of the lip and a Class I molar relation. B, The younger sister, SJ, shows a straight profile, a slightly prominent chin, and a full Class III molar relation (due to lower first premolar extraction).
The superimpositions of the pre-treatment and post-treatment lateral cephalograms showed quite distinct differences between the growth patterns of the two sisters in terms of the cranial base angle, mandibular position, and mandibular length and shape (Fig. 14-7). SH showed a downward and backward rotation of the mandible with the chin cap treatment while SJ showed a downward and forward growth of the mandible following the normal growth pattern. In addition, the posterior cranial base bending observed in SH could be explained by the application of chin cap force.
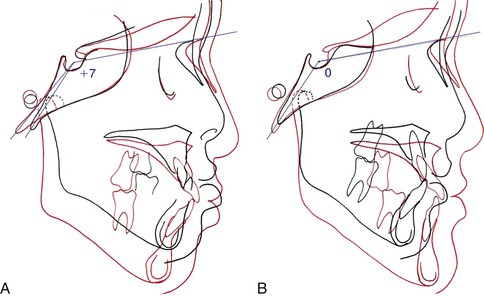
Figure 14-7 Cephalometric superimpositions of two sisters at pre-treatment and post-treatment. The superimpositions show distinct differences in mandibular position after treatment. The black line is pre-treatment and the red line is post-treatment. A, The older sister, SH, who had chin cap treatment, shows a downward and backward rotation of the mandible. B, The younger sister, SJ, who had no orthopedic treatment, shows a downward forward growth, following normal mandibular growth. In addition, posterior cranial base bending was observed in SH while no change was observed in SJ.
The orthopedic effects in SH can be seen more clearly by cephalometric superimpositions of the sisters at pre-treatment and post-treatment (Fig. 14-8). There was no difference in the position of the maxilla and upper face as well as the position of the anterior cranial base at pre-treatment. However, there were distinct changes in the position of the mandible and posterior cranial base at post-treatment. The results illustrate the typical effect of chin cap therapy.
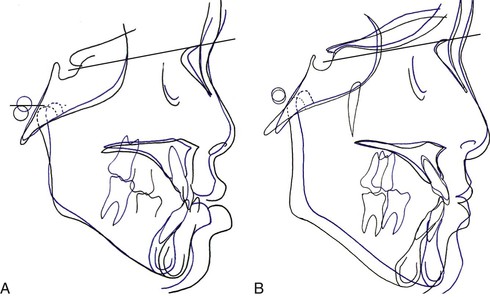
Figure 14-8 Cephalometric superimpositions of two sisters at pre-treatment and post-treatment. The black line is the older sister, SH, and the blue line is the younger sister, SJ. A, Cephalometric superimposition at pre-treatment. B, Cephalometric superimposition at post-treatment. In the pre-treatment superimposition, SH (black line) shows a protruded mandible and chin compared to SJ (blue line). However, in the post-treatment superimposition the mandible and chin of SH are behind those of SJ.
Limitations
The limitations of chin cap therapy in growing children with Class III malocclusion include long treatment time. Chin cap therapy is recommended to start early in childhood and continue until growth completion. However, it is almost impossible to obtain such cooperation from patients. Another limitation is that chin cap therapy shows various responses depending on the facial pattern of patients. Therefore it is important to select cases that will show good response to the chin cap.
Figure 14-9 shows a female patient age 5 years, 5 months who presented with an anterior crossbite in the primary dentition. Cephalometric analysis showed an increase in the vertical dimension and an obtuse gonial angle. The patient was treated with a chin cap and an activator at that time. Retrospectively, early orthopedic treatment in Class III patients with hyperdivergent growth pattern is not recommended. Another unfavorable decision that was made at that time was the removal of the four first premolars to obtain proper occlusion. Therefore proper occlusal interdigitation was never achieved due to the continuous growth of the mandible. The growth discrepancy was explained to the parents and the patient accepted orthognathic surgery as the definitive treatment (Fig. 14-10).
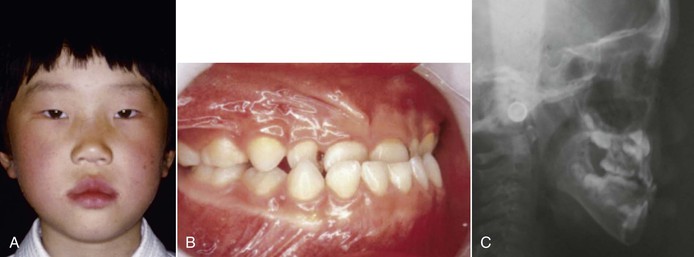
Figure 14-9 Initial (A) facial and (B) intraoral photographs and (C) cephalogram of a girl age 5 years, 5 months. ANB –0.5, gonial angle 142, and Frankfurt Mandibular Plane Angle (FMA) 39.
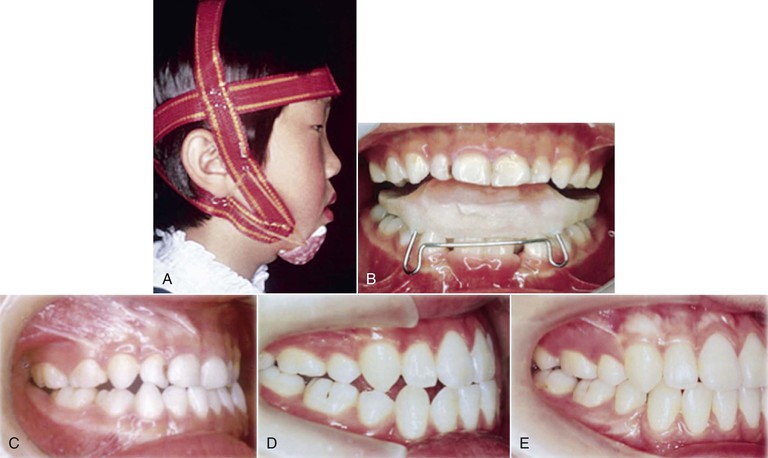
Figure 14-10 A–C, At age 5 years, phase I treatment was performed with activator and chin cap treatment. D, At age 15 years, after phase II treatment with four first premolar extractions. E, At age 19 years, orthognathic surgery was performed because of late mandibular growth.
Two lessons can be learned from the treatment of this patient. One is that the length of treatment is too long. Despite the long orthodontic treatment, surgery is still inevitable. The other lesson is that chin cap therapy tends to increase the lower facial height. The mandible actually grew forward after the termination of chin cap therapy (Fig. 14-11). Therefore chin cap treatment is not recommended for patients with hyperdivergent growth pattern. The changes from initial to post-treatment show tremendous growth of the mandible and large vertical growth of the mandible (Fig. 14-12). These results show that individual growth of the mandible cannot be predicted.
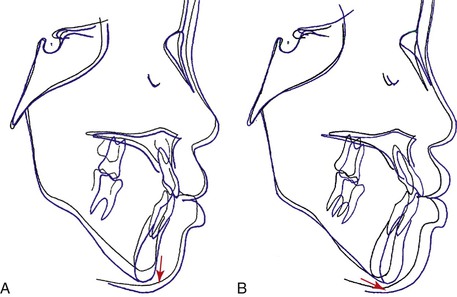
Figure 14-11 Cephalometric superimpositions of treatment progress. A, Mandibular changes during chin cap therapy. The black line is before chin cap therapy at age 6 years, 5 months and the blue line is after chin cap therapy at age 8 years, 1 month. B, Mandibular changes after stopping chin cap therapy. The black line is just after chin cap therapy at age 8 years, 1 month and the blue line is after growth without chin cap therapy at age 10 years, 1 month. Note the changes in mandibular growth direction between parts A and B.
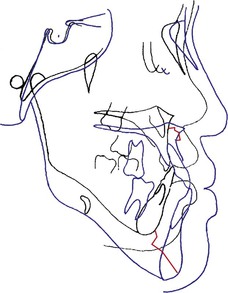
Figure 14-12 Cephalometric changes until the completion of growth. The black line is the initial stage at age 5 years and the blue line is after completion of growth at age 19 years. Note the great growth changes in the vertical dimension of the mandible. The red line indicates the changes of the A point and the gnathion during the observed period.
Removable Functional Appliance Therapy
Treatment Effects of Frankel III Regulator
The Frankel III regulator (FRIII) has been used to treat young Class III patients with mild maxillary skeletal deficiency. This appliance is usually used during early mixed dentition when the maxillary incisors are erupting. The treatment effects of FRIII include a more forward movement of maxillary skeletal and dental landmarks as well as a backward rotation or repositioning of the mandible combined with an increase in lower anterior facial height.38–41 Occlusal changes have also been noted, including proclination of maxillary incisors and lingual tipping of lower incisors. The FRIII looks quite bulky to insert in a child’s mouth. However, clinical experience shows that it is a very acceptable and comfortable appliance for treatment in young patients. Most children have no resistance to wearing the FRIII for a long time. As well, the FRIII could be a good retention appliance after facemask therapy. Figures 14-13 to 14-16 illustrate a typical Class III malocclusion treated with the FRIII.
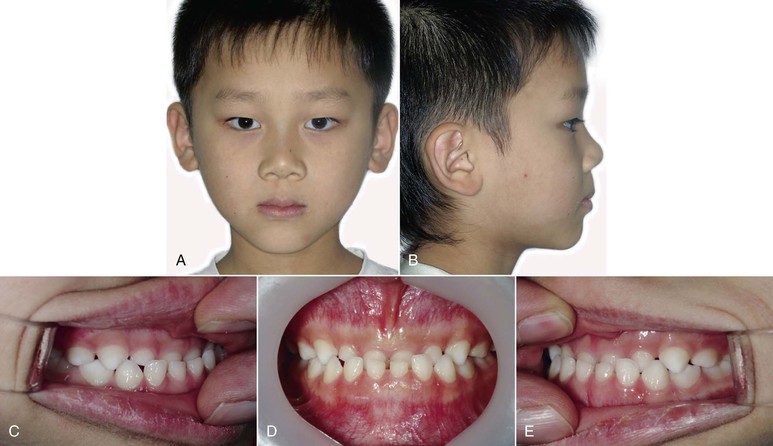
Figure 14-13 Initial (A and B) facial and (C–E) intraoral photographs of patient who presented with an anterior crossbite in the primary dentition. He was age 5 years, 4 months at first visit. ANB 0.4, Frankfurt Mandibular Plane Angle (FMA) 30, and gonial angle 130.

Figure 14-14 Photographs of treatment progress. A–C, After 6 months of using Class III activator, (D) the Frankel III regulator (FRIII) was delivered. E–G, Results after 17 months of FRIII.

Figure 14-15 A and B, Facial and (C–E) intraoral photographs at age 9 years, 8 months. The Frankel III regulator (FRIII) was stopped and the patient was observed until growth completion.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses