14
Soft Tissue Reconstruction
INTRODUCTION
It is critical to understand the potential complications associated with soft tissue reconstruction of the head and neck. This allows the surgeon to anticipate untoward events and take proper action to manage them or help prevent their occurrence. Complications in soft tissue reconstruction can be divided in two general categories: those involving the recipient site and those involving the donor site. Recipient site complications include total or partial flap necrosis, infection, fistula formation, suture line dehiscence, and hematoma or seroma formation. Donor site complications are similar and can include hematoma or seroma formation, infection, poor healing as well as other specific complications based upon the particular donor site. This chapter will discuss complications associated with commonly used myocutaneous flaps and several specific free flaps, and general prevention and management of these complications.
COMPLICATIONS IN PEDICLED SOFT TISSUE FLAPS
Pectoralis Major Myocutaneous Flap
The pectoralis major myocutaneuous flap (PMMF) has traditionally been one of the primary reconstructive options for the oral cavity, oropharynx, and cutaneous head and neck defects. It can be used with a cutaneous skin island or as a myofascial flap by itself. While its popularity has diminished over the past two decades with the widespread use and reliability of microvascular free flaps, the PMMF still plays an important role in head and neck reconstruction. The utilization of this flap is now important for salvage procedures after free flap failure, as muscle bulk for coverage of the great vessels of the neck, and in circumstances where microsurgical reconstruction is contraindicated or expertise is not available.
The overall complication rate for the PMMF has been reported to be as high as 44% to 63%.1–5 The majority of complications are considered minor, and conservative local wound care is often sufficient to resolve most of these minor complications.1 Wound dehiscence, flap edge necrosis, local infection, seromas, hematomas, donor site complications, and fistula formation are all possible minor complications. These complications are not unique to the PMMF and can be experienced with any method of reconstruction, particularly in the medically compromised, malnourished, and generally less than ideal surgical head and neck cancer patient.1
Although overall complication rates are high, most studies show a relatively low major complication rate with the PMMF ranging from 2.4% to 4%.1,6,7 Complete necrosis or greater than 25% partial necrosis of the flap are two possible major complications [Figs. 14.1(a), (b)]. Improved cutaneous paddle survival can be achieved by designing the skin paddle to remain over the pectoralis major muscle and minimizing its extension over the anterior rectus sheath (Fig. 14.2), careful dissection around the skin paddle without the use of monopolar cautery, and securing the skin paddle to the underlying muscle and fascia with temporary sutures.7
Fig. 14.1. (a) Complete flap loss of a free radial forearm free flap lining a right mandibular defect. (b) Partial flap loss of a pectoralis major myocutaneous flap lining the left preauricular region.
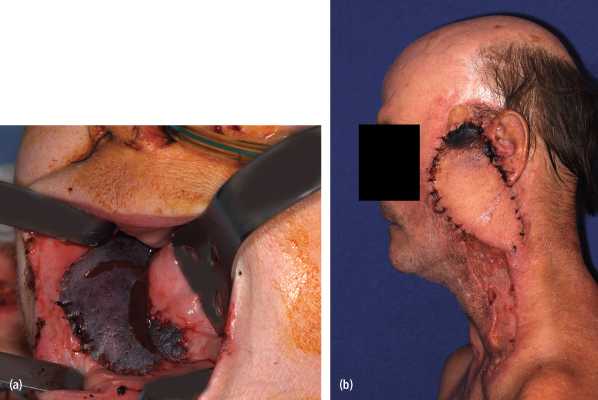
Fig. 14.2. Extension of skin paddle harvest over the rectus sheath (arrow) resulting in partial flap loss
[refer to Fig. 14.1(b)].

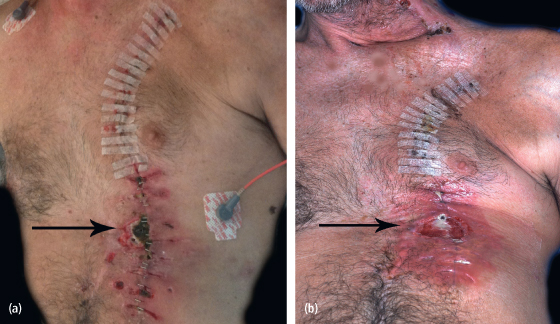
Depending on the size of the skin paddle that is required for the defect, primary closure of the pectoralis major flap may not be possible. This can be a more likely issue in very thin, male patients. A split-thickness skin graft may be necessary for closure of these donor sites. This is preferred over having wound breakdown later owing to primary closure with excessive tension [(Figs. 14.3(a), (b)].8
Fig. 14.3. (a) Donor site wound breakdown (arrow) owing to primary closure with tension. (b) Donor site wound after staple removal and debridement of necrotic tissue.
Submental Island Flap
The submental island flap is a viable reconstructive option for head and neck defects. Its cervical location assures good color and texture match for facial reconstruction. This flap is based on the submental artery, a consistent branch of the facial artery; venous drainage is through the submandibular vein into the facial vein.9,10 Dissection of the pedicle allows for good mobility of the flap. This flap can also be harvested as a reverse-flow flap with dependence on the angular artery for its blood flow.11 One study comparing the two patterns of submental flaps showed a success rate of 95% and 94.4% for the submental artery island flap and the reverse submental artery island flap, respectively.
Complications reported with this flap include venous drainage disruptions, partial or complete flap loss, hematoma formation under the flap, and marginal mandibular nerve injury.12 In one series, six of the nine cases experienced venous drainage disruption after raising the flap, but this did not cause flap loss.9 This was overcome in 4 to 5 days without any interventions.
Sterne et al. described the use of the submental island flap in 12 patients for intraoral reconstruction.12 One patient experienced partial flap loss, one a complete flap loss, one formed a hematoma under the flap, and two patients experienced a marginal mandibular nerve injury. To address the issue of nerve injury, Sterne et al. recommend that identification of the marginal mandibular nerve and preserving it before raising the flap may help prevent inadvertent damage to the nerve. Others advocate staying close to the posterior aspect of the platysma from the angle of the mandible to the midbody area when incising the ipsilateral upper limit of the flap. This will adequately protect the nerve and make it unnecessary to identify the nerve.13
Paramedian Forehead Flap
The forehead skin is acknowledged as an ideal donor site with which to resurface the nose due to its good color and texture match, as well as its favorable anatomic location. The paramedian forehead flap is thus a commonly used flap for nasal reconstruction. Complications associated with the paramedian forehead flap are rare, as the superficial axial blood supply provides for robust vascularity.
The excellent vascularity of this flap makes distal flap necrosis unusual and markedly reduces the risk of infection. This characteristic of the paramedian forehead flap also accounts for its most common complication, namely, hematoma formation. Often, the distal aspect of the flap is stripped of its muscle and subcutaneous tissue and has a propensity to bleed postoperatively.14 The potential dead space between the thinned flap and the underlying nasal defect is an area where hematoma formation can occur. To avoid this complication, much attention is given to achieving hemostasis over the entire area of the raw surface of the flap. Compression dressings applied with several bolster sutures passing full thickness through the flap to the nasal passage and back again may be helpful if bleeding is significant.14 However, bolster dressings are not used routinely as they may impair circulation to the distal part of the flap.
COMPLICATIONS IN MICROVASCULAR FREE FLAPS
Microvascular free tissue transfer (MFTT) after tumor extirpation or trauma is extremely reliable in achieving successful reconstruction of the head and neck. Foremost of the advantages of MFTT is the ability to tailor the donor flap to the specific needs of the ablative site. For example, a thin and pliable radial forearm flap would be ideal for a defect of the floor of the mouth or tongue, whereas the muscular bulk and large skin paddle of a rectus abdominus flap may be better suited for total glossectomy or maxillectomy defects. The pedicled flaps described earlier in this chapter are less suitable for defects that require either extreme bulk of tissue or very thin, pliable, and mobile tissue.
Due to the increased operating time and need for technical expertise, MFTT is often perceived as being a less reliable and more costly procedure than rotational flap reconstruction. However, several studies that compared MFTT to rotational flaps for reconstruction of the head and neck have suggested that this may not be true. Brown et al. showed that the risk of postoperative complications in patients who underwent free flap reconstruction was not significantly greater than those matched patients who received pedicled flap reconstruction.15 Their data suggested a trend toward shorter intensive care unit (ICU) and overall hospital stays with MFTT, although the differences were not statistically significant. In addition, several reviews identified the pectoralis major myocutaneous flap as having a higher risk of major postoperative complications such as fistula formation, flap loss, infection, and hematoma compared with radial forearm or rectus abdominus flaps.16,17
The disadvantages of MFTT include the technical demands on the surgical team, operating room staff, anesthesiology, and the ICU. The initial anesthetic time for MFTT is longer than for nonmicrovascular reconstructions, but studies have shown that the overall cost, length of hospital and ICU stay, and incidence of complications is not significantly increased with MFTT.15,18 The potential for total flap loss is also a distinct disadvantage of MFTT. Even the most experienced microsurgeons will have failures, usually due to thrombosis. However, as mentioned previously, the radial forearm and the rectus abdominus flaps have shown lower incidence of flap loss than the pectoralis major myocutaneous flap.16,17 Several large studies have shown a 0.8% to 2.9% incidence of free flap failure and a 3% incidence of partial flap necrosis.19,20 The current state of MFTT has evolved from a radical, last-resort procedure with a high failure rate to the first and most reliable choice in many types of soft tissue reconstruction of the head and neck.
Hypercoagulable states are the only true contraindications to MFTT (Table 14.1).21 This includes diseases such as polycythemia, thrombocytosis, and possibly sickle cell anemia. The risk of thrombosis in these conditions is too high to justify MFTT. Patients taking the antiestrogen medication tamoxifen for prevention or treatment of breast cancer should be taken off this medication prior to surgery due to its known thrombogenic activity.22 Also, smokers should be encouraged to stop at least 1 week prior to surgery for similar reasons, in addition to risk for decreased flap perfusion and overall impaired wound healing.
Table 14.1. Hypercoagulable States
| INHERITED | ACQUIRED |
| Antithrombin III deficiency | Prolonged immobilization |
| Protein C deficiency | Pregnancy |
| Protein S deficiency | Surgery/trauma |
| Activated protein C resistance | Oral contraceptives/antiestrogens |
| Factor V Leiden | Homocystinuria |
| Dysfibrinogenemia | Vitamin K deficiency |
| Plasminogen activator deficiency | Disseminated intravascular coagulation |
| Plasminogen deficiency | Smoking |
| Factor XII deficiency | Nephrotic syndrome |
| Polycythemia | L-asparaginase |
| Thrombocytosis | Diabetes mellitus |
| Sickle cell anemia | Hyperlipidemia |
| Heparin cofactor II deficiency | Malignancy |
| Lupus anticoagulant | |
| Anticardiolipin antibody |
Age has not been shown to be a significant risk factor for postoperative complications with MFTT. Although studies have implied that advanced age has a greater risk for prolonged hospital stay, medical complication, and in-hospital death,23,24 others have shown no significant difference in complications following major head and neck reconstructive surgery.25 However, advanced age is associated with atherosclerotic disease and increased vessel fragility, which may pose a specific potential, though not absolute, problem in MFTT. Atherosclerosis is most problematic when evaluating the patient for harvest of the fibula flap due to concerns of distal lower extremity vessel perfusion. However, the actual effect of atherosclerosis on a microvascular anastomosis is not known. Diabetes mellitus can predispose patients to microvascular disease and atherosclerosis, which may result in delayed wound healing, infection, and possible flap loss.
Finally, pediatric patients may have very small caliber vessels that will make anastomosis difficult and less reliable, especially when the vessels are less than 1 mm in diameter.
The postoperative management of patients receiving MFTT is as important as the intraoperative MFTT technique. Protocols vary by institution and are not based on scientific evidence of efficacy but rather surgeon preference and experience. However, in order to minimize postoperative complications, certain standards should be applied to all free flap reconstructions regardless of site.
Pressure on the microvascular pedicle should be avoided at all times. In head and neck reconstruction, circumferential ties or straps such as those for tracheostomies or oxygen tents can easily compress the vessels in the neck. Similarly, kinking or undue tension on the vessels must be avoided, especially during the immediate postoperative period. The position of the neck that optimizes vessel geometry should be strictly maintained. This position can be sustained by using postoperative sedation with ventilator support. A paralytic agent can also be added to this pharmacologic management. It is the authors’ preference not to sedate most patients in the postoperative period as long as the patient is able understand and follow instructions to maintain a neutral head position.
Hemodynamics should be maintained as close to normal limits as possible. Avoiding extreme hyper- or hypotension is crucial to preventing hematoma formation while maintaining perfusion of the flap. A balance in the oxygen-carrying capacity of blood and blood viscosity must also be achieved. Although little scientific evidence exists, a hematocrit of 28% to 30% is generally accepted as the desired goal for the immediate postoperative period.
Flap monitoring protocols vary drastically between institutions. Although many modalities of monitoring flaps are currently available, with most oral and maxillofacial reconstructions, the skin paddle is readily examinable and its clinical appearance is the current standard for flap monitoring (Fig. 14.4). The parameters evaluated include color, capillary refill, flap turgor, and warmth. The frequency of serial postoperative evaluations of flaps also varies by institution, from every 1 hour to every 4 hours. The frequency is based on the fact that the time between the onset of a thrombotic event and its recognition may be critical to the flap’s salvage.26 In pig skin flaps, this critical time is reported as 7 hours.27 After 8–12 hours it may not be possible to reestablish the flap’s circulation.28
Fig. 14.4. Early postoperative appearance of healthy skin paddle of mandibular reconstruction. Notice natural skin color and texture, minimal swelling. This flap would be soft, warm, and have good capillary refill.
(From Kim D, and Ghali GE. “Postablative reconstruction techniques for oral cancer.” Oral and Maxillofacial Surgery Clinics of North America, Vol. 18 No. 4, Elsevier, Nov. 2006, 573–604.)

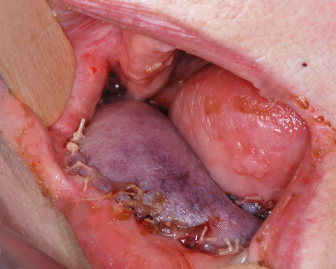
Possibly the most commonly used adjunct to the clinical exam is the pin-prick test. A 25-gauge needle is used at the center of the skin paddle, and the rapidity, color, and amount of blood return is evaluated. A healthy flap will bleed bright red blood after a slight delay (within 1–3 seconds). Rapid return of dark-colored blood, combined with an ecchymotic skin paddle, suggests venous insufficiency (Fig. 14.5). The blood consistency of a venous congested flap has been compared with crankcase fluid. Finally, no blood return, with a flap that is cool to the touch with a pale color, suggests arterial thrombosis. Although this widely used exam is subject to much interobserver error, it can be a valuable aid to the clinical assessment.
Fig. 14.5. Radial forearm flap on postoperative day 3 showing signs of venous congestion. Note the presence of significant flap edema and ecchymotic appearance of the skin. A pin-prick test on this flap would result in rapid return of dark colored blood.
The next most commonly used modality in postoperative flap monitoring is the handheld surface Doppler probe. The practical utilization of the Doppler probe is mainly for confirmation of arterial flow, but its ability to confirm venous outflow has been proposed.29 Observance of a change in the character of the “phases” of the Doppler signal may help the clinician identify the impending failure of a flap. However, because thrombotic complications are usually venous in nature, the utility of this modality is severely limite/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


