Prevention of Dental Disease
Prenatal Counseling
For more than a century, the medical profession has recognized the importance of providing prenatal counseling and care to expectant mothers. Oral health care is important to the expectant mother as well. Studies report a strong association between the presence of maternal periodontitis and both preeclampsia and preterm births.1–5 There is also strong evidence that relates the oral levels of Streptococcus mutans in mothers to the caries activity experienced by their offspring.6 Such studies have renewed the interest in the oral health of the expectant woman.7 Dental professionals can make important contribution in this primary preventive effort by attending to women’s oral health during pregnancy and providing prenatal counseling related to infant oral health and oral development.
Although many oral health counseling programs have been developed in recent years, the goals of the programs are similar (Box 14-1). Regardless of the setting, time allotted, and staff involved, the program should be individualized to the greatest extent possible and should provide parents with information about the development of oral structures and functions, dental disease processes, and recommended preventive measures. In addition, the program should provide information on the importance of the mother’s diet and health-related behaviors during pregnancy (including the effects of drugs, tobacco, and alcohol), the importance of maternal oral health care during pregnancy, and recommended scheduling of maternal dental treatment (Box 14-2).
Knowing that there is a strong relationship between S. mutans levels in expectant mothers and the caries experience of their offspring, prenatal counseling should include a discussion on interventions that can disrupt the transmission of these virulent organisms.6 Interventions that can suppress maternal S. mutans reservoirs include dietary changes that reduce the frequency of simple carbohydrate consumption, chemotherapeutic applications such as topical fluorides and topical chlorhexidine, and the elimination of existing caries by either tooth restoration or extraction.8 In addition, evidence suggests that xylitol-containing products can significantly reduce maternal levels of S. mutans.9–11 Xylitol is a sugar alcohol that is used as a low-calorie sugar substitute. It is available in a variety of forms that include gums, mints, nasal sprays, toothpastes and gels, xylitol-containing beverages and snacks, and wipes (Figure 14-1), which are promoted to cleanse the oral cavity of infants. Consumption of 6 to 10 g of xylitol per day at three different time intervals has been shown to reduce levels of S. mutans in adults.12 Reducing levels in mothers can help delay the colonization of their offspring which in turn has the potential to reduce the caries activity in these children.10,13
The timing and sequence of eruption of teeth should be discussed during prenatal counseling. Variations are common and a frequent source of parental anxiety. Teething should also be mentioned because it most likely will be the first postnatal oral issue that parents confront. Teething is a natural phenomenon that usually occurs with little or no associated problems. Nevertheless, some infants exhibit signs of systemic distress including a slight rise in body temperature (typically lower than 101° F), diarrhea, dehydration, increased salivation, skin eruptions, and gastrointestinal disturbances.14–16 Increased fluid consumption, a nonaspirin analgesic, and palliative care consisting of the use of teething rings to apply cold and pressure to the affected areas generally reduce the symptoms and result in a happier infant.17 Lancing of tissues is usually not indicated. If symptoms persist for more than 24 hours or if body temperature exceeds 101° F, a physician should be consulted to rule out the possibility of other common diseases and conditions of infancy.
Prenatal counseling programs should also provide guidelines for the parents about the timing of the first professional dental visit. In the past, guidelines have recommended that children without symptoms of disease be scheduled for their first dental examination beginning at age 3 years. More recently, however, professional guidelines have incorporated the importance of earlier attention to oral health during infancy, particularly for children at elevated risk for the development of dental caries.18–20 Programs designed to provide comprehensive preventive measures now stress the importance of initiating professional visits with a risk assessment within 6 months of the eruption of a child’s first tooth or no later than age 12 months (Figure 14-2).21
Several educational programs are available that provide comprehensive and practical information designed to assist health professionals and families to more effectively promote the health and well-being of children and adolescents. The American Academy of Pediatrics, Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents is one such program.22 These programs not only stress the importance of the early initial exam to assess the infant’s risk for dental disease but they also provide anticipatory guidance information and guidelines to help establish follow-up appointments based on the outcomes of the caries risk assessment.23
Caries Risk Assessment
Another innovation in designing preventive programs is based on the concept of the caries risk assessment as detailed in Chapter 13. The risk of developing dental disease varies among children and over time for each child. Assessing each child’s risk for common dental diseases and identifying specific risk factors on a regular basis allows the practitioner to more effectively individualize oral health supervision and preventive measures.
Risk assessments for dental caries based on a single risk indicator are unlikely to reliably differentiate between those at high and low risk because caries is a complex disease process. Accordingly, various multifactorial models have been developed. The risk assessment protocol developed by the American Academy of Pediatric Dentistry, as detailed in Chapter 13 and presented in Table 13-1 and Table 13-2, is one such model. Based on the risk level, the clinician can personalize and initiate a comprehensive preventive program for the child. Risk status should be reassessed periodically to detect changes in the child’s clinical, environmental, and general health conditions. The American Academy of Pediatrics also endorses the early risk assessment as well as the establishment of a dental home by 12 months of age.18
Establishing a Dental Home
All children should have a place where they can receive appropriate health care provided by physicians, dentists, and other allied health professionals. The health provider should know the child and parent and should establish a level of trust and responsibility with the family. Doing so allows for optimal cooperation and opens avenues of communication between the family and the provider. Most parents establish such an environment early with respect to medical care for their infants and toddlers. To complement the medical home, all infants and toddlers should have an established dental home as well. The concept of a dental home was introduced in 2002 as a means to address the epidemic of early childhood caries as well as other oral health issues that pertained to the pediatric patient.24 The proposal that the first dental visit should take place earlier than 3 years of age, which had been customary, was a major change in philosophy. This recommendation was based on the fact that while dental caries had been declining in the permanent dentition for decades, the rates of early childhood caries had been static and had even began to worsen in more recent years.25 It was recognized that by 3 years of age, the damage from caries had already occurred and dental professionals were forced into surgical modes of treatment that included restorations and extractions as opposed to preventive measures of treatment. The benefits of early initial exams have been supported by studies which have shown that early enrollment of children into oral health care programs increases parental compliance with preventive measures,26 reduces caries activity,27–29 and results in lower expenses for dental care over time.30
The dental home should include accessible facilities and comprehensive oral health services geared to the needs of children and their families. Whether this dental home is located in a private practice, a community health center, or at the neighborhood hospital, it should be supervised by dentists trained in primary pediatric care. By establishing a dental home early, parents will be appropriately counseled during the early infant years and have a facility to contact immediately in case of an orofacial traumatic injury. The dental home should provide all of the services listed in Box 14-3. Today’s children should have not only established medical homes but also established dental homes as part of their comprehensive health care program.24,31
Fluoride Administration
Rationale
Significant reductions in the prevalence of dental caries have been documented in older children and adults in the United States and other countries over the past several decades.32 Although the reason for this decline is unknown, most experts include increased availability of fluorides as one of the primary contributing factors. In spite of these advances, caries remains a relatively common yet largely preventable disease of childhood. Because of the importance of fluoride in this regard, the contemporary dental practitioner should understand the basis for using the many available forms of fluoride.
Systemic Fluorides
Water Fluoridation
Water fluoridation remains the cornerstone of any sound caries prevention program. It is not only the most effective means of reducing caries, but remains the most cost-effective, cost-saving, convenient, and reliable method of providing the benefits of fluoride to the general population because it does not depend on individual compliance.33,34 Early studies documented caries reductions of 40% to 50% in the primary dentition and 50% to 65% in the permanent dentition of children and adolescents exposed to fluoridated water from birth.35 More recent studies have reported that the mean decayed-missing-filled surfaces (dmfs) of children with continuous residence in fluoridated areas was about 18% lower than that of children with no exposure. When corrected to remove children that have been exposed to topical or supplemental fluorides, the mean dmfs was 25% lower in the group exposed continuously to water fluoridation.36
Many water supplies contain significant levels of natural fluoride, especially in the midwestern and southwestern sections of the country. Although it is relatively expensive to remove existing fluoride from a community water source, it is relatively inexpensive to add fluoride to a community water source. Numerous fluoride-deficient community water supplies have been artificially fluoridated at a cost of less than $0.50 per person, depending on the size of the community. In 2008, over 195 million U.S. individuals (72.4% of the population served by public water systems) received optimally fluoridated water. These data reflect an increase from 162 million (65.8%) reported in 2000.37,38
Dietary Fluoride Supplements
The use of bottled and processed waters for drinking and cooking has become increasingly popular in recent years. The total U.S. consumption of bottled water was estimated at more than 8.5 billion gallons in 2009 (up from 4.7 billion in 2000).39,40 Consumers are turning to these water sources as alternatives to tap water, which they believe is contaminated with microorganisms, pesticides, herbicides, industrial waste, and heavy metals. The fluoride content of these bottled waters generally has been found to exhibit wide variability, usually below optimal concentrations.41–45 Regulations presently do not require bottled water manufacturers to list the fluoride concentration on the label. Though optimally fluoridated bottled water is commercially available, it is infrequently used by consumers. Hence, dentists need to be aware of the bottled water products readily available in their community and be prepared to obtain fluoride analyses when necessary. Furthermore, all parents, including those who reside in areas where water is fluoridated, should be questioned about the sources of fluid in their infant’s diet and should realize that fluoride supplements are advisable for at-risk children who consume very little fluoridated water.
Fluoride supplements can be as effective as fluoridated water in preventing caries46–48; however, their effectiveness depends largely on the degree of parental compliance. Supplements are commercially available in liquid and tablet forms, both with and without vitamins. The fluoride-vitamin formulations are not inherently superior to supplements without vitamins in terms of reducing caries. Unfortunately, the parents of children at high risk of developing caries often fail to comply with fluoride supplement regimens.49 The combination of fluoride and vitamins may improve parental compliance, thereby providing greater benefits.50 These fluoride-vitamin combinations should only be recommended for those children determined to be deficient in their fluoride consumption. Prescribing fluoride-vitamin combinations to the child already using an optimally fluoridated water source exposes that/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Outline
Outline Box 14-1
Box 14-1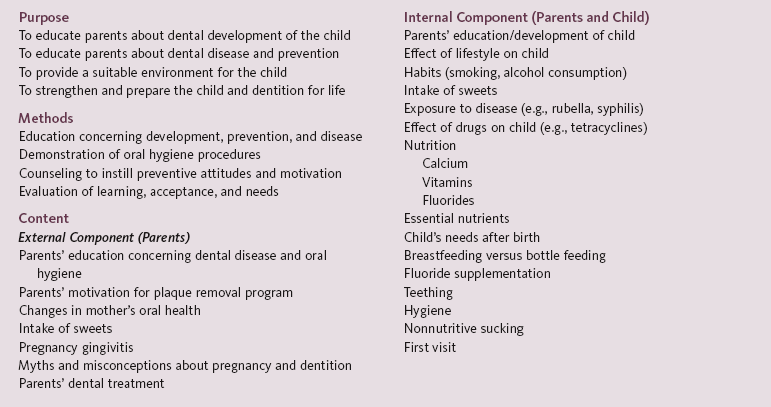
 Box 14-2
Box 14-2
 FIGURE 14-1
FIGURE 14-1
 FIGURE 14-2
FIGURE 14-2 Box 14-3
Box 14-3