Orthodontic diagnosis and treatment in the mixed dentition
John Fricker, Om P Kharbanda and Julia Dando

Introduction
The primary aim of orthodontic assessment in a growing child is to differentiate between a developing normal occlusion and a potential malocclusion, including any abnormal growth of the face and function of the stomatognathic system. It is essential to have a sound understanding of facial growth and dental development, and the ability to recognize the rate and direction of facial and dental growth. Many situations of apparent malocclusion in the mixed dentition are actually manifestation of the normal process of dental and facial development. Minor incisor irregularities, spacing and ectopic eruption of teeth, which may show up during the mixed dentition, could self-correct with growth and development.
Correction of dental arch irregularities, occlusal and jaw relation abnormalities and elimination of functional interferences may be classified as preventive or interceptive. The term ‘preventive orthodontics’ implies steps undertaken for elimination of factors that may lead to malocclusion in an otherwise normally developing dentition.
‘Interceptive orthodontics’ implies that corrective measures may be necessary to intercept a potential irregularity from progressing into a more severe malocclusion. Neither the appliances used nor the treatment itself should interfere with the often rapid changes in eruption of permanent teeth and the dynamic nature of occlusal adjustment. It is important to understand that even when such procedures are carried out, a majority of these children will go on to require some further treatment in the permanent dentition.
Orthodontic assessment of a child
An orthodontic assessment in common with other specialties, must include a good history, a thorough clinical examination and any relevant investigations. The information gathered leads to a diagnosis, which in turn allows treatment planning. This topic is covered in detail in Chapter 1. Additional points relevant to aid orthodontic diagnosis, however, will now be discussed.
The child should be assessed for skeletal and dental problems and abnormalities of functions of the stomatognathic system. Clinical assessment is performed in all the three dimensions of space, i.e. vertical, anteroposterior and transverse.
Skeletal classification
This describes the anteroposterior relationship between the maxilla and mandible relative to the cranial base:
Dental relationships
Dental relationships are recorded with the teeth in occlusion. It describes the anteroposterior relationship of the upper and lower molars according to Angle’s classification and the anteroposterior incisor relationship according to the British Standards Institute classification (1983). Angle’s classification of malocclusion is based on the relationship of the upper and lower first permanent molars.
Molar relationship (Figure 14.1)
Incisor relationship (Figure 14.2)
• Class II Division 1 (proclined upper incisors).
• Class II Division 2 (retroclined upper incisors).
• Class III cross-bite of the anterior segment or negative over jet.
Vertical assessment includes normal or abnormal vertical overlap of the incisors, i.e. normal, deep or open bite. Transverse assessment should include any cross-bite or scissors-bite of the buccal segments of the dental arches.
Complicating factors in any malocclusion
These include:
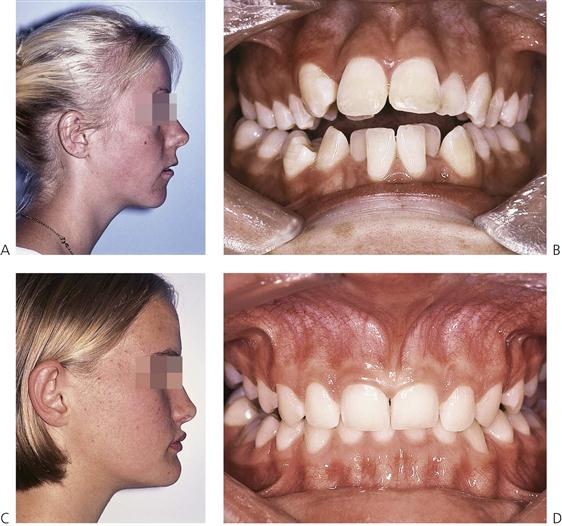
Intra-arch problems (Figure 14.3)
Inter-arch problems
Orthodontic examination
Extra-oral
The physical status of the child should be included here, and if relevant, height and weight should be recorded on a standard growth chart. It is essential to determine if the face of the child is also growing normally. The face is examined with the child sitting upright. This is important because the mandibular rest position will change, if lying back.
Frontal view
Lateral view (Figure 14.4)
• Profile – convex/straight/concave.
• Skeletal pattern – Class I, II, III.
• Nose – small/normal/prominent.
• Chin – recessive/normal/prominent.
• Lip position – competent (closed), incompetent (apart).
• Labiomental sulcus – normal/deep.
• Extreme types are vertical growers (with FMA angle >32°) and horizontal growers (with FMA angle of <20°). Growth direction is an important consideration in treatment planning (Figure 14.5).
Intra-oral
A record should be made of:
• Number of teeth present radiographically and intra-orally.
• Tooth quality and any existing restorations or active caries.
• Level of oral hygiene and assessment of gingival health.
• Assessment of crowding/spacing in both arches.
• Overjet, overbite, canine and molar relationships.
• Anterior or posterior cross-bites and any associated functional shift into occlusion.
• Dental centre lines in relation to each other (upper to lower).
• In relation to the facial midline (upper to face and lower to face).
• Condition of the oral soft tissues
• Any other pathology such as an epulis.
• Tongue position: at rest and during swallowing.
It is important to identify any deviation of the mandible during opening and closing into full intercuspal occlusion. Often the underlying cause is interference from an erupting tooth leading to either functional forward or lateral shift that demands early treatment to restore the balance in the temporomandibular joint (TMJ).
Investigations
These are determined by the findings at examination.
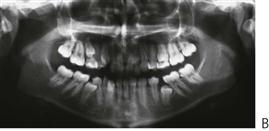
• Posteroanterior (PA) cephalogram – for transverse discrepancies or asymmetry.
• Anterior occlusal films – only for location of impacted canines, supernumeraries, or ectopic teeth.
• 3-dimensional CT may be required for evaluation of exact location of impacted or supernumerary teeth that are otherwise difficult to locate with standard 2D radiographs. Cone beam CT (CBCT) is becoming increasingly popular, since radiation doses are much less than CT (see Chapter 11).
Evaluation of crowding
In the permanent dentition, it is easy to assess the amount of crowding by taking measurements directly from study models. Treatment will depend on the severity of the problem and may involve arch lengthening or extractions. In the mixed dentition, however, a prediction of future crowding is necessary.
Mixed dentition analysis
The purpose of a mixed dentition analysis is to determine the space available in the dental arch for the permanent successors to erupt. To complete this analysis, it is necessary to first record the arch length and the mesiodistal widths of the mandibular permanent incisors.
Measurement of arch length
The conventional way to determine arch length is to measure directly from a set of study casts. Soft brass wire can be adapted from the mesial of the first permanent molar to follow the arch form around to the mesial of the contralateral first molar. The wire should be shaped to the ideal arch form and not follow any teeth out of alignment. Once the arch length has been determined, it is then necessary to estimate the space required for the permanent successors. Mesiodistal dimensions of erupted teeth up to second premolars can be obtained directly from a study cast. Unerupted teeth can be measured by one of two methods:
Both methods are based on the high correlation between the crown measurements of the permanent mandibular incisors and the combined sizes of two premolars and permanent canines. Thus, it is possible to forecast the amount of space required for the unerupted teeth and to plan interceptive and/or preventive space management requirements.
The difference in values between arch length and tooth size will indicate the amount of crowding or spacing present.
Summary
At the end of diagnosis, a clinician should have gathered the following information:
• Growth pattern – normal, Class I, Class II, Class III.
• Growth trend – horizontal, vertical.
• Sequence and stage of eruption of teeth.
• Number of teeth missing or supernumeraries.
• The dental arch relations – cross-bites.
• Amount of crowding and spacing.
• Digit sucking/thumb sucking habit.
• Pattern of respiration, i.e. normal breathing or mouth breathing.
• Is the child likely to grow normally or would he/she benefit from orthodontic intervention?
Crowding and space management in the mixed dentition
Space management can minimize the development of crowding in the permanent dentition. It essentially involves:
• Space maintenance following the premature loss of primary molars.
• Utilization of the leeway space by placement of holding arches.
Space maintenance
The best space maintenance treatment is the preservation of the primary molars until natural exfoliation. Although dental health education and improved caries prevention have lowered the number of children who develop malocclusion because of premature loss of primary teeth, it is still one of the most common controllable causes of malocclusion.
When a primary second molar is lost prematurely due to caries or to the ectopic eruption of the first permanent molar, the first permanent molar will drift mesially. This is most pronounced in the maxilla with a more rapid shift of the molar and causing a Class II malocclusion. The earlier the loss of the second primary molar and the less the root development of the permanent molar, the greater will be the amount of bodily mesial shift of the permanent molar.
Factors to consider for placement of space maintainers
Placement of a space maintainer requires care of the appliance and oral hygiene maintenance. A child with poor oral hygiene and high caries risk is not the ideal case for such appliance therapy. Before a decision is made to provide a space maintainer, it is often essential to critically evaluate its merits, the need and the benefit it would provide to the development of normal occlusion.
Anterior teeth
Types of space maintainer
Removable
Removable space maintainers have shortcomings similar to all removable appliances:
A removable space maintainer that is only worn at night is often sufficient to hold space and prevent the mesial drift of permanent molars. Night-only wearing of the appliance also reduces the risk of loss or breakage by the patient. The appliance should be washed and inserted in place before going to bed, then removed, washed and placed in a safe place when not worn. Hawley’s appliance is a typical example.
Utilization of the leeway space
Regaining space
Within an arch, space may need to be regained when migration of permanent teeth has already occurred following the loss of adjacent deciduous teeth (Figure 14.7). Furthermore, space maintenance would then be needed until the permanent successor erupted. In the maxilla, this would intercept a developing Class II, dental relationship secondary to mesial migration and rotation of the first permanent molar. In the mandible, it could prevent a mild dental Class III relationship by uprighting tipped lower first permanent molars. In individuals with a developing skeletal discrepancy, the dental correction would have no effect on the underlying skeletal problem.
In general, tooth movement is slower in cases with severe horizontal growth pattern (low FMPA). Conversely, it is rapid in vertical growers, and space loss can occur very quickly. Early fitting of a space maintainer will prevent space loss. If space is to be regained, it is essential that the mechanics should not extrude the teeth at all.
Radiographs and study models are essential aids in assessing space needs. It is important to note whether teeth have moved bodily or have tipped into the space. Tipping can be easier to resolve than bodily tooth movement. Radiographic examination should also locate the permanent second molars and establish space available for distalization of the first permanent molars.
Appliances used to regain space
• Removable appliances – Acrylic cervical occipital appliance (ACCO appliance).
An ACCO appliance (Figure 14.8) is comprised of a palatal acrylic plate with an anterior bite platform to disclude the posterior teeth, allowing the first permanent molar to move freely. Retention is obtained via Adams clasps on the first premolars or deciduous molars and a labial bow across the permanent incisors. The bow should be supported with a band of acrylic across the labial surfaces of the incisors to increase the anchorage for the finger springs against the mesial surface of the molars to be distalized. These are most successful in the maxillary arch, where there is a dental and skeletal Class I pattern with normal vertical proportions and the regaining of space is by way of uprighting the first permanent molar.
Timed extraction of teeth to resolve intra-arch crowding
The total amount of arch length deficiency is the key to planning of timed extractions. For this to be beneficial, a cephalometric analysis should show the child to be growing within a normal pattern and that all the permanent teeth are present radiographically and in the normal order of eruption.
Extraction of deciduous canines
Serial extraction
The purpose of serial extraction is to encourage the early eruption of the first premolars ahead of the permanent canines and should only be considered where there is an arch discrepancy of >4 mm. Serial extraction is usually limited to the upper arch as serial extractions in the lower arch usually results in lingual collapse of the lower anterior segment.
Contraindications
Serial extraction should not be performed in the following circumstances:
Treatment stages in serial extraction
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses