Chapter 14
Management of Complications and Emergencies
Aim
This chapter describes the complications and emergencies that can occur in the minor oral surgery patient.
Outcome
After reading this chapter you should understand the management of complications and emergencies in patients having minor oral surgery.
Introduction
Early recognition and prompt management of complications and emergencies distinguishes the experienced surgical practitioner from the novice. Perhaps of most significance, however, is the ability to identify potential difficulties at the time of patient assessment (see chapter 2).
Complications are usually the result of local surgical difficulties, whilst emergencies arise when generalised conditions threaten patient welfare.
Complications in Minor Oral Surgery
A complication may be defined as an unwanted event, rendering a surgical procedure more difficult, intricate or involved than previously expected. As in most clinical situations, forethought and preparation beforehand lessen their incidence.
It is helpful to divide complications into those arising during the immediate pre-operative phase, those occurring during surgery itself, and finally those that present post-operatively (Table 14-1).
| Complications in minor oral surgery | |
| PRE-OPERATIVE PROBLEMS | |
| (A) Anatomical |
– Trismus Small mouth Dental crowding Misplaced teeth |
| (B) Anaesthetic |
– Difficulty or failure to achieve anaesthesia |
| (C) Patient cooperation |
– Anxious patient Inadequate sedation |
| OPERATIVE DIFFICULTIES | |
| (A) At surgical site |
– Resistance to tooth extraction Tooth fracture Alveolar bone fracture Fracture of maxillary tuberosity Creation of oro-antral communication Haemorrhage Tooth/Root displacement Damage to instruments Failure to complete procedure |
| (B) At adjacent sites |
– Extraction of wrong tooth Damage to adjacent teeth/restorations Damage to oro-facial soft tissues Inhaled or swallowed tooth/roots Fractured mandible TMJ trauma/dislocation |
| POST-OPERATIVE PROBLEMS | |
| (A) Pain |
– Tissue damage Acute alveolar osteitis (dry socket) Osteomyelitis TMJ injury |
| (B) Swelling |
– Oedema Haematoma Infection |
| (C) Bleeding |
– Upon completion of surgery Reactionary haemorrhage Secondary haemorrhage |
| (D) Trismus |
– TMJ injury Muscular spasm Haematoma |
Pre-Operative Problems
Limited access to the mouth creates obvious difficulties for minor oral surgery, and it may be better to postpone elective procedures when such conditions exist. Similarly, problems in achieving local anaesthesia or anxious patients with poor cooperation or unsuccessful sedation may require referral for hospital management. It is essential to take the medical history into consideration and adequately prepare the patient. Collapse of the patient during or immediately after giving a local anaesthetic is well recognised and should be managed promptly. Vasovagal syncope can be pre-empted in the nervous patient. It should be countered by ensuring that an adequate meal has been eaten prior to the appointment and by injecting the local anaesthetic with the patient in the supine position.
Operative Difficulties
Complications during extractions
These include:
-
failure of pain control
-
extraction of the wrong tooth
-
fracture of the crown or root
-
displaced tooth or root
-
fracture of the bone
-
damage to other structures
-
broken instruments
-
haemorrhage.
Failure of pain control
Pain during the extraction may be encountered and can be very disturbing both for the patient and the clinician. Collateral supply should be considered once the regional blockade of the sensory supply has been established. Periodontal ligament and intraosseous anaesthesia can be useful in some circumstances (Fig 14-1).
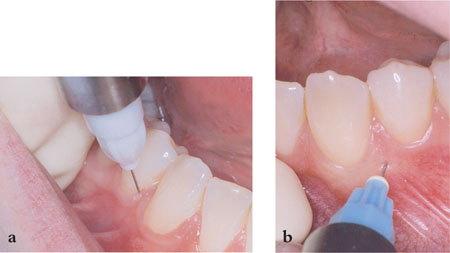
Fig 14-1 Periodontal ligament (a), and intraosseous (b) techniques are useful adjuncts when conventional approaches fail to provide complete anaesthesia.
Extraction of the wrong tooth
This can occur if the clinician does not establish with the patient exactly which tooth is to be extracted. It is most likely to involve teeth of a similar morphology, such as premolars. The patient must be informed and reimplantation may be considered. However, the prognosis is not always favourable. In any case the planned extraction should be completed unless the tooth has been symptom-free.
Fracture of the crown or root
Whilst experienced clinicians often recognise and deal with abnormal resistance during tooth removal, crown or root fractures do occur at times due to pre-existing caries or restorations. It may also occur if the clinician relaxes the apical pressure on the tooth whilst moving the tooth buccally. In addition it may be the result of an abnormal root pattern. This should not be regarded as a major complication. The removal of the remainder of the tooth may require a surgical approach as described in Chapters 5 and 6. An assessment of the remaining fragment should be made concerning its size, proximity to important structures and the morbidity associated with its removal. Small apical fragments may be left in situ, as injudicious instrumentation may displace the remnant into the inferior alveolar canal or the maxillary sinus. If a decision is made to leave a root in situ (e.g. a third molar apex intimately related to the inferior alveolar nerve) the patient should be fully informed and an appropriate entry made in the case notes. The clinician should be prepared to proceed to a surgical approach if symptoms develop.
Displaced tooth or root
Displacement of teeth or roots may occur due to inappropriate elevation, and dental tissues may be forced into th/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


