Gingival Inflammation
Joseph P. Fiorellini, David M. Kim and Panagiota G. Stathopoulou
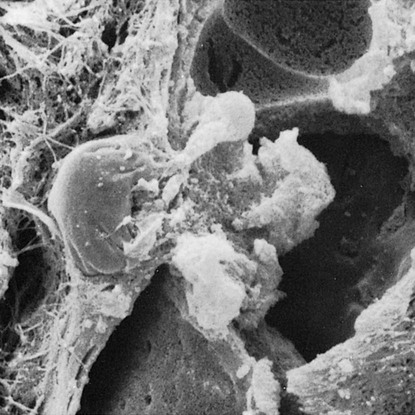
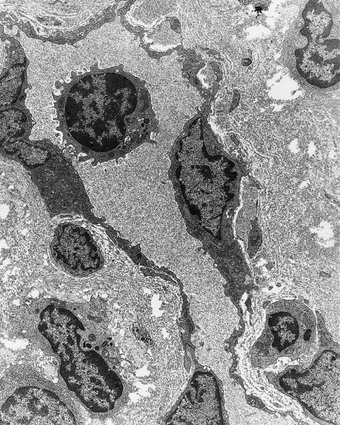
These organisms are capable of synthesizing products (e.g., collagenase, hyaluronidase, protease, chondroitin sulfatase, endotoxin) that cause damage to epithelial and connective tissue cells as well as to intercellular constituents such as collagen, ground substance, and glycocalyx (cell coat). The resultant widening of the spaces between the junctional epithelial cells during early gingivitis may permit injurious agents derived from bacteria or bacteria themselves to gain access to the connective tissue.10,44,48 Microbial products activate monocytes and macrophages to produce vasoactive substances such as prostaglandin E2, interferon, tumor necrosis factor, and interleukin-1.25,38 In addition, interleukin-1β alters the properties of gingival fibroblasts by delaying their death via mechanism-blocking apoptosis. This stabilizes the gingival fibroblast population during inflammation.54
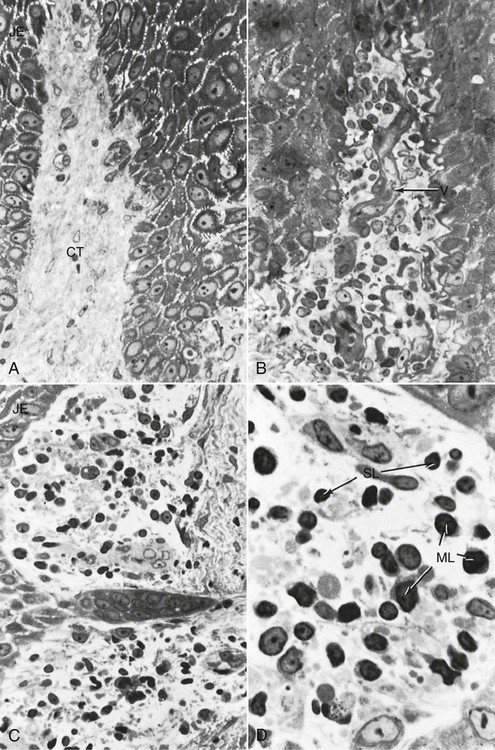
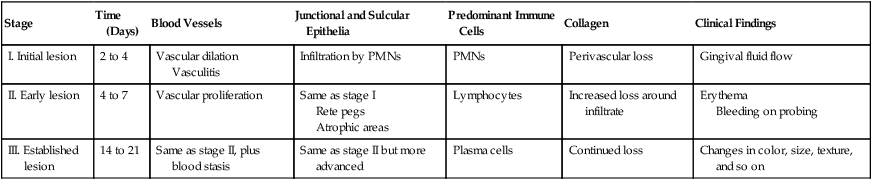
Morphologic and functional changes in the gingiva during plaque accumulation have been thoroughly investigated, especially in beagle dogs and humans.36 A useful framework for the organization and consideration of these data has been devised on the basis of histopathologic, radiographic, and ultrastructural features and biochemical measurements.37,39 The sequence of events that culminates in clinically apparent gingivitis is categorized as the initial, early, and established stages of disease, with periodontitis designated as the advanced stage38 (Table 14-1). One stage evolves into the next, with no clear-cut dividing lines.
TABLE 14-1
| Stage | Time (Days) | Blood Vessels | Junctional and Sulcular Epithelia | Predominant Immune Cells | Collagen | Clinical Findings |
| I. Initial lesion | 2 to 4 | Vascular dilation Vasculitis |
Infiltration by PMNs | PMNs | Perivascular loss | Gingival fluid flow |
| II. Early lesion | 4 to 7 | Vascular proliferation | Same as stage I Rete pegs Atrophic areas |
Lymphocytes | Increased loss around infiltrate | Erythema Bleeding on probing |
| III. Established lesion | 14 to 21 | Same as stage II, plus blood stasis | Same as stage II but more advanced | Plasma cells | Continued loss | Changes in color, size, texture, and so on |
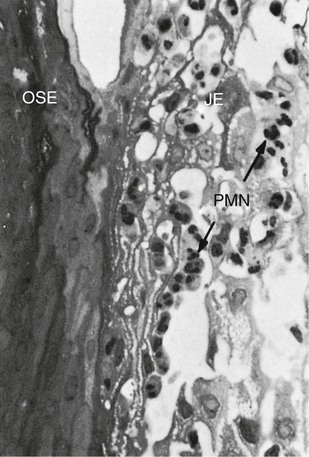
Despite extensive research, we still cannot distinguish definitively between normal gingival tissue and the initial stage of gingivitis.36 Most biopsies of clinically normal human gingiva contain inflammatory cells; these consist predominantly of T cells, with very few B cells or plasma cells.36,49,50 These cells do not create tissue damage, but they appear to be important in the day-to-day host response to bacteria and other substances to which the gingiva is exposed.36 Therefore, under normal conditions, a constant stream of neutrophils is migrating from the vessels of the gingival plexus through the junctional epithelium, to the gingival margin, and into the gingival sulcus and the oral cavity.43
Stage I Gingival Inflammation: The Initial Lesion
The first manifestations of gingival inflammation are vascular changes that consist of dilated capillaries and increased blood flow. These initial inflammatory changes occur in response to the microbial activation of resident leukocytes and the subsequent stimulation of endothelial cells. Clinically, this initial response of the gingiva to bacterial plaque (i.e., subclinical gingivitis26) is not apparent.
However, these findings are not accompanied by manifestations of tissue damage that are perceptible at the light microscopic or ultrastructural level; they do not form an infiltrate, and their presence is not considered to indicate pathologic change.36
Subtle changes can also be detected in the junctional epithelium and the perivascular connective tissue at this early stage. For example, the perivascular connective tissue matrix becomes altered, and there is exudation and deposition of fibrin in the affected area.36 In addition, lymphocytes soon begin to accumulate (see Figure 14-2, D). The increase in the migration of leukocytes and their accumulation within the gingival sulcus may be correlated with an increase in the flow of gingival fluid into the sulcus.4
Stage II Gingival Inflammation: The Early Lesion
The early lesion evolves from the initial lesion within about 1 week after the beginning of plaque accumulation.35,41 Clinically, the early lesion may appear as early gingivitis, and it overlaps with and evolves from the initial lesion with no clear-cut dividing line. As time goes on, clinical signs of erythema may appear, m/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses