14
Endodontic Retreatment
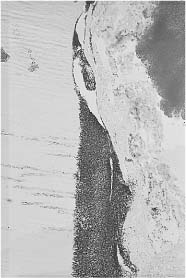
As discussed above, the results of endodontic treatment are influenced by a number of biological and technical factors like diagnosis, root canal morphology, root canal instrumentation and obturation, and complications during the treatment. Still it should be understood that the underlying reason for failure usually is infection and the influence of bacteria and bacterial components and products on the periapical tissues. Thus, in a study of 60 root filled teeth which were extracted because of apical periodontitis, bacteria were found in the root canal of all teeth (Fig. 14.1). This finding stresses the importance of obturating the root canal bacteria-tight at all levels and also that the root filling should be protected by a solid, well-fitting coronal restoration. The lack of healing after endodontic treatment may also be due to extra-radicular infection that might not respond to conventional treament.
The goal of endodontic retreatment is the same as for primary treatment, namely to obtain a bacteria-free tooth with a bacteria-tight root filling and an adequate coronal restoration so that healing may occur and reinfection is prevented. About two-thirds of retreatment cases will heal after renewed conventional treatment. Of the latter, one-third of which mostly comprises treatment-resistant or refractory cases, again about two-thirds will heal following surgical–endodontic treatment. In addition, the success rate in this group may be improved by adequate systemic antibiotic treatment, preferably following identification of the infecting bacteria.
Fig 14.1 Inadequately root filled tooth with large bacterial colony and plaque between root filling material and root canal wall.
Indications for Retreatment
Root Filled Teeth with Apical Periodontitis
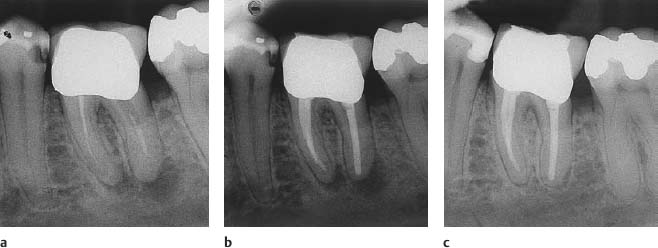
Epidemiological studies have shown a clear correlation between the technical standard of the root filling and the periapical condition of root filled teeth. Thus, whereas 80–90% of teeth with adequate root fillings have a normal apical periodontium, only about 50% of teeth with inadequate root fillings have a normal periapex. There is no reason to expect that healing of an apical periodontitis occurs if the root filling does not provide an adequate seal of the root canal. Teeth with a technically inadequate root filling and a persisting apical periodontitis should therefore be retreated (Fig. 14.2).
If the root filling, as seen radiographically, is technically adequate, an apical periodontitis will usually resolve within a period of 2–3 months to 3–4 years. It is unlikely that a lesion that has not healed after 4 years will heal in the future. Persisting infection will have to be suspected and if pathways of infection like a vertical fracture or a deep periodontal pocket are not diagnosed, chances are that there is coronal leakage or an extra-radicular infection and the tooth should be retreated endodontically. If treatment failure is diagnosed sooner than at the 4-year control, the retreatment should of course be carried out as soon as the failure is evident.
Teeth without apical periodontitis that appear to have been treated technically adequately may also fail, and an apical periodontitis may develop (Fig. 6.14). These teeth should be retreated immediately.
Fig 14.2
a Radiograph of a mandibular molar with inadequate root filling and asymptomatic apical periodontitis.
b The tooth has been retreated conservatively through the crown.
c Complete periapical repair is evident at the 6-month control.
Root Filled Teeth with Normal Apical Periodontium
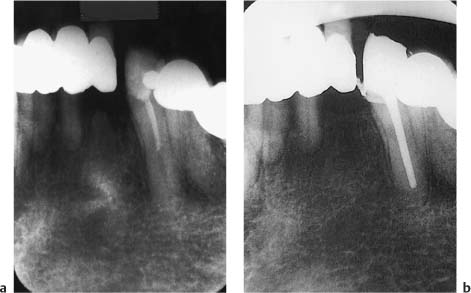
Teeth with inadequate root fillings but without clinical or radiographic signs of periapical inflammation represent a problem group. A certain percentage of these teeth will fail every year, and in reality all teeth in this group are candidates for retreatment (Fig. 14.3). However, there is no immediate urgency in treating these teeth that have no signs of disease and the treatment can be done over time and if possible when it is convenient for the patient. Often it will be practical to carry out the endodontic retreatment in conjunction with renewing a coronal restoration. Clearly the patient has to be made aware of the situation, and regular clinical and radiographic controls are necessary.
Fig. 14.3
a Radiograph of a mandibular canine with root filling material in the coronal half of the canal. No periapical inflammation is evident.
b The tooth is retreated endodontically in conjunction with renewing the coronal restoration.
Retreatment
Before beg/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses