13
Orthodontically related root resorption
INTRODUCTION
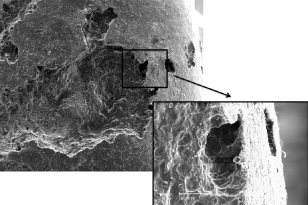
Orthodontic treatment can be associated with a number of iatrogenic changes including decalcification, periodontal problems and root resorption. Orthodontically induced inflammatory root resorption (OIIRR) is a common unavoidable adverse effect of treatment which is the focus of this chapter. It is a pathological process that results in a loss of substance from mineralised cementum and dentine1,2 (Figure 13.1) due to the removal of hyalinised tissue during orthodontic tooth movement.3,4 Fortunately, a reparative process in the periodontium commences when the applied orthodontic force is discontinued or reduced below a certain level.5,6 This healing process can occur as early as the first week of retention following orthodontic treatment and increases over time.7–9 There are biological and mechanical factors that influence the severity of OIIRR. Mechanical causative factors can be controlled by the clinician to minimise the adverse effect of OIIRR and allow initiation of repair.
Figure 13.1 Scanning Electron Microscopy of a root resorption crater.
INCIDENCE, DISTRIBUTION AND SEVERITY OF OIIRR
OIIRR occurs in almost all orthodontically treated individuals. However, significant root resorption following orthodontic treatment is a rare event. Lupi et al.10 radiographically investigated a sample of 88 ethnically diverse adults and showed that 15% of the teeth had resorption prior to orthodontic treatment. After 12 months of orthodontic treatment, the incidence of OIIRR increased to 73%. Two percent showed moderate to severe root resorption before treatment and 24.5% showed the same degree of severity after orthodontic treatment. More recently, Smale et al.11 showed that 24% of the teeth had root shortening, but only 3.6% had shortening of more than 2 mm.
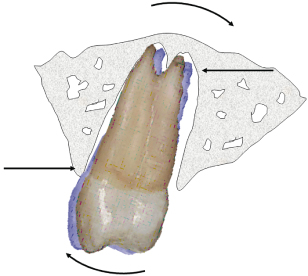
Generally, the distribution of root resorption is dictated by the pressure zone created by different types of tooth movement. Therefore, for tipping movement, it is usually found in the marginal and apical parts of the tooth.12 OIIRR tends to occur preferentially in the apical region because (Figure 13.2):
- Orthodontic tooth movement is not entirely translatory and the fulcrum is usually occlusal to the apical half of the root13
- The orientation of the periodontal fibres in the apical end is different which increases the stress in the region14
- More friable acellular cementum covers the apical third of the root, which can be easily injured in the case of trauma and concomitant vascular stasis.13–15
Figure 13.2 Majority of orthodontic movements are not translatory but tipping in nature, therefore, root resorption occurs at the apical part of the tooth root.
There are three levels of OIIRR severity:16
1. Cemental or surface resorption with remodelling
2. Dentinal resorption with repair
3. Circumferential apical root resorption.
Significant resorption of the root apex results in root shortening with no evidence of regeneration. However, with time, the sharp edges formed by resorption craters may be levelled. Surface reparation only occurs in the cemental layer.
RADIOGRAPHIC DIAGNOSIS OF OIIRR
Radiographs have been widely used to clinically diagnose OIIRR. The dental panoramic tomograph (DPT) provides an overall view of the dentition with a lower radiation dose than a full-mouth series of intraoral radiographs.17 However, due to the narrowness of the focal trough, the apices and palatal structures can be out of focus in the incisor region. Therefore, additional radiographs such as periapical radiographs or occlusographs may be needed to supplement the DPT. Sameshima and Asgarifar18 compared periapical radiographs with DPTs and found the amount of root resorption was exaggerated by 20% or more on a DPT. The paralleling technique for periapical radiography is preferable as it provides a geometrically accurate image, and, together with the use of a film holder and aiming device, radiographs can be standardised at two different time points. The two-dimensional nature of radiography limits its accuracy because buccal and lingual root defects are not detectable.19 With the advance of technology, cone-beam computed tomography will be more readily used in future root resorption studies. It will provide a more accurate three-dimensional image with a lower dosage of radiation, which can be used for qualitative and quantitative assessment.
PATHOGENESIS OF OIIRR
Orthodontic tooth movement is associated with local over-compression of the periodontal ligament (PDL), which results in hyalinisation. Resorption of the cementum occurs simultaneously with the removal of hyalinised tissue.5,20–22 Resorption starts at the periphery of the hyalinised periodontal membrane and is followed by resorption of surrounding root and bone surfaces4,23 and invasion of blood vessels.24 The resorption process propagates until no hyalinised tissue is present and/or the force level diminishes. The resorption crater expands the root surfaces involved and thereby indirectly decreases the pressure exerted through force application. Decompression alters the process to reverse and cementum reparative process begins. It has also been documented that OIIRR initiated 10–20 days after force onset12,21,25 continued even during extended retention periods of up to 1 year.7,8,26 The resorbing areas on a root surface may show signs of concurrent active resorption and repair.7,12
The cellular process of OIIRR involves three sequences of events in the periphery and main hyalinised zones.4,24 First, tartrate resistant acid phosphatase (TRAP)-negative mono-nucleated fibroblast-like cells initiate root resorption from the periphery of the main hyalinised zone by the nearest viable cells in the presence of adequate vascularity. Second, TRAP-positive multinucleated cells participate in the removal of main hyalinised tissue and resorption of the adjacent root structure. This phase commences only after a considerable amount of hyalinised tissue between alveolar bone and the root surface has been eliminated and continues even after the initial root resorption has terminated. The cells involved during this resorptive phase are derived from adjacent marrow spaces. Lastly, active root resorption continues to occur in areas of hyalinised tissue even after orthodontic force has ceased to be applied. Reparative processes start from the periphery of the resorption craters and extend to the central part.
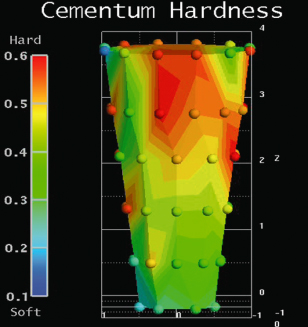
PHYSICAL PROPERTIES OF OIIRR CEMENTUM
Cementum at the cervical and middle thirds of the root has greater hardness and elastic modulus than that of the apical third27,28 (Figure 13.3). This is because of the variable mineral content of cellular and acellular cementum.29 Chutimanutskul et al.29 showed the hardness and elastic modulus of cementum were affected by the application of orthodontic forces whereby the mean hardness and elastic modulus of cementum was greater in the light force group than the heavy force group. The mean hardness and elastic modulus of cementum also gradually decreased from the cervical to apical regions.27,28
Figure 13.3 Cementum hardness distribution along the tooth root.
Rex et al.30 studied the mineral composition (calcium [Ca], phosphorus [P] and fluoride [F]) of human premolar cementum following the application of orthodontic forces. The results showed limited change in the mineral composition of cementum after the application of light force. There was a trend towards an increase in the Ca and P concentration of cementum at various areas of PDL compression. The application of heavy force caused a significant decrease in the Ca concentration of cementum at certain areas of PDL tension. Orthodontic force did not appear to influence the F concentrations in cementum.
FACTORS INFLUENCING THE DEGREE OF OIIRR
OIIRR can be influenced by a wide range of shared biological and or mechanical factors. Biological factors are directly related to the individual and can be genetic or environmental. Mechanical factors are attributed to the nature of the orthodontic appliance and could be controlled by both the clinician and the patient.
Biological Factors
Root resorption can occur in individuals without orthodontic treatment and is related to one’s tissue response and metabolic activity. The metabolic signals (e.g. hormones, body type and metabolic rate) influence the relationship between osteoblastic and osteoclastic activity which modifies cell metabolism, an individual’s reaction pattern to disease, trauma and ageing.5 Root resorption can vary among individuals and within the same person at different times.
Genetic Factors
Genetic influence on the susceptibility to root resorption remains controversial. Previously, a sib-pair model was used to investigate the genetic influence on root resorption and reported 70% heritability for resorption of maxillary incisor roots and the mesial and distal roots of the mandibular first molars. This accounted for approximately half of the total phenotypic variation.31 This meant that siblings experienced similar levels of OIIRR. A further study also revealed a familial association of OIIRR.32
One of the difficulties in assessing the genetic contribution to OIIRR is the ability to separate genetic factors from environmental factors such as orthodontic treatment.33 Ngan et al.33 investigated the genetic contribution to OIIRR by retrospectively assessing the pre- and post-treatment records of 16 monozygotic and 10 dizygotic twins. Each twin pair had the same malocclusion and the same type of appliance treatment with the same clinician. Panoramic radiograph tooth root measurements were used to obtain quantitative and qualitative estimates of concordance for OIIRR. The concordance estimate for root resorption in monozygotic twins was 44.9% for qualitative measurements and 49.2% for quantitative measurements. The concordance estimate for root resorption in dizygotic twins was 24.7% for qualitative measurements and 28.3% for quantitative measurements. The authors thus confirmed the presence of a genetic component to OIIRR. However, they advised that a larger sample was required before a model of heritability could be used to determine the components contributing to the variance.33
Ethnicity can also influence the susceptibility to OIIRR. Sameshima and Sinclair34 have found that Caucasians and Hispanics are more prone to OIIRR than people from the Far East.
Environmental Factors
- Asthma and allergy. An increased incidence of OIIRR, especially blunting of maxillary molars, has been found in patients with chronic asthma.35,36 This could be attributed to the close proximity of the roots to the inflamed maxillary sinus and/or the presence of inflammatory mediators in these patients. Allergy may increase the risk of OIIRR.36,37 Nishioka et al.38 investigated the association between excessive root resorption and immune system factors in a sample of Japanese orthodontic patients. The result showed that the incidence of allergy, asthma and root morphology abnormality was significantly higher in the root resorption group. Corticosteroids are commonly used to treat allergy, asthma, dermatitis and eczema. They have been shown to interfere with orthodontic tooth movement rate and tissue reaction in animal studies.39–42 Research of the effects of corticosteroids on orthodontic induced root resorption remains controversial. This could be due to different dosages of corticosteroids used and also different animal models studied. Verna et al.43 investigated the effect of acute and chronic corticosteroid treatment on OIIRR. The results showed more root resorption at the mesial coronal level in the acute treatment group than in the chronic treatment and control groups. The less resorption found in the chronic group may have been due to faster remodelling of bone, less hyalinisation and less remodelling of root tissue.
- Endocrine and hormone imbalance. Imbalance of the endocrine system due to hypothyroidism, hypopituitarism, hyperpituitarism, hyperparathyroidism,44 Paget’s disease45 and hypophospataemia46 is hypothesised to be related to OIIRR.44,47,48 Goldie and King49 reported an association with a decrease in OIIRR and secondary hyperparathyroidism. An excess of thyroid hormones, which increases bone turnover, have been found to reduce root resorption during orthodontic tooth displacement in a rat model.50 In contrast, hypothyroidism has been associated with increased root resorption in the absence of orthodontic load.51 Calcitonin can inhibit odontoclast activity.52 The action of calcitonin on osteoclasts occurs at later stages of osteoclast development and it inhibits the fusion of pre-osteoclasts to form mature multinucleated cells.
- Nutrition. Root resorption has been demonstrated in animals deprived of dietary calcium and vitamin D.44,48 Engstrom et al.44 found the experimental rat group that was fed with a diet deficient in calcium and vitamin D had hypocalcaemia, increased alkaline phosphatase activity and increased circulating parathyroid hormone when compared with the control group, which was fed with a normal diet. Orthodontic tooth movement produced greater and more rapid bone resorption and more severe OIIRR in the experimental group. The study also showed an increased number of osteoclasts in the PDL of the test group, which was suggested to be due to the increased parathyroid hormone levels.
- Drugs. Inhibition of cyclo-oxygenase and the subsequent production of prostaglandins by non-steroidal anti-inflammatory drugs (NSAIDs) can be useful in decreasing bone and root resorption. Villa et al.53 investigated the effect of nabumetone, a type of NSAID, on root resorption during intrusive orthodontic tooth movement and discovered less root resorption when patients received nabumetone, and the drug did not impede tooth movement. This was supported by Kameyama et al.,54 in whose study the rats were prescribed aspirin and which led to a suppression of root resorption caused by mechanical injury. Bisphosphonates are potent inhibitors of bone resorption that are widely used to treat osteoporosis. Bisphosphonates directly or indirectly induce apoptosis in osteoclasts, which plays a role in the inhibition of bone resorption.55 The effects on orthodontic tooth movement includes slower tooth movement and less root resorption due to decreased number of osteoclasts.56 Clodronate has also been shown to inhibit the production or release of pro-inflammatory molecules in macrophages and or osteoblastic cells.57–61
Age
The ageing process results in changes to the hard and soft tissues of the dentoalveolus. The PDL becomes less vascular, aplastic and narrow with age. The bone becomes more dense, avascular and aplastic and the thickness of cementum increases.6 Mirabella and Artun62 evaluated a large sample of adult patients for investigating the prevalence and severity of OIIRR in maxillary anterior teeth. Forty percent of the adults had one or more teeth with ≥2.5 mm resorption. This indicated that the sample of adults had a higher mean value of severely resorbed teeth per patient than the comparable group of adolescents which was 16.5%.63 On the other hand, Harris and Baker64 reported that 61% of adult patients had some degree of root resorption after orthodontic treatment, which was not significantly different from the 58% of adolescent patients experiencing root resorption in that same study.
Partially formed roots have been found to develop normally during orthodontic treatment and it has been suggested that teeth with open apices may be more resistant to OIIRR.63,65–67 Linge and Linge63 found less resorption in patients treated before the age of 11. They suggested that resorption could be avoided if tooth movement was completed before the roots were fully developed, before the age of 11.5 years, but treatment at this age may not be suitable for many patients.
Habits
A number of habits have been reported to result in an increased risk of OIIRR. Finger sucking beyond the age of 7 years has been suggested to be a risk factor.63 Nail biting,68 forward tongue pressure and tongue thrust63,69 have also been proposed to be linked to OIIRR. Long-term orthopaedic tongue thrusting forces that result in anterior open bite may promote root resorption,70 particularly when vertical elastics are used in an attempt to close open bites associated with tongue problems.
History of Trauma
Orthodontic tooth movement of a severely traumatised tooth may result in increased resorption.63,67,71–73 Linge and Linge67 found that teeth which had previously experienced trauma had an average loss of root structure after orthodontic movement of 1.07 mm compared with a loss of 0.64 mm in untraumatised teeth. However, Kjaer74 proposed that teeth with slight or moderate injuries may not have any greater tendency towards OIIRR than uninjured teeth. Malmgren72 suggested a waiting period of 1 year after a traumatic incident before the initiation of orthodontic tooth movement.
Cortical and Alveolar Bone
It has been suggested that OIIRR is amplified in dense alveolar bone compared with less dense alveolar bone, especially if there is an increased number of resorptive cells associated with the increased number of marrow spaces.6,22 Reitan22 proposed that a strong continuous force on low density alveolar bone caused an equivalent amount of OIIRR to that of a mild continuous force on high density alveolar bone.
Kaley and Phillips75 identified the risk of root resorption was 20 times greater when upper incisors were in close proximity to cortical plate. On the contrary, Otis et al.76 found that the amount of alveolar bone present around the root, the thickness of cortical bone, the density of trabecular network and fractal measurements on the bony trabeculae had no significant correlation with the amount of root resorption.
Verna et al.77 investigated the impact of bone turnover rate on the amount of tooth movement and the incidence of OIIRR in rats. High bone turnover increased the amount of tooth movement compared with the normal or low bone turnover state. The untreated side in the low bone turnover group showed more root resorption suggesting that in clinical situations where turnover of alveolar bone was delayed, root surfaces could already be affected by root resorption at baseline condition.
Type of Malocclusion
A number of studies have found a relationship between OIIRR and malocclusion.31,34,63,70 Severe malocclusion requires greater tooth movement, for example, greater overjet requires greater retraction and deeper overbite needs greater intrusion,31,78 with hence greater amounts of root resorption.
Kaley and Phillips75 reported that Class III patients showed severe root resorption with the root apex approximating the palatal cortical plate. They suggested that tipping forward of maxillary incisors to compensate for the Class III jaw relationship forces the roots against the palatal cortical plate during orthodontic treatment.
Harris and Butler70 demonstrated that open bite patients experienced significantly greater degrees of root resorption. It was believed that the orthopaedic forces of tongue thrusting generated the same physiological responses as mechanotherapy intended to torque or intrude a tooth. This study also suggested that:
- The greater the overjet, the greater the in-treatment root loss
- The greater the skeletal discrepancy, the greater the resorption
- The more the maxillary plane was tipped up anteriorly, the greater the resorption
- The steeper was Down’s occlusal plane, the greater was the observed degrees of incisor root shortening.
Hypofunctional Periodontium
A hypofunctional periodontium results in a narrowed periodontal space and derangement of functional fibres, which eliminates the normal cushioning effect of the PDL,79 thus resulting in a high concentration of force. This leads to stimulation of inflammation by the promotion of inflammatory mediators secreted from local cells to induce destruction of tooth and bone.80 Sringkarnboriboon et al.81 found that the amount of root resorption was significantly greater in teeth with a hypofunctional periodontium than in those with a normal periodontium, which suggested that orthodontic movement of non-occluding teeth should be performed with caution.
Specific Tooth Vulnerability to Root Resorption
The teeth most frequently affected by OIIRR according to severity are the maxillary lateral incisors, maxillary central incisors, mandibular incisors, the distal root of mandibular first molars, mandibular second premolars and maxillary second premolars.34,82–84 Maxillary lateral incisors are more susceptible to root resorption if they have abnormal root shape.34 Paetyangkul et al.85 showed in a micro-CT study that the maxillary premolars were more susceptible to orthodontic root resorption than mandibular premolars when these teeth were subjected to buccally directed force for 12 weeks.
Dental Invagination
Dental invagination is the most prevalent dental anomaly in orthodontic patients.86 Maxillary lateral incisors are most often affected followed by maxillary central incisors. It has been claimed that dental invagination was one of the predisposing factors for OIIRR.74,86 However, there is no general agreement concerning the role of dental invagination as a risk factor for orthodontic root resorption.87 Mavragani et al.88 investigated the association between dental invagination and root shortening during orthodontic treatment and found invaginated teeth often displayed deviated root form, which was considered a risk factor for OIIRR. However, invaginated teeth had delayed development and immature roots which seemed to protect against root resorption.89 The authors concluded that the mild form of dental invagination confined within the crown and not extended beyond the level of the cementoenamel junction was not a risk factor for OIIRR.
Abnormal Root Morphology
The tendency of OIIRR was found to be greater in teeth with aberrant shaped roots.34,74,90–92 Sameshima and Sinclair,34 in a comparative study using radiographs taken before and after orthodontic treatment, reported that teeth with abnormal root morphology, for example, pipette-shaped, pointed, dilacerated and slender roots, frequently showed OIIRR when compared with teeth with a normal root shape.
Oyama et al.93 investigated in a variety of root shapes the stress distribution at the root apex during orthodontic force application, using finite element method. They discovered that during orthodontic force application, short, bent and pipette root shapes resulted in a greater loading of the root than normal root shapes, which suggested root deviations tended to promote root resorption.
Root Resorption Prior to Orthodontic Treatment
Patients with pre-existing evidence of root resorption have been found to be at greater risk of developing further severe OIIRR with treatment.70,94
Previous Endodontic Treatment
Conflicting reports remain in the literature regarding the susceptibility of non-vital endodontically treated teeth to OIIRR. One group has found a greater incidence of OIIRR in endodontically treated teeth.95 The increase in root resorption in the study appeared to be biased as the non-vital teeth were treated endodontically as a result of trauma.95 Spurrier et al.96 found vital incisors resorbed to a significantl/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


