Diagnosis and Management of Dentoalveolar Injuries
Traumatic injuries to the teeth and supporting structures are commonly seen in the injured patient. Orofacial trauma is involved in approximately 15% of all emergency room visits, and 2% of these cases involve isolated dentoalveolar trauma.1 These injuries can be isolated, as in childhood falls (the major cause of all dental injuries),2 or can occur in association with other injuries, as seen in motor vehicle accident (MVA) victims. Children commonly sustain dentoalveolar injury usually between the ages of 8 through 12 years.3 Dentoalveolar injuries pose a major threat to dental health that may even surpass that of caries and periodontal disease.4
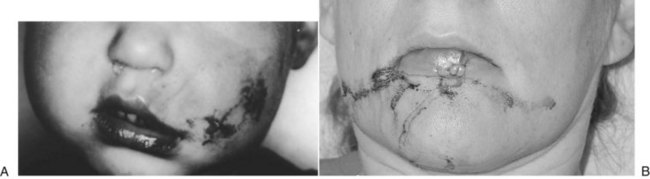
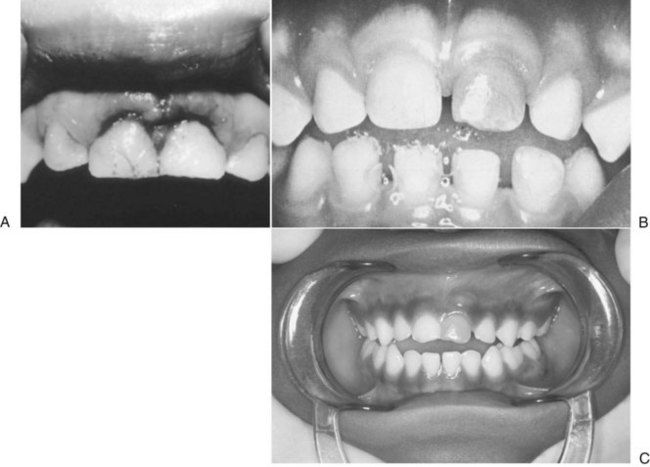
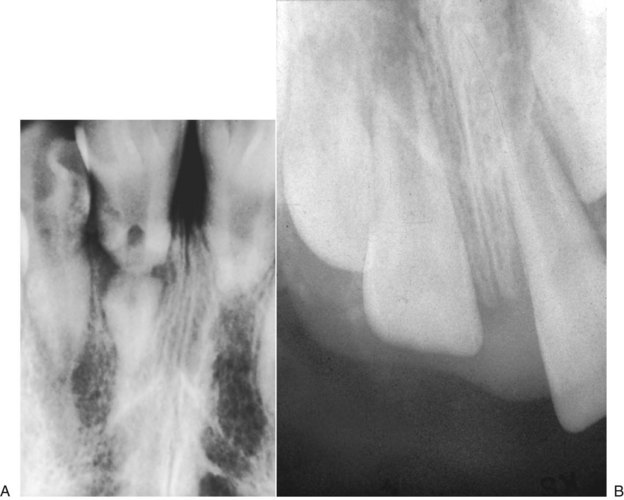
Dentoalveolar trauma ordinarily results from falls, playground accidents, abuse and domestic violence, bicycle accidents, MVAs, assaults, altercations, and athletic injuries. The dentoalveolar structures can be injured from direct trauma to the teeth or from indirect trauma, usually from forced occlusion, as the mandibular dentition is forcibly closed against the maxillary dentition.5–7 Direct trauma usually causes injury to the maxillary central incisors because of their relatively exposed position.8–13 Predisposing factors include abnormal occlusions, overjet exceeding 4 mm, labially inclined incisors, lip incompetence, a short upper lip, and mouth breathing (Fig. 13-1A).14 These conditions can be seen in individuals with class II division I malocclusions or oral habits, such as thumb sucking. Dental injuries are approximately twice as frequent among children with protruding incisors as among children with normal occlusions.15,16 Therefore, early orthodontic treatment in predisposed children may be an effective prevention strategy.17 Dental injuries are also common in patients who have been identified as accident prone (see Fig. 13-1B and C). Indirect trauma to the teeth and supporting structures usually results from a blow to the chin or from a forceful whiplash to the head and neck. If the teeth are out of occlusion or not protected by a mouthguard, they are forced into occlusion, resulting in damage to the posterior teeth, anterior soft tissue, or both (Figs. 13-2 and 13-3).7 The extent of the dental injury can be characterized by the energy of the impact. A low-velocity blow usually causes damage to the supporting dentoalveolar structures and a high-velocity impact usually results in crown fractures. Objects that are cushioned on impact typically result in alveolar damage and a reduced incidence of crown fractures. Sharp objects usually favor clean crown fractures as opposed to blunt objects, resulting in luxation, or root fractures. Variations in the direction of the impacting force usually result in multiple fracture sites.11,18
Injuries to the dentoalveolar structures increase in frequency substantially as a toddler begins to attempt to walk and run, at approximately 1 year of age.7,10,19,20 The incidence of injury to the dentoalveolar structures in school-age children is reported to be approximately 5%, usually resulting from falls on playgrounds and from bicycle accidents.13,21–25 Lacerations to the chin and vermilion border of the lip and crown fractures are commonly seen in children.26 Lacerations of the lip account for most injuries to oral structures.27 Participation in contact sports, such as hockey, soccer, football, basketball, boxing, and wrestling, can result in oral trauma. The use of an intraoral mouthguard during athletic practice and competition has been found to reduce intraoral injuries, notably in contact and noncontact sports.28 Skiing and snowboarding have also been shown to increase the risk of dentoalveolar trauma. Helmets with faceguards can help prevent serious trauma to the head and maxillofacial structures.29
Multiple injuries of the hard and soft tissues are the result of automobile accidents, with the greatest incidence of dental injuries occurring through the ages of 18 to 23 years.13 Dental trauma in older age groups may result from assault and domestic abuse, usually closely related to the abuse of drugs or alcohol, or both.11,30
Mucosal or gingival lacerations and mobile incisors are seen in oral injuries as a result of child abuse.31,32 In 1996, 4.3% of children younger than 18 years in the United States were reported to be victims of maltreatment.33 More than 3 million cases of child abuse are reported each year, with 1 million cases later being substantiated.34 Approximately 50% to 75% of the physical abuse cases had trauma to the facial and oral regions, with injuries to the upper lip and maxillary labial area.11,14,35,36 Abuse should always be considered if the child’s injuries show a marked discrepancy between the clinical evaluation and the history reported by the supervising adult, or if there appears to be a considerable period between the time of injury and when treatment is sought (Fig. 13-4).6
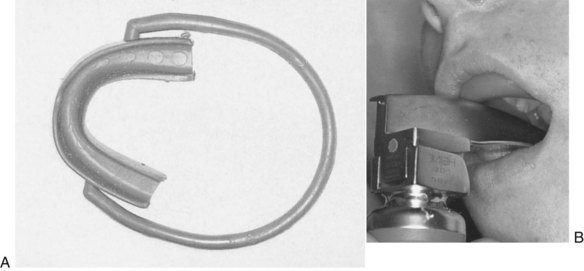
Many dentoalveolar injuries are associated with the management of the comatose patient37 or the patient undergoing general anesthesia.14,38–48 Lockhart et al44 have surveyed 133 directors of training programs in anesthesiology and found that an average of 1 in 1000 tracheal intubations resulted in dental trauma. They also reported that 90% of the dental complications might have been prevented with a screening dental examination of the patient and the use of a mouth protector (Fig. 13-5).45,46 It is important to remember that a mouth protector can be useful in protecting the anterior teeth during intubation, but it will not protect the teeth from poor technique. A retrospective analysis of 14 years of general anesthetic cases from a university hospital showed a 0.02% incidence in dentoalveolar trauma related to general anesthesia. Only 50% of these incidents occurred during intubation or extubation procedures, and 80% of all incidents were deemed by anesthesiologists to be unavoidable. Despite adequate prescreening, damage to dentoalveolar structures can occur. Care must be taken to avoid trauma to the dentoalveolar structures at all times during general anesthesia, not just during endotracheal intubation.47
Dental professionals are often asked to evaluate these injuries. Good documentation of the injury is essential because these cases may become involved in litigation. In the United States, damaged teeth constitute the most frequent anesthetic-related claim.48 An increased number of dentoalveolar injuries have also been seen in patients with mental retardation, epilepsy, drug abuse, and congenital abnormalities, such as familial dysautonomia.11,27
Dental trauma (single and multitooth) of the primary and permanent dentition occurs primarily in boys, originally related to participation in contact sports. The incidence of dentoalveolar injury in girls has increased notably as more competitive athletic opportunities have become available. A 2003 study reported that 9% of young adults aged 18 to 19 years who participated regularly in at least one sport had experienced dental injuries during sports participation at some point in their lifetimes.49 Several studies have shown a proportional relationship between the frequency of dental injuries and the summer months. Injuries to the deciduous teeth involve the supporting bone, because of its resilient nature, whereas injuries in the permanent dentition usually result in a higher percentage of crown and crown-root fractures. Therefore, impact absorption injuries are preponderant among younger children and sharp impact injuries are preponderant among older children.11–13,24,25,50
Examination and Diagnosis
Injuries to the teeth and supporting structures should be considered an emergency situation because successful management of the injury requires proper diagnosis and treatment within a limited time, especially in the case of avulsions and alveolar fractures.51
The initial evaluation must include a general assessment of the patient’s overall condition. The patient should be relieved of pain and displaced teeth and alveolar fractures should be reduced as quickly as possible to improve the prognosis for survival of these structures. A complete history of the mechanism and events of the injury should be obtained and a thorough clinical and radiographic examination performed quickly to ensure proper diagnosis and treatment (Fig. 13-6) because teeth have the lowest potential of any tissue for returning to a normal healthy state after injury. An incomplete examination can lead to inaccurate diagnosis and less successful treatment.52 It is important to remember that patients with dentoalveolar trauma may have concomitant head injury and that continual evaluation must be made of the patient’s neurologic status.53,54
A history can provide valuable information regarding the nature of the injury and any alterations in the normal occlusion, such as open bites or crossbites that were present before the injury. The nature of the accident can provide insight into the type of injury suspected, such as injuries to the maxillary anterior teeth with falls or associated jaw fractures with blows to the chin. If the history of the injury does not correspond to the clinical presentation, abuse should be considered. The patient should be referred for a medical examination.52,55–57 The time interval between the injury and presentation to the clinic is critical because the success of treating luxated teeth, avulsed teeth, crown fractures with and without pulp exposure, and alveolar fractures may be influenced by delayed treatment. The sooner the injury is treated, the more favorable the prognosis in most situations.7 Many post-traumatic dentoalveolar complications may also be associated with delays in treatment.1 Alterations in normal occlusion reported by the patient may indicate displaced teeth, dentoalveolar fractures, jaw fractures, or a combination.
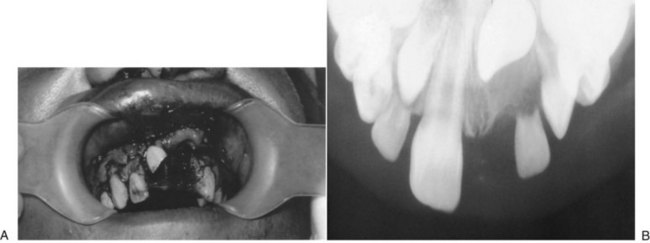
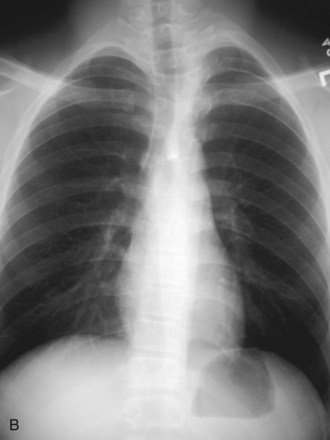
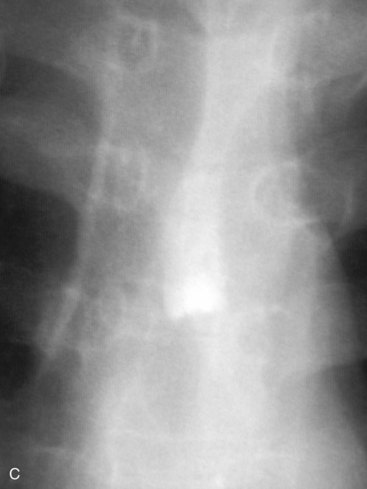
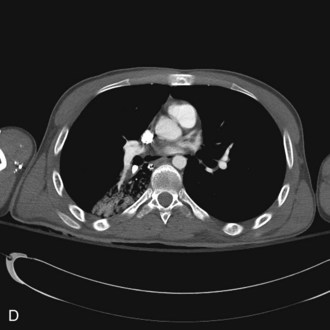
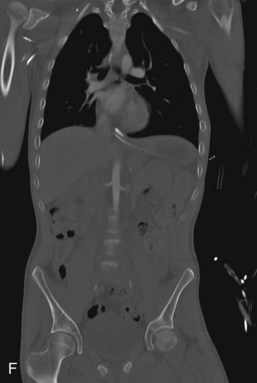
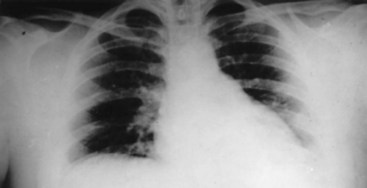
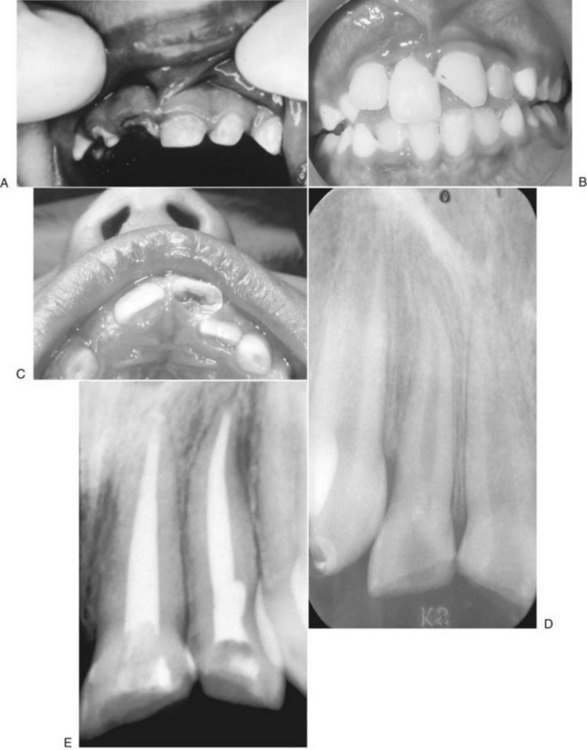
It is prudent that all teeth be accounted for at the time of examination. Extraoral as well as intraoral photographs have become increasingly beneficial in trauma cases. They not only aid in diagnosis and treatment planning, but can serve as further documentation of the trauma. Because trauma can result from abuse, assault, or even medical procedures, pictures can provide further evidence for medicolegal proceedings.58 Missing teeth or pieces of teeth that have not been left at the scene of the accident must be considered to have been aspirated, swallowed, or displaced into soft tissue of the lip, cheek, floor of the mouth, neck, nasal cavity, or maxillary sinus.59 A radiographic examination of the head and neck, chest, and abdomen must be performed to rule out the presence of teeth or teeth fragments within these tissues or organs (Figs. 13-7 to 13-11). It is important to note that in patients with maxillofacial trauma, teeth that are unaccounted for and loose may complicate anesthetic procedures.60 Early diagnosis and surgical removal of theses fragments could prevent undesirable foreign body reaction and scarring. In such cases, the need for taking routine facial soft tissue radiographs and chest x-ray before starting treatment is emphasized.61 The patient or those who have who transported the patient with avulsed teeth should be questioned regarding the storage media in which the avulsed tooth was transported, as well as how long the tooth has been out of the mouth.
A clinical examination should include an inspection of soft tissue for embedded fragments of tooth or debris. Lacerations, abrasions, and contusions should be examined and evaluated for damage to vital structures, such as the parotid duct, submandibular duct, nerves, and blood vessels. Extraoral wounds may indicate underlying dentoalveolar injuries. A wound under the chin suggests injury to the premolar and molar regions, mandibular fractures, or both, which may be associated with condylar trauma. Patients with suspected condylar trauma should have a full neurologic examination to rule out deficits and the improbable but reported protrusion of the condyle into the middle cranial fossa.54 Abnormalities in occlusion can indicate fractures of the jaws, dentoalveolar structures, or displacement of teeth. The direction of tooth displacement should be noted. In the primary dentition, the dislocation of the apex of the displaced primary tooth can possibly damage the succedaneous tooth. The direction of the dislocation and extent should be recorded (in millimeters). Fracture of the alveolar socket is common in displaced teeth. All teeth should be tested for abnormal mobility, horizontally and axially, which would suggest displacement of teeth or alveolar or jaw fractures. Disruption of the vascular supply to the pulp should be expected when axial mobility is present.7 Tongue blades can be found in emergency rooms to assess tooth mobility. Erupting teeth may exhibit some mobility that is unrelated to the injury. Movement of several teeth en bloc during the evaluation of a single tooth suggests fracture of the alveolar process. Uneven contours of the alveolar process may indicate a bony fracture.52,56
All the crowns of the teeth should be cleansed of blood and debris before evaluation for fractures of the crown and exposure of the pulp (Fig. 13-12A). Bleeding may be from lacerated mucosal tissue and nonlacerated marginal gingiva with damage to the periodontal ligament. Blood covering the alveolar process must be removed and the teeth and tissue evaluated for possible fracture, damaged teeth, and damaged periodontal tissue. The color of the traumatized tooth should be noted with the use of digital photographs or transillumination techniques because color changes may occur over time, indicating alterations in tooth vitality and representing gradual pulp necrosis.60–62 The involved teeth should be tapped or percussed with the handle of a mouth mirror or with a calibrated percussion instrument (e.g., Periotest, Medizintechnik Gulden, Modautal, Germany) to evaluate damage to the periodontal ligament. Pain elicited with percussion is suggestive of injury to the periodontal ligament (see Fig. 13-12B). Teeth that have undergone lateral luxation and intrusion usually do not demonstrate tenderness to percussion because these teeth are normally locked into their displaced position. The sound elicited by percussion is also of diagnostic value. A sound resembling a hard metallic ring is elicited with teeth that are locked into bone, whereas a dull sound indicates a subluxated tooth.52
Testing pulp vitality in acutely traumatized teeth is of questionable value because these procedures require the cooperation of a relaxed patient to prevent false-negative reactions. Mechanical stimulation and electric pulp testing have been advocated for examining the vitality and sensory perception of the dental pulp. Thermal tests, such as with heated gutta-percha, ice, ethyl chloride, carbon dioxide, and dichlorodifluoromethane, are usually of little value until several months have passed. Also, the reliability and the value of these tests have been questioned because noninjured teeth may also fail to respond. Although the functional repair of pulp nerve fibers has been shown to be reestablished approximately 35 days after reimplantation, the electric pulp tester is of little or no value in teeth with incompletely formed apices.63 The interpretation of vitality tests performed immediately after traumatic injuries is complicated by the fact that sensitivity responses are temporarily decreased, especially after luxation injuries. Repeated vitality tests show that normal reactions can return after a few weeks or months.7,62 Teeth that have been loosened can elicit pain responses merely from pressure of the pulp testing instrument; therefore, it is important to immobilize these teeth before testing. Teeth at different stages of eruption may sometimes show no reaction to stimulation. A 2007 study has shown that recently traumatized teeth yield positive responsiveness in thermal or electric pulp tests, which increased from no teeth showing responsiveness on day 0 (day of trauma) to 29.4% teeth on day 28, 82.35% of teeth at 2 months, and 94.11% teeth at 3 months.63 However, vitality readings with a pulse oximeter have yielded positive vitality readings that remained constant over the study period, from day 0 to 6 months in all patients. This is because blood flow in the tooth was being measured rather than thermal or electrical response in the tooth, which indicates the functioning of A delta nerve fibers.64,65
Another new method that has been developed to measure pulp vitality by measuring blood flow in the pulp is laser Doppler flowmetry (LDF). This noninvasive technique measures blood flow in the pulp and has been used in studying traumatized and luxated teeth to differentiate between those that are vital and those that are nonvital. Because this test produces no noxious stimuli, apprehensive or distressed patients accept it more readily than current methods of pulp vitality assessment.66,67 There has been some promise with this technique, especially in the case of deferred treatment. Studies have shown that vitality of a traumatized tooth can be ascertained in the first month with LDF and other modalities—ethylene chloride, CO2, or ice—do not elicit a clinical response until the 6-month follow-up.62,68 This may prevent the need for early invasive techniques that would otherwise be carried out if LDF were not used. However, this technique has been limited in its diagnostic value because measurements are difficult to evaluate through the crown of a tooth discolored by blood pigments and LDF relies on measurement of light transmission to function. The high cost of an LDF unit is also a limiting factor in its use.60,69
Radiographic evaluation of dentoalveolar injuries should include at a minimum a panoramic radiograph and periapical radiographs of the involved teeth. Computed tomography (CT) and cone beam CT (CBCT) provide more detail than panoramic and periapical radiographs and are helpful in diagnosing fractures of the teeth, roots, and supporting bone. Patients who are evaluated in the hospital setting will often have CT performed if there is evidence of trauma to the head and maxillofacial structures. These images can be helpful in diagnosis and treatment planning for further reconstruction after dentoalveolar injury. Use of CBCT in the oral and maxillofacial surgery office is becoming more prevalent and should be considered for dentoalveolar trauma patients. Valuable information for implant therapy can be obtained by CT and CBCT images regarding bone height and width and location of anatomic structures.70–72
The radiographic examination reveals the stage of root formation and discloses injuries affecting the root portion of the tooth and periodontal structures. Multiple periapical radiographs taken at different angles are useful to demonstrate root fractures that are minimally displaced. Ideally, three different angles should be obtained for each traumatized tooth.52 The radiographic examination should provide information concerning the following73:
• Degree of extrusion or intrusion
• Presence of preexisting periodontal disease
• Size of the pulp chamber and root canal
The radiographic appearance of teeth following luxation injuries is important in assessing pulp survival or necrosis. Teeth that have been displaced laterally or extruded radiographically exhibit a widening of the periodontal ligament space or displacement of the lamina dura, whereas intruded teeth often demonstrate an absence of the periodontal ligament space. Fracture of the alveolar process may appear radiographically as a small radiolucent line, which in some cases is blurred on the panoramic radiograph but detectable on periapical radiographs (Fig. 13-13).
Classification
Many systems have been developed to classify various traumatic injuries to the teeth and supporting structures.21,74–78 The present classification is based on a system presented by the World Health Organization26 and modified by Andreasen.7 It includes injuries to the teeth, supporting structures, gingiva, and oral mucosa based on anatomic, therapeutic, and prognostic considerations.
Injuries to Hard Dental Tissue and Pulp
Crown Infraction.
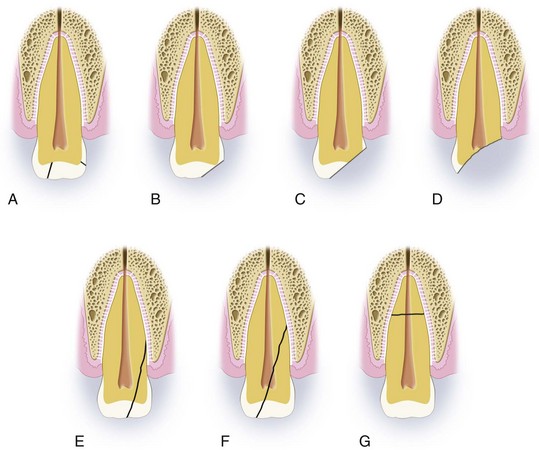
A crown infraction (Fig. 13-14A) is an incomplete fracture or crack of the enamel without loss of tooth substance.
Uncomplicated Crown Fracture.
An uncomplicated crown fracture (see Fig. 13-14B and C) is a fracture confined to the enamel or involving the enamel and dentin without exposing the pulp.
Complicated Crown Fracture.
A complicated crown fracture (see Fig. 13-14D) involves enamel and dentin with exposure of the pulp.
Uncomplicated Crown-Root Fracture.
An uncomplicated crown-root fracture (see Fig. 13-14E) involves enamel, dentin, and cementum without exposure of the pulp.
Injuries to the Periodontal Tissue
Concussion.
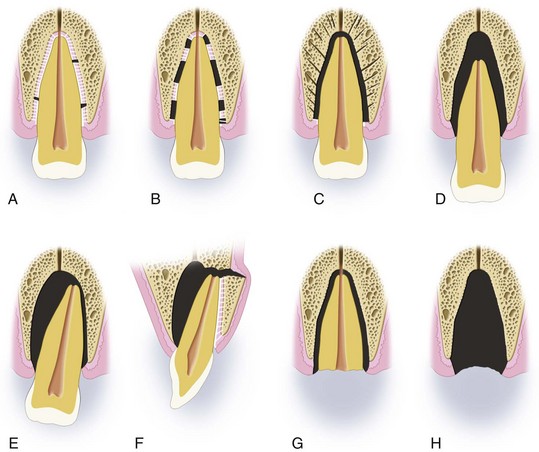
A concussion (Fig. 13-15A) is an injury to the tooth-supporting structures without abnormal loosening or displacement of the tooth but with marked reaction to percussion.
Subluxation (Loosening).
Subluxation (see Fig. 13-15B) is an injury to the tooth-supporting structures with abnormal loosening but without displacement of the tooth.
Intrusive Luxation (Central Dislocation).
Intrusive luxation (see Fig. 13-15C) is displacement of the tooth into the alveolar bone with comminution or fracture of the alveolar socket.
Extrusive Luxation (Peripheral Dislocation, Partial Avulsion).
An extrusive luxation (see Fig. 13-15D) is partial displacement of the tooth out of the alveolar socket.
Lateral Luxation.
A lateral luxation (see Fig. 13-15E and F) is displacement of the tooth in a direction other than axially, accompanied by a comminution or fracture of the alveolar socket.
Injuries to the Supporting Bone
Comminution of the Alveolar Socket.
Crushing and comminution of the alveolar socket (Fig. 13-16A) can occur together with intrusive and lateral luxation.
Fracture of the Alveolar Socket Wall.
A fracture of the alveolar socket (see Fig. 13-16B and C) is confined to the facial or lingual socket wall.
Treatment
3. Injury to the primary or permanent dentition and stage of root development
4. Location and extent of the injury—horizontal and proximal superficial (corner) fractures demonstrate a low frequency of pulp necrosis, whereas deep proximal fractures show an increased risk of eventual pulp necrosis.
6. Periodontal health of the remaining teeth
7. Whether or not there has been a fracture of supporting bone
9. Whether apical foramina are wide or narrow
11. Extent of any concomitant head, chest, or abdominal injuries may affect the treatment of the dentoalveolar injury and length of time between trauma and treatment.11,79
Also, the practitioner should determine the amount of time that has passed since the injury occurred and what storage medium, if any, was used.80,81 Lack of cooperation on the part of the patient, especially young children and mentally challenged individuals, may require the use of a general anesthetic or intravenous sedation.
The periodontal health of the involved and adjoining teeth must be evaluated for osseous support of the traumatized teeth and to determine whether the adjoining teeth can be used for splinting, if indicated. The prognosis for traumatized teeth is generally better in younger patients and in vital teeth with wide apical foramina, teeth with intact soft tissue, teeth with no root fractures, and teeth with maximal bone support.82 Any blow to a tooth, even in the absence of obvious dental injury, can endanger pulp vitality by severing the apical vessels or through secondary pulp hyperemia and congestion, resulting in ischemia and possibly leading to necrosis. Therefore, long-term dental follow-up is necessary. The typical follow-up schedule should include a clinical visit within 24 to 48 hours after the initial clinical evaluation and treatment, followed by a clinical visit within 2 weeks for removal of the splint. Monthly clinical visits are planned for the first 6 months and should be followed up by annual visits for 5 years.3,83,84 The patient should be informed that future endodontic therapy may be necessary, regardless of the severity of injury to the teeth and supporting structures (Fig. 13-17).7,85–89
The treatment of traumatized primary incisors is complicated by the size of the pulp cavity, susceptibility of the developing permanent tooth, and cooperation of the child. It is also important to note than any type of traumatic injury to a primary tooth could result in potential sequelae to the permanent tooth. Concerning the permanent dentition, the most common developmental disturbances are discoloration of enamel and/or enamel hypoplasia (46.08%) and eruption disturbances (17.97%) caused by the traumatic injury in their predecessors. It has not been possible to find an association between the type of injury in primary teeth and sequelae in their successors.90 Heroic methods designed to maintain the primary incisors after trauma should be discouraged. The loss of primary incisors does not require space maintenance as growth occurs, regardless of which primary incisors are involved, but loss of primary molars may require space maintenance to prevent mesial drift of the permanent first molar.7,9,85,91 If the primary incisor is lost before the roots begin to be absorbed (between the ages of 3 and 4 years), eruption of the succedaneous permanent tooth is often delayed. However, this delay usually does not create additional orthodontic problems. If the primary tooth is lost after 25% of the permanent incisor root has formed (between the ages of 4 and 5 years), eruption of the permanent successor is often accelerated.
Injuries to Hard Dental Tissue and Pulp
Crown Infractions.
Infractions are often overlooked. It is important that direct transillumination (directing a light beam perpendicular to the long axis of the tooth from the incisal edge) be performed for adequate evaluation and treatment.92 Infractions predominantly result from a direct impact to the enamel, frequently occurring on the labial surface of the maxillary incisors. Usually no treatment is indicated for a crown infraction or cracks in the enamel layer (see Fig. 13-14A). Sealing multiple infraction lines with unfilled resin and an acid etch technique may prevent stains from becoming an aesthetic problem. The vitality of the traumatized tooth should be documented at the time of diagnosis and evaluated adequately by periodic follow-up to monitor the pulpal health of the involved tooth. If the tooth does not respond to pulp vitality testing at the time of injury, endodontic therapy is not indicated immediately, but the tooth must be kept under observation. The patient should be informed of signs and symptoms that may occur, such as pain, swelling, and tooth discoloration. If the patient experiences any of these, further evaluation and potential treatment may be necessary. The prognosis with respect to pulp necrosis is good, provided that concussion or subluxation injuries are not overlooked.11
Crown Fractures.
For crown fractures that involve the enamel only (see Fig. 13-14B), treatment is limited to smoothing of sharp edges or restoration with acid etch composite (Fig. 13-18A). Because of aesthetic demands, midline symmetry may also be recovered with orthodontic extrusion of the tooth to restore properly balanced incisal height. The treatment objectives are to restore the crown’s anatomy and occlusion, thus preventing labial protrusion, drifting, tilting, or extrusion of adjacent and opposing teeth into the fracture site (see Fig. 13-18B and C). The risk of pulp necrosis is minimal.
Fractures without exposure of the pulp from oral trauma occur more frequently than any other type of crown fracture in the primary and permanent dentitions. Exposed dentin usually is sensitive to thermal changes and mastication. If there is a notable amount of dentin exposed, measures should be taken to do the following: (1) seal the dentin tubules from microbial irritants to prevent ingress of bacteria; and (2) promote secondary dentin deposition by the pulp tissue (Fig. 13-19; also see Fig. 13-18D). A calcium hydroxide liner is placed over the exposed dentin and the tooth form is restored with a composite restoration. This traditional technique has been well studied, but current evidence suggests that because calcium hydroxide is soluble in water, the dentinal tubule fluid on surfaces of the exposed fractured site interferes with the calcium hydroxide material, resulting in its dissolution and loss of protective function over time. An alternative treatment uses glass ionomer cement as a liner, which has proven to be as effective.92 Reattachment of the fractured segment using dentin-bonding agents can be performed to restore the tooth and reduce the microleakage around the restoration.11 There is no change in the bond strength with the use of the dentin-bonding agents compared with standard enamel bonding techniques.93 No matter which technique is used, the tooth should be evaluated periodically for alterations in pulpal health. The overall risk for pulp necrosis is minimal, with associated luxation injuries, stage of root development, type of treatment, and extent of fracture increasing the risk of pulp necrosis.
If the pulp tissue is exposed (see Fig. 13-14C), measures must be taken quickly to attempt to preserve the vitality of the neurovascular tissue because hemorrhage from the exposed pulp is usually present. Teeth with pulp exposure require pulp capping, partial pulpotomy, or endodontic therapy. The primary aim is to preserve a vital noninflamed pulp surrounded by hard tissue. Whichever treatment option is used, careful periodic evaluation is necessary, including clinical examination, vitality testing, and periapical radiographs. If the tooth is relatively sound, a pulp-capping procedure with calcium hydroxide liner or mineral trioxide aggregate (MTA) and composite restoration should be performed. MTA is a bioactive material that can create an ideal environment for healing. From the time that MTA is placed into direct contact with human tissue, it appears that the material does the following:
1. Forms calcium hydroxide (CH) that releases calcium ions for cell attachment and proliferation
2. Creates an antibacterial environment by its alkaline pH
3. Modulates cytokine production
4. Encourages differentiation and migration of hard tissue–producing cells and
5. Forms hydroxyapatite (HA, or carbonated apatite) on the MTA surface and provides a biologic seal
To achieve the best prognosis, the pulp-capping procedure should be carried out only in teeth with small exposures and those that appear within 24 hours after injury (Fig. 13-20A and B). Pitt-Ford and Patel65 have compared CH and MTA as pulp-capping agents on monkeys’ teeth. Their results showed that most pulps capped with MTA were free of inflammation and all of them showed calcified bridge formation after 5 months. In contrast, the pulp of teeth capped with CH showed the presence of inflammation and significantly less calcified bridge formation. MTA promotes dentin bridge formation through differentiation of pulpal cells into odontoblastic-like cells.94–96 MTA has grown in favor with clinicians because of its biocompatibility and ability to help maintain pulp vitality.
Pulp capping is also indicated in complicated crown fractures in immature teeth, in which maintenance of pulp vitality is desirable. Most complicated fractures eventually require partial or complete pulpotomy; the latter procedure should be considered a temporary treatment and should be followed by pulpectomy when root development is complete.92 A cervical pulpotomy involves removing 2 to 4 mm of pulp tissue subadjacent to the exposure (i.e., all the coronal pulp), placing a CH or MTA base, and using an acid etch composite for restoration.
A cervical pulpotomy is indicated in cases involving immature teeth with incomplete closure of the apex because it is not indicated for teeth with concurrent displacement injuries. CH paste or MTA has been demonstrated to promote closure of the apex of the immature tooth.7 There have been multiple studies confirming MTA’s ability to help promote apex closure and, again, may be a superior material to CH.94
Completion of root canal therapy is usually indicated by closure of the apex. This closure can be confirmed by serial radiographs, usually within 3 to 6 months. Partial, or Cvek, pulpotomy implies the removal of pulp tissue to only a depth of 1 to 2 mm. Partial pulpotomy provides many advantages when compared with cervical pulpotomy because there is no necessity for subsequent endodontic therapy and the cell-rich coronal tissue is preserved (see Fig. 13-20C).97
If the teeth are mature and fully formed, with notable exposure of the pulp tissue, total pulp removal is indicated (Fig. 13-21). The canals should be completely treated endodontically and filled with gutta-percha to prevent post-traumatic complications associated with pulp necrosis. Follow-up examinations are necessary to evaluate all traumatized teeth (with pulp exposure treated conservatively for degenerative pulp necrosis) and to determine whether definitive root canal therapy is necessary. Definitive restoration of crown fractures consists of composite restorations, reattachment of original crown fragments, full crown coverage, or laminate veneers.
Crown-Root Fractures.
Crown-root fractures (see Fig. 13-14E and F) account for 5% of traumatic injuries to the permanent teeth and 2% of injuries to the primary dentition. The treatment options are dependent on the amount of root remaining. Treatment goals are to preserve the remaining root fragment to support a post and crown prosthesis, which requires additional periodontal procedures, such as gingival-alveolar surgery or orthodontic measures to expose the retained root segment.
Primary teeth with any type of crown-root fracture should be extracted and conventional prosthetic-restorative treatments provided.7,85,98 Emergency treatment should include stabilization of the coronal fragment to adjacent teeth with an acid etch resin splint.99 In the permanent dentition, uncomplicated fractures of the enamel, dentin, and cementum depend on the location of the fractured segment, which determines the type and extent of treatment. If the fracture line is above or slightly below the cervical margin, the tooth can be restored, as with a crown fracture. Occasionally, crown-lengthening procedures are necessary to allow restoration of the margin. If the fracture continues too apically to allow adequate restoration, extraction of the tooth may be indicated. If the pulp is involved (complicated), the level of the root fracture determines the treatment. Extraction is usually indicated if the coronal segment includes more than one third of the clinical root or in cases of vertical root fractures; otherwise, the tooth may be treated endodontically and restored. When the coronal fragment compromises one third or less of the clinical root and the fracture line extends below the marginal bone level, adequate access to provide margins on sound tooth structure is necessary. This can be accomplished by extrusion, by surgical exposure (gingivectomy or osteotomy) or orthodontic elevation of the fracture surface, or by crown-lengthening procedures.92 Surgical procedures are indicated only in teeth with completed root development and an apical fragment long enough for definitive restorative procedures.99 The stability of orthodontic movements has been evaluated and it was concluded that the risk of relapse is always present but can be minimized by fibrotomy techniques.100 If the tooth is mature and root formation is complete, endodontic treatment is indicated. If the apex is open, a pulpotomy should be performed with a CH or MTA base and should be observed through the use of x-rays for closure of the apex, after which definitive root canal therapy and permanent restoration can be initiated. A crown-root fracture of a tooth in a young person may require extraction and placement of a space-maintaining partial denture. Alternative treatments have been presented in the literature, suggesting the retention of the root fragment by the procedures described until the completion of the pubertal growth spurt to preserve the alveolar bone. After that time, definitive treatment can be accomplished with placement of endosseous implants.98
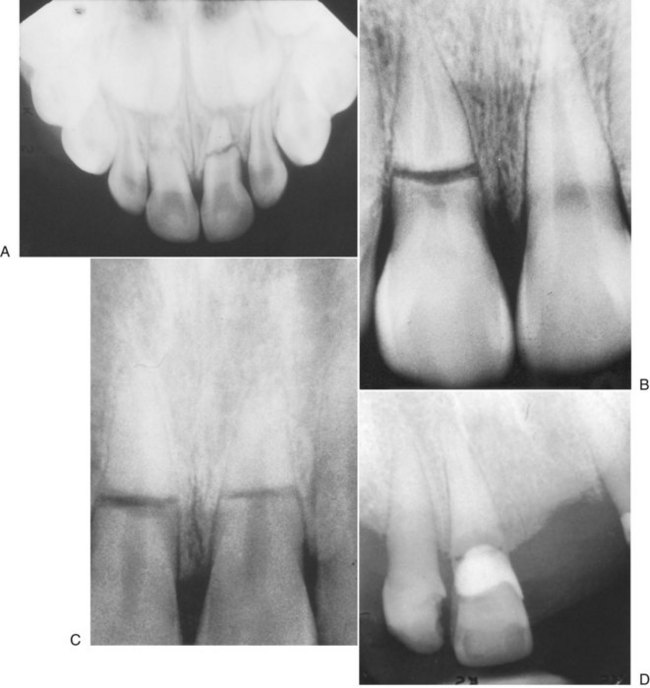
Root Fractures.
Root fractures (see Fig. 13-14G) account for approximately 6% of cases of dental trauma.101 Root fractures account for approximately 7.7% of the trauma associated with the permanent dentition and 3.8% in the primary dentition. Careful examination of the supporting soft tissue, alveolar bone, and surrounding teeth is important in patients with suspected root fractures.
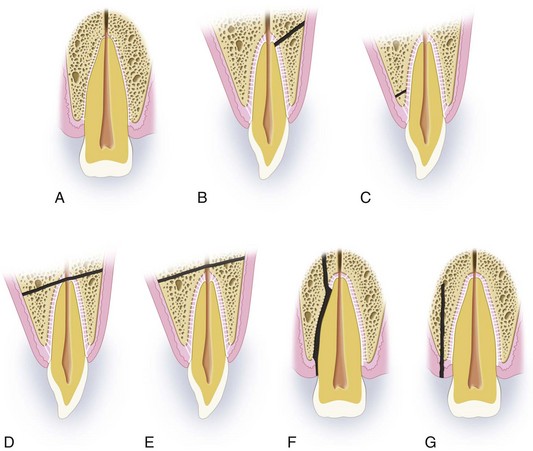
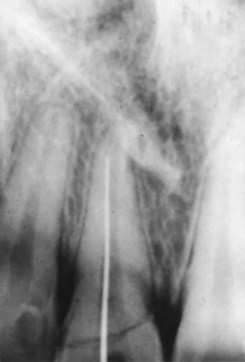
The teeth most commonly traumatized by root fractures are the maxillary incisors (75%). Concomitant fracture of the surrounding alveolar bone is associated with 40% of teeth involved with root fractures, and additional teeth are traumatized in 45% of cases initially found with root fractures.102 Careful follow-up care is important for patients with root fractures, not only to evaluate the teeth that are directly involved but also to evaluate surrounding teeth and alveolar bone, which may demonstrate complications over time not obvious at the initial presentation and evaluation of the patient. Horizontal root fractures occur mostly in maxillary central incisors of male patients. These are fully erupted permanent teeth with closed apices and are solidly supported by bone and periodontium.103 The most common mechanism of injury is a frontal impact on the dentoalveolar structures. The clinical examination reveals a slightly extruded tooth, usually displaced in a lingual direction and clinically difficult to distinguish because of root fracture from luxation injury. A reliable radiographic examination is necessary for a proper diagnosis. Occlusal radiographs are ideal for disclosing fractures in the apical third of roots, whereas periapical views are better for fractures in the coronal segment.101,104
Root fractures in primary teeth are uncommon before the completion of root development. Root fractures in primary teeth without mobility can be preserved and should exfoliate normally. If there is mobility or dislocation of the coronal segment, the tooth should be removed without attempts to remove the apical fragments, which could possibly damage the permanent tooth. Normal physiologic resorption of the apical fragment can be expected (Fig. 13-22A). Leaving a mobile coronal segment will more likely cause pulp necrosis to develop and removal is indicated.104
Root fractures of the permanent teeth are most prevalent in the maxillary central incisor region in the 11- to 20-year-old age group.104 Studies have shown a survival rate of up to 80% in root-fractured teeth when treated appropriately.105
The prognosis of the involved tooth and treatment indicated are dictated by the level of the fracture along the horizontal aspect of the root (see Fig. 13-22B and C). If the fracture is in the apical third of the root and there is little or no mobility, the prognosis is good and minimal treatment is indicated.1,3,101,103 Surgical removal of the root tip can also be considered with the retained segment sealed.105 If possible, however, the apical segment should be left to minimize bony resorption. The coronal fragment of the tooth generally remains vital and endodontic treatment usually is not necessary. If the fracture line is closest to the gingival crevice, there is a poor chance that healing with calcified tissue will occur. The worst prognosis is associated with high root fracture where the coronal portion is mobile (see Fig. 13-22B) compared with apical or midroot fractures (see Fig. 13-22C).104,106 The higher the fracture on the root, the greater the chance of a communication between the oral cavity and root fracture line developing, based on the degree of periodontal disease and bone loss present before the injury. It is important to evaluate the patient’s oral hygiene, especially around the gingival margins, and the periodontal status around the involved tooth, which might eventually dictate treatment. If the fracture occurs near the cervical margin (see Fig. 13-22D) and significant mobility is present, both the coronal and apical fragments are extracted or only the coronal portion is removed, complete endodontic treatment is carried out on the retained apical portion, and restoration is completed with a crown over a post and core. Alternatively, after removal of the coronal fragment, subsequent orthodontic or surgical extrusion of the remaining apical fragments may be necessary so that the final crow/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses