CHAPTER 13 CONTEMPORARY SUBANTRAL SINUS SURGERY AND GRAFTING TECHNIQUES
The atrophic edentulous posterior maxilla often poses problems for implant placement. Following loss of teeth there is a gradual loss of alveolar bone and in many patients the sinus floor dips close to the alveolar ridge, leaving less than optimal bone height or width for placing implants. In some patients the loss of alveolar bone coupled with increased antral pneumatization may result in only a 2- to-3 mm thickness of alveolar bone height. The result is insufficient bone to place implants.1 For these patients the sinus lift procedures represent a treatment of choice.
Sinus lift subantral augmentation has produced excellent results with few complications.2,3 Autogenous bone alone or in combination with particulate allografts, xenografts, or alloplasts has provided excellent results.4 More recently, to reduce donor site morbidity, blood loss, operative time, and postoperative complications, allografts, xenografts, and/or alloplasts alone or in combination have been used as the graft of choice without the addition of autogenous bone.5 The grafts are combined with the patient’s blood, platelet-rich plasma, bone marrow aspirate, aqueous antibiotics, or sterile saline.6 In some cases, depending on the volume of alveolar bone, simultaneous sinus lift subantral augmentation and implant placement can be accomplished for the patient.7,8
 Historical Perspective
Historical Perspective
As far back as the 18th century successful sinus surgeries were performed using calcium sulfate as the graft material.9 In 1893 American physician George Caldwell and French laryngologist Henry Luc accessed the maxillary sinus by creating a lateral window providing access to lift the sinus membrane. Hilt Tatum, in 1975, introduced a technique to increase alveolar bone height that placed graft material under the maxillary sinus membrane prior to placing implants.10 In 1980 Boyne and James, using the Caldwell-Luc procedure, grafted autogenous bone between the sinus membrane and antral floor.11 Smiler and Holmes reported a series of five successful subantral grafts performed via a lateral window approach using porous hydroxyapatite alone as the graft material in 1987.12
 Biologic and Anatomic Considerations
Biologic and Anatomic Considerations
Morphology
The adult maxillary sinus, or antrum of Highmore, lies within the body of the maxilla. It is the largest of the paranasal sinuses, measuring on average 34 × 33 × 23 mm with a 15 mL volume. It can occupy the body of maxilla from the tuberosity to the canine fossa. The root apices of molar teeth can extend into the sinus with only a thin sheet of bone or connective tissue separating the antrum from the oral cavity.13 With age and loss of maxillary posterior teeth there is progressive alveolar atrophy, increased pneumatization of the sinus, and thinning of the buccal wall.
The mucosal lining of the sinus has a rich vascular network of complex vascular loops that help warm and filter inspired air. This layer of peudostratified columnar ciliated epithelium and connective tissue lines the maxillary sinus. The rapid, rhythmic sweeping movements of the cilia remove the mucus that goblet cells secrete, with the debris and bacterial contaminants, toward the ostium to the middle meatus of the nose.14–17
Vascular Supply, Lymphatic Drainage, and Innervation
Arterial Supply
Branches of the maxillary artery via the external carotid artery supply the maxillary sinus. These include the infraorbital artery as it runs with the infraorbital nerve, the terminal branches of the sphenopalatine artery, and the posterior lateral nasal artery that supplies the medial wall of the maxillary sinus and the mucous membrane lining of the lateral nasal wall. Branches of the facial artery,18 the pterygopalatine artery, the greater palatine artery, the alveolar artery, and the posterior superior alveolar artery supply the lateral wall of the sinus.19–21
Venous Return and Lymphatic Drainage
Venous return of the anterior region of the maxillary sinus drains from the cavernous plexus into the facial vein. The posterior return is into the pterygoid plexus of veins via the sphenopalatine vein and the retromandibular and facial veins. These empty into the internal jugular vein.22 The lymphatic drainage from the maxillary sinus is via the infraorbital foramen though the ostium and into the submandibular lymphatic system.
 Incision
Incision
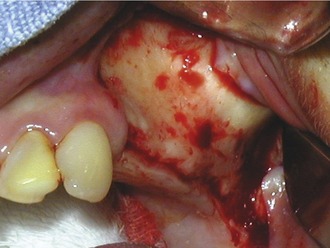
A crestal incision is made along the alveolar crest from the tuberosity to the anterior border of the sinus. A vertical relaxing incision, anterior to the planned osteotomy, is made to the depth of the vestibule to facilitate tissue release. Dissection is initiated at the apex of the crestal and vertical relaxing incisions. The mucoperiosteal flap is reflected with a periosteal elevator or molt curette to expose the canine fossa, malar buttress, and infratemporal fossa (Figure 13-1). Care is taken not to tear the periosteum.
 Quadrilateral Buccal Osteotomy
Quadrilateral Buccal Osteotomy
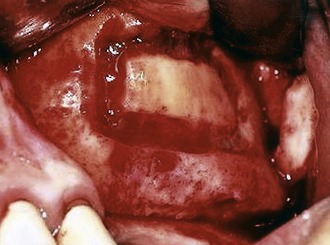
Although the hinge osteotomy was one of the first approaches for sinus lift grafting, this procedure worked well only when there was sufficient vertical maxillary bone height.12 The quadrilateral buccal osteotomy is indicated for either normal or minimal vertical maxillary bone height. An advantage of quadrilateral osteotomy is that it permits the sinus membrane to be elevated higher than the superior horizontal osteotomy. The surgery proceeds after reflection of the mucoperiosteal flap and exposure of the lateral wall of the maxilla, the canine fossa, the malar buttress, and the infratemporal fossa. An inferior horizontal osteotomy begins 2-to-3 mm above the floor of the antrum in the area of the first molar using a #6 or #8 round bur and copious irrigation23 (Figure 13-2). A small round bur or a fissure bur must not be used because either will most likely cause tearing of the schneiderian membrane.
The anterior vertical bone cut is begun from the inferior horizontal osteotomy and extended as high as access permits. The superior horizontal osteotomy extends from the superior limit of the anterior vertical bone cut posterior to approximate the length of the inferior horizontal osteotomy. A posterior vertical osteotomy connects the inferior and superior horizontal bone cuts to complete the quadrilateral osteotomy (Figure 13-3).
 Elevation of the Schneiderian Membrane
Elevation of the Schneiderian Membrane
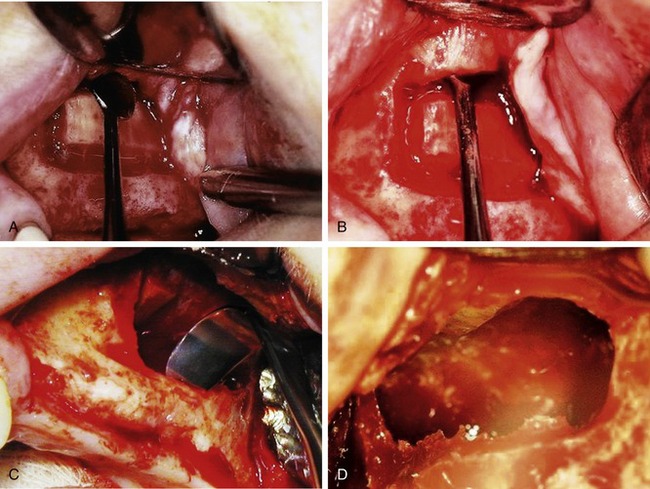
The quadrilateral osteotomy exposes the schneiderian membrane circumferentially around the bone cuts. The membrane is first lifted along the superior horizontal osteotomy using broad-based freer elevators or curettes (Figure 13-4, A) The membrane can be elevated higher than the superior bone cut (Figure 13-4, B). This is especially important when the anatomy and resorption patterns restrict visibility and exposure.
With the sharp border of the dissection elevators placed on bone, and its broad base supporting the membrane, the membrane is lifted from its anterior and posterior walls (Figure 13-4, C). Further dissection exposes the medial wall of the sinus (Figure 13-4, D). The buccal osseous window stays attached to the schneiderian membrane as elevation continues. The bony wall turns inward and is positioned horizontally in the superior aspect of the dissection.
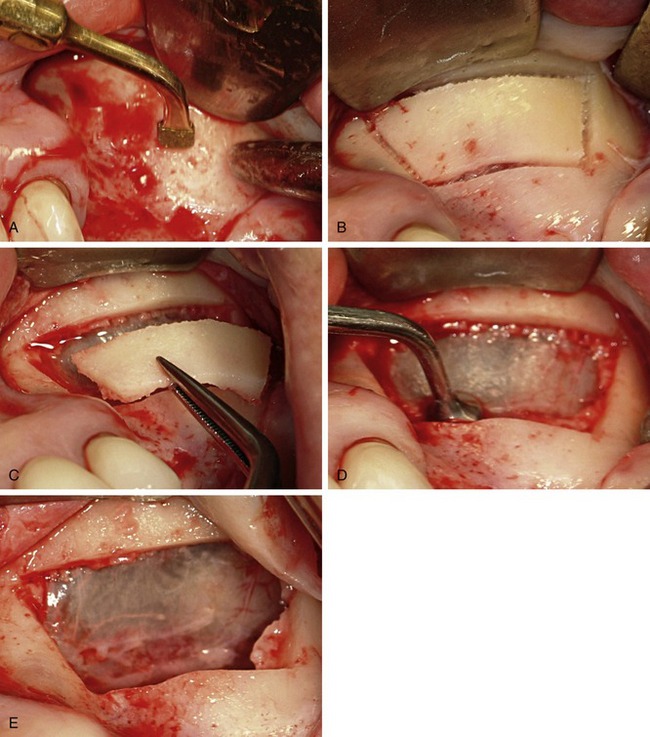
Piezosurgery with the diamond-coated insert or saw insert will cut a precision osteotomy (Figure 13-5, A). The quadrilateral osteotomy (Figure 13-5, B) can be removed, exposing the sinus membrane (Figure 13-5, C). Using the noncutting smooth insert, the membrane is elevated (Figure 13-5, D). The elevated membrane exposes the medial, inferior, and posterior bone walls of the sinus (Figure 13-5, E).
 Grafting the Osseous Cavity
Grafting the Osseous Cavity
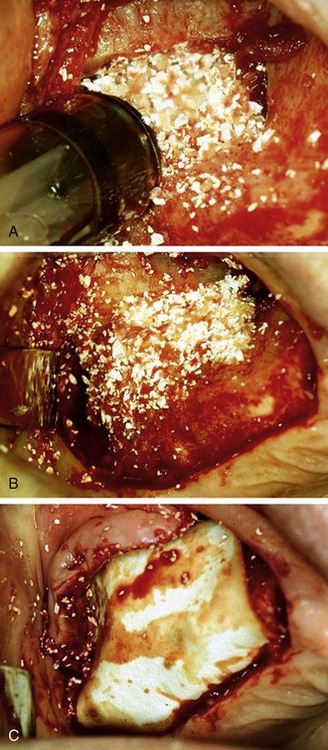
Graft material is placed under the membrane within the osseous cavity in an anterior inferior direction and with a loose compaction. It is important that the graft is in contact with the medial osseous wall (Figure 13-6, A). Graft is added until the cavity is loosely filled, reconstituting the buccal wall (Figure 13-6, B). Overpacking the site and/or pressure in a superior direction is avoided because this might tear the membrane. Also, overcompressing the graft restricts blood flow into the material, inhibits angiogenesis, decreases oxygen tension, and compromises success. The mucoperiosteal flap is then repositioned and sutured. If the periosteum is torn a hemostatic collagen wound dressing or a guided bone regenerative membrane can be placed over the buccal window to inhibit fibrovascular growth into the graft (Figure 13-6, C).
 Complications
Complications
Dehiscence of the Incision
A vestibular horizontal buccolabial incision should be avoided. The blood supply in the vestibule is diminished when compared to alveolar crest–attached keratinized tissue. Suturing in this area is also more difficult.24 In addition, flanges of an appliance must be reduced because they impinge on the vestibule and push the incision apart.25
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses