Chapter 13 Actinomycetes, clostridia and Bacillus species
Actinomycetes
Actinomyces israelii
Culture and identification
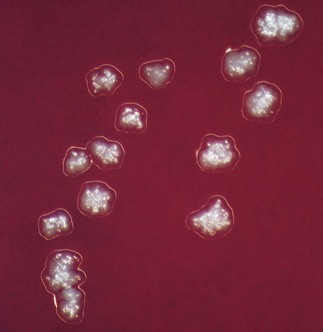
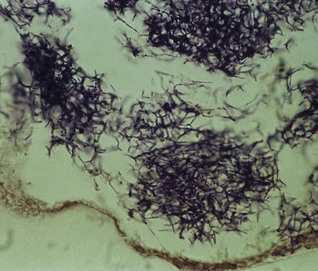
Grows slowly under anaerobic conditions, on blood or serum glucose agar at 37°C. After about a week, it appears as small, creamy-white, adherent colonies on blood agar. The colonies resemble breadcrumbs or the surface of ‘molar’ teeth (Fig. 13.1). Because of the exacting growth requirements and the relatively slow growth, isolating this organism from clinical specimens is difficult, particularly because the other, faster-growing bacteria in pus specimens tend to obscure the slow-growing actinomycetes. ‘Sulphur granules’ in lesions are a clue to their presence. When possible, these granules should be crushed, Gram-stained and observed for Gram-positive, branching filaments, and also cultured in preference to pus.
Pathogenicity
Most (70–80%) actinomycotic infections are chronic, granulomatous, endogenous infections of the orofacial region (Fig. 13.2). Typically, the lesions present as a chronic abscess, commonly at the angle of the lower jaw, with multiple external sinuses. There is usually a history of trauma such as a tooth extraction or a blow to the jaw. Actinomycetes are also isolated from infections associated with intrauterine devices, but their pathogenic role is unclear.
Clostridia
Clostridia comprise many species of Gram-positive, anaerobic spore-forming bacilli (but spores are not found in infected tissues); a few are aerotolerant. They are an important group of pathogens widely distributed in soil and in the gut of humans and animals. There are four medically important species (Clostridium tetani, Clostridium botulinum, Clostridium welchii and Clostridium difficile) that cause significant morbidity and mortality, especially in developing countries. The major diseases caused by these organisms are listed in Table 13.1.
Table 13.1 Common Clostridium species associated with human disease
| Clostridium spp. | Disease |
|---|---|
| C. welchii | Gas gangrene, food poisoning, bacteraemia, soft-tissue infections |
| C. tetani | Tetanus |
| C. botulinum | Botulism (foodborne, infant, wound) |
| C. difficile | Pseudomembranous colitis, antibiotic-associated diarrhoea |
| Other species (e.g. C. septicum, C. ramosum, C. novyi, C. bifermentans) |
Bacteraemia, gas gangrene, soft-tissue infections |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses