Radiographic Evaluation of Facial Injuries
Until the 1980s, diagnostic imaging of facial injuries consisted almost exclusively of standard facial and panoramic radiographs and, if available, tomographic studies. Although standard radiographs are still useful for assessing these injuries and their repair, especially during the intraoperative and early postoperative periods, computed tomography (CT) is widely and routinely used as initial or supplemental diagnostic imaging of facial trauma. This chapter will review the role of diagnostic imaging in the evaluation of the patient with maxillofacial trauma, radiographic maxillofacial anatomy, and various imaging techniques.1
Maxillofacial Skeleton and Significance of Osseous Structures
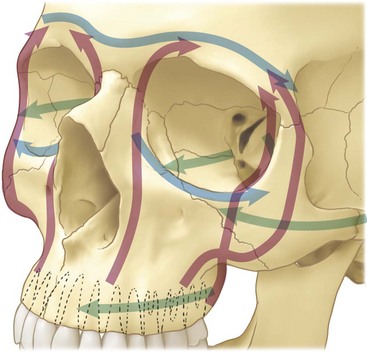
There are three vertical buttresses of the midface that provide the primary support in the vertical and anteroposterior (AP) directions. These are the nasomaxillary, zygomatic, and pterygomaxillary buttresses2 (Fig. 12-1A). In the AP direction. the structures that support the facial projection are the frontal bone, zygomatic arch and zygoma complex, maxillary alveolus, palate, and basal segment of the mandible from one angle to the other.3 The main objective of the vertical buttresses is to dissipate forces and transmit them along a vertically oriented vector. In addition, the buttresses also maintain the spatial position of the maxilla in relation to the cranium above and the mandible below.
There are also three horizontal buttresses of the maxillofacial region—the superior, middle, and inferior buttresses (see Fig. 12-1B). The superior horizontal buttress is composed of the orbital plate of the frontal bone and cribriform plate of the ethmoid. The middle horizontal buttress consists of the zygomatic process of the temporal bone, body and temporal process of the zygoma, infraorbital process, orbital surface of the maxilla, and segments of the frontal process of the maxilla. This buttress provides lateral stability to the facial skeleton and protects the central facial skeleton from horizontally directed forces. The inferior horizontal buttress consists of the alveolar ridge and hard palate.4 Because of their functions, realignment and proper reconstruction of the buttresses in three dimensions during repair of maxillofacial fractures is an important step for preserving function and appearance.5
Causes and Classification of Facial Injuries
The most common causes of facial injuries include motor and other vehicular accidents, altercations, falls, and sports- and work-related injuries.4 The degree of force delivered by the impact to the skeletal tissue plays a role in the severity or complexity of the resultant injury. Low-energy forces may cause little comminution or displacement, moderate-energy injuries have an increased chance of fracture displacement, and high-energy injuries could result in highly comminuted fractures, accompanied by dramatic instability and marked alteration in facial skeletal architecture.1 Therefore, the cause of the injury is an important component of the patient’s evaluation and assessment. Knowing the mechanism of the trauma may lead to more specificity in the clinical examination and acquisition of radiographic images and their assessment. Classification of facial injuries is also important to define the treatment better and develop a successful plan. In addition to a thorough clinical examination of the patient, radiographic analysis is extremely helpful in classifying facial injuries and plays a central role in providing essential information for the initial diagnosis and treatment. Maxillofacial injuries can range from isolated fractures involving only one or two osseous structures of the facial skeleton to complex facial injuries involving the entire osseous facial skeleton, with different degrees of displacement. Important clinical and radiographic findings that need to be adequately defined include severity of injury, comminution, bone loss, occlusal disharmony, loss of teeth, alveolar fractures, presence of condylar fracture, displacement of segments, and entrapment of vital structures.
Diagnostic Imaging of Maxillofacial Injuries
Imaging Modalities
Plain Films
Radiographic evaluation of severe facial trauma requires some essential radiographic projections and, although CT with three-dimensional reformatting has become the imaging modality of choice in complex facial trauma, plain films are still widely used in the initial evaluation of the trauma patient. The facial bone series consists of three to five projections, including the lateral cephalic, Caldwell’s lateral oblique, and Waters’ views. The submentovertex (SMV) and Towne’s view can also be obtained to help delineate fractures not seen on the other views (Fig. 12-2).

FIGURE 12-2 Facial series. A, Waters’ view. B, Lateral cephalic view. C, Lateral oblique view. D, SMV view.
Towne’s view is the most useful for assessing subcondylar fractures because it is the only plain radiographic study that optimally demonstrates lateral or medial angulation and/or displacement in these fracture patterns (Fig. 12-3). It is also useful for the evaluation of the orbits because it provides optimal demonstration of the inferior orbital fissure. Towne’s view also provides additional exposure of the maxillary sinuses and inferior orbital rims, aiding in the postoperative evaluation after fracture repair. When Towne’s view is obtained from a posteroanterior (PA) angulation it is useful to evaluate areas such as the petrous ridges and mastoid air cells, as well as the foramen magnum, dorsum sellae, and occipital bone.6 In the reverse Towne’s projection, which is a reverse of the half-axial or Towne’s view, the same fracture patterns seen on the PA Towne’s view can be observed.7
Lateral cephalic views can provide information for evaluation of the airway, retropharyngeal soft tissue, anterior and posterior maxillary antral walls, and anterior alveolar ridge, as well as fractures involving the midface, such as LeFort I, II, and III fractures and nasal fractures (Fig. 12-4). PA films are also useful for evaluating midface and mandibular fractures (Fig. 12-5). The Caldwell view is used for evaluation of the midface and paranasal sinuses and provides the best view of the orbits and posterior facial structures. This view is particularly useful for evaluating the nasofrontal and vertical segments of the zygomatic buttresses, nasal fossa, and mandible. Lateral oblique views can be used for evaluation of the mandibular angle and condyles. Waters’ view is useful for evaluating the midface and delineating fractures of the orbital rims, zygomatic arches, and anterior facial structures. The SMV view provides a good view for zygomatic arch and midface fractures.

FIGURE 12-5 PA view showing evidence of mandibular fracture.
Cervical Spine Films
In cases of facial trauma, cervical spine (C-spine) injuries should be ruled out with a complete cervical spine series, which includes lateral view (cross table), odontoid (open mouth), and oblique views before any manipulation of the neck. Undiagnosed cervical spine injury can occur in 15% to 30% of patients and lateral views have a false-negative rate of 26% to 40%.8 In equivocal clinical cases, CT is recommended because it identifies more fractures and is more accurate in locating the position of bone fragments. CT scans are also recommended for all unconscious patients with suspected neck trauma and all alert conscious patients who complain of neck pain and spasms after high-velocity injuries. CT, however, is not adequate for identifying ligamentous injuries in the cervical spine and, although they can be identified in flexion-extension lateral views, this is a potentially hazardous procedure. It must be done only for alert and cooperative patients with minimal spasm who have no evidence of a potentially unstable fracture on plain film or CT imaging. MRI, on the other hand, can identify ligamentous injuries and should be considered if the previous investigations remain unhelpful or cannot be undertaken.
One of the primary purposes of C-spine imaging is to identify potentially unstable injuries; one of the most helpful classifications of instability has been proposed by Denis.9 This classification divides the spine into three columns (Fig. 12-6):
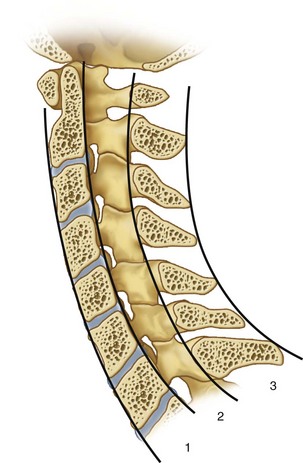
FIGURE 12-6 Denis classification—columns dividing the C-spine in anterior, middle, and posterior segments.
1. Anterior: This is comprised of the anterior longitudinal ligament, anterior disc, and anterior vertebral body.
2. Middle: This is comprised of the posterior longitudinal ligament, posterior disc, and posterior vertebral body.
3. Posterior: This is comprised of the posterior ligamentous complex, pedicles, lamina, and spinous processes.
An injury is considered unstable if two or three columns are disrupted. An alert asymptomatic patient without a distracting injury or neurologic deficit, and who can complete a functional range of motion evaluation, may safely be cleared from cervical spine immobilization, even without radiographic evaluation.10
Computed Tomography
Although plain films will often provide adequate information, CT scans will often yield additional information or can be used when C-spine precautions or other injuries do not permit standard facial films. There is wide agreement that the exact anatomic identification and quantification of facial fractures, recognition of the true extent of bone displacements, and precise assessment of major bone and soft tissue complications can be effectively and accurately imaged with high-resolution CT.11
Since the introduction of CT in the late 1970s and early 1980s, there have been major advancements in the diagnostic imaging of maxillofacial injuries. CT scanning allows for the visualization of injuries of each of the osseous components of the facial skeleton in the axial and coronal planes and allows for the evaluation of various soft tissue injuries. Continued improvements in software have enabled multiplanar reconstruction of image slices in various planes using the digitized data obtained in the initial axial evaluation. These advances in computer technology enable automatic reconstruction of surface models using digitized contour lines and three-dimensional representation on a graphic terminal (Fig. 12-7). Three-dimensional reconstruction of facial bones from two-dimensional images can help guide treatment of facial injuries; in addition to trauma, it is helpful for the evaluation of congenital malformations and pathology.

FIGURE 12-7 Three-dimensional reconstruction from CT scan.
Although two-dimensional CT scans can be helpful when evaluating facial trauma, one of the difficulties is obtaining coronal sections because they require significant movement of the patient’s neck. Thus, the examination is restricted to axial sections and the impossibility of obtaining sagittal sections requires the additional use of conventional tomography.12 Interpretation of three-dimensional reconstruction allows for easier evaluation and the use of three-dimensional images for the assessment of facial injuries ensures a high degree of reliability in morphologic diagnosis.
With the increasing role of CT for the assessment of trauma patients, most clinicians advocate its use. It is considered the gold standard for radiographic evaluation of the facial trauma patient. In the past, the use of traditional or single-slice acquisition CT produced images by data collected from detectors after a 360-degree rotation. After each tomographic image, the patient table was moved and another image obtained. A time delay of 10 to 15 seconds between each slice was necessary, which made image acquisition a slower process. The development of spiral or helical scanning has allowed for faster image acquisition.13,14 Spiral CT involves the simultaneous movement of the patient table and x-ray tube, which results in a volume acquisition of data from which individual tomographic images can be reconstructed. Because a volume data set is acquired, excellent multiplanar reformations are possible when using thin image slices (≤3 mm).9 Thus, spiral CT scanners can rapidly scan acutely traumatized patients in less than 1 minute and can generate direct images in the scan plane and three-dimensional images in a matter of seconds.
Multidetector CT is another improvement over spiral CT; whereas spiral CT uses a single row of detectors, multidetector CT uses a matrix of detectors that allows for the acquisition of multiple tomographic images per revolution, which greatly increases the speed of imaging. Also, fracture detection has been shown to be significantly higher with thin multiplanar reformations.15 These are currently considered state of the art imaging for the patient with severe maxillofacial injuries.
Computed Tomography Angiography
CT angiography (CTA) is an important tool in the maxillofacial field for a variety of indications, ranging from the management of traumatic injuries to the treatment of pathologic conditions such as vascular malformations or vessel aneurysms. CTA in combination with MR angiography (MRA) is highly efficient for the diagnosis of most arterial and venous traumatic lesions in the acute setting and when patients develop delayed symptoms. Conventional angiography is mainly recommended for therapeutic purposes or when the diagnosis remains unclear after performing cross-sectional imaging.16 Taking into consideration that approximately 25% of penetrating injuries to the neck result in vascular injury, in addition to an 80% chance of carotid artery injury and a 43% chance of vertebral artery injury in the trauma patient, the development of vascular imaging techniques has been beneficial for the diagnosis of these injuries.
Additional diagnostic modalities include dacrocystography, ultrasound, and sialography, which become useful in the delayed management of lacrimal/salivary duct injury.17 Currently, multidetector row CT provides isotropic data acquisition, allowing imaging reformats with high resolution. This provides an excellent noninvasive evaluation of the major vascular structures of the head and neck regions. Studies have reported 100% sensitivity and 98% specificity in diagnosing vascular occlusion, pseudoaneurysms, fistulas, and partial thrombosis.7
Magnetic Resonance Imaging
MRI has become the preferred diagnostic tool for examination of the soft tissue structures of the extracranial head and neck. In the early 1980s, the first MRI scan became available after the independent and simultaneous work of Felix Bloch and Edward Purcell in the 1940s, which led to their being awarded the Nobel Prize for Physics in 1956.18
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses