Chapter 12
Preprosthetic Ridge Augmentation: Hard and Soft
HISTORY
In 1983, Seibert (1983a, 1983b) classified the different types of alveolar ridge defects that a clinician may encounter while planning a prosthetic rehabilitation. His classification described the following three clinical situations:
- Class I alveolar ridge defects have a horizontal loss of tissue with normal ridge height.
- Class II alveolar ridge defects have a vertical loss of tissue with normal ridge width.
- Class III alveolar ridge defects have a combination of class I and class II resulting in loss of normal height and width.
The reconstruction of a normal alveolar housing, in height and width, is imperative to achieve a harmonious balance between biology, function, and aesthetics.
INDICATIONS
The indications of alveolar ridge defects occur when the loss of substance compromises the positive outcome of a prosthetic restoration. This is particularly true in the aesthetic zone, and most of the time is caused by periodontal disease, careless tooth extraction, chronic infection, implant failure, congenital diseases, trauma, or neoplasm.
The loss of gingiva or bone can be detrimental to the successful placement of an implant or a fixed partial denture. This loss of substance can be avoided by socket preservation or immediate implant placement, or treated with soft and hard tissue grafting.
When planning treatment for corrective surgery, it is important to inform the patient that a single procedure may not repair the defect, so a second, or sometimes even a third, procedure is sometimes warranted. A Seibert class I defect is easier to treat than a class II, which, in turn, is easier to treat than a class III. A class III defect will require multiple grafting. In addition, the prognosis is better in the case of horizontal defects as opposed to vertical or combined defects.
These defects can be corrected by the following procedures (Table 12.1).
Soft tissue grafts
These are the roll technique (small to moderate class I defects), free gingival onlay grafts (class I, II, and III defects), connective tissue inlay grafts (class I defects), wedge-sandwich grafts (class I and small class II), and soft tissue allografts [AlloDerm (acellular dermal matrix allograft); LifeCell, Branchburg, NJ, USA] for class I, II and III.
Hard Tissue Grafts
These are guided bone regeneration (GBR) with autogenous bone grafts, bone allografts, bone xenografts, synthetic bone substitutes, and block grafts.
Combination of soft and hard tissue grafts
The hard tissue graft used will depend on the extent and severity of the defect and on the type of prosthetic restoration that will follow. When an implant-supported fixed prosthesis is planned, a bone graft is needed with or without a soft tissue graft. However, when a fixed partial denture is planned, a soft tissue graft could be sufficient. It is important to keep in mind that a patient may need more than one surgery to correct a defect. In certain specific cases, procedures such as edentulous ridge expansion (ERE), distraction osteogenesis, and orthodontic treatment can be performed in conjunction with or in lieu of grafting.
ARMAMENTARIUM
This includes a basic surgical kit plus the following:
- Polytetrafluoroethylene sutures [Gore-Tex (W.L.Gore, Flagstaff, AZ, USA), suture CV-5]
- Barrier membranes: resorbable [i.e., Resolut (W.L. Gore), Bio-Gide (Osteohealth, Shirley, NY, USA), or Ossix (3i, Palm Beach Gardens, FL, USA)] and nonresorbable [i.e., Gore-Tex expanded polytetrafluoroethylene (e-PTFE)]
- Bone allograft or substitute [i.e., Regenaform (Exactech, Gainesville, FL, USA), Dembone (Pacific Coast Tissue Bank, Los Angeles, CA, USA), Bio-Oss (Osteohealth), or Cerasorb (Curasan, Research Triangle Park, NC, USA)]
- Acellular Dermal Matrix: AlloDerm (LifeCell)
- Fixation screws: OsteoMed (Dallas, TX, USA)
- Collagen plugs: CollaPlug (Zimmer, Warsaw, IN, USA)
- Purified n-butyl cyanoacrylate glue (PeriAcryl) (GluStitch; Delta, BC, Canada)
TABLE 12.1. Soft tissue versus hard tissue augm entaton
| Soft tissue graftingc | Hard tissue grafting |
| Midto m oderate defects (3mm–6m m ) | M oderate tosevere defects (> 4mm) |
| Horiontaldefects | Horiontaland vertcaldefects |
| Fixed partaldenture | Implanttherapy |
| Availabity of softtissue | Inadequate soft tissue quantity |
| Q uestonable long-term stabity | Stable withtme |
| May need m ultiple augm entations |
SOFT TISSUE GRAFT
Technique
The soft tissue graft technique is particularly well suited when a fixed partial denture restoration is planned (Figs. 12.1 & 12.2). After proper anesthesia has been established, a partial thickness flap is elevated (Fig. 12.3). The horizontal crestal incision is slightly palatal or lingual with two vertical releasing incisions when necessary. Whenever possible, the vertical releasing incisions should be away from the external borders of the anticipated graft.
The partial thickness flap is raised and dissected beyond the mucogingival line to achieve coronal mobility. A connective tissue graft is harvested from the palate (Figs. 12.4 & 12.5), or a piece of AlloDerm is used when there is not enough autogenous tissue available. This graft is inserted under the buccal flap (Fig. 12.6) and secured to the periosteum with resorbable sutures (5-0 chromic gut P-3 needle).
Figure 12.1. Seibert class I defect.The gingival buccal concavity needs to be augmented for a better aesthetic outcome.The restoration planned here is a fixed partial denture; hence the need for a soft tissue graft only.

Figure 12.2. Occlusal view without the temporary restoration.

Figure 12.3. The horizontal incision is made and continued intrasulcularly to teeth 9 and 11. This helps with the sharp dissection and mobilizes the flap. An alternative would be to put two vertical incisions on each side of the area to be augmented.
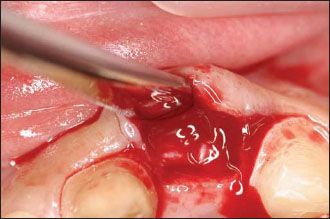
Figure 12.4. A trapdoor is opened in the palate to harvest the connective tissue graft to be used to correct the defect.

Figure 12.5. The harvest of the piece of connective tissue.The desired length and thickness have been determined by the size and shape of the defect to be corrected.
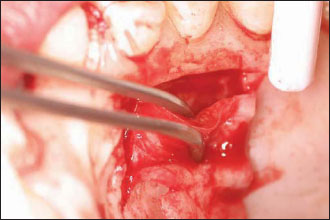
Figure 12.6. The graft is inserted and positioned into the wound. It will be secured to the periosteum bucally with an intraperiosteal horizontal mattress resorbable suture.
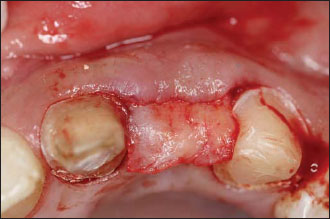
Figure 12.7. Once the connective tissue graft has been secured, the flaps are secured using single interrupted sutures.

Figure 12.8. Buccal view of the augmented site 2 weeks after the surgery.


The partial thickness flap is then mobilized and coronally pulled to cover the graft. Single interrupted sutures are used to close the wound by primary intention (Fig. 12.7). It is advisable to keep the sutures in place for 2 weeks to ensure enough healing of the site (Figs. 12.8–12.10).
CLINICAL CROWN REDUCTION USING A CONNECTIVE TISSUE GRAFT
Use this technique when the crown preparation extends too far apically with or without a lack of attached gingiva (Figs. 12.11–12.20).
HARD TISSUE GRAFT
Hard tissue grafts are primarily used when an implant-supported restoration is planned. The hard tissue augmentation can be done with block grafts (autografts and allografts), particulate grafts (cort/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


