Physical and Chemical Injuries of the Oral Cavity
 . Injuries of Teeth Associated with Tooth Preparation
. Injuries of Teeth Associated with Tooth Preparation
 . Reaction To Rotary Instrumentation
. Reaction To Rotary Instrumentation
 . Effect of Restorative Materials
. Effect of Restorative Materials
 . Physical Injuries of the Teeth
. Physical Injuries of the Teeth
 . Physical Injuries of the Bone
. Physical Injuries of the Bone
 . Physical Injuries of Soft Tissues
. Physical Injuries of Soft Tissues
 . Nonallergic Reactions to Drugs and Chemicals used Systemically
. Nonallergic Reactions to Drugs and Chemicals used Systemically
Injuries of Teeth Associated with Tooth Preparation
Reaction to Rotary Instrumentation
Stainless steel burs revolving at low speed were used in the past for cavity and crown preparation. As the hardness of the enamel is high, these burs could not abrade instead they cut or chip away the tooth material. Also a considerable amount of pressure is applied during the procedure, which results in excessive heat production and evaporation of the contents of the dentinal tubules. High speed rotary instrumentation with tungsten carbide and diamond burs has replaced the steel burs in recent years. Nevertheless stainless steel burs are used in procedures involving bone.
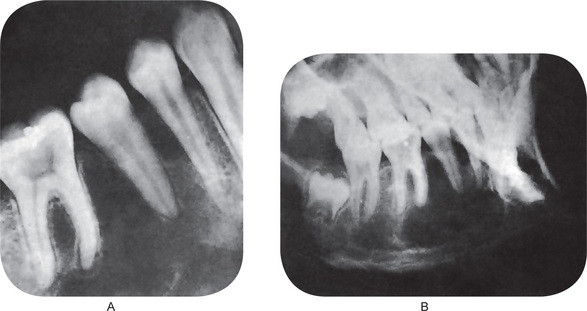
The pulp reaction to superficial injury of the dentin varies in degree of severity, depending partially upon the depth of the prepared cavity and partially upon the elapsed time between cutting the cavity and extraction of the tooth for study. In mild reactions the odontoblasts become distorted and reduced in number. Small vacuoles may appear between them, probably lymph exudate. Capillaries in the damaged area may be prominent. In more severe injuries, there may be complete disorganization of and hemorrhage in the odontoblastic layer (Fig. 12-1). The bulk of the pulp tissue away from the cut tubules may exhibit little or no reaction.
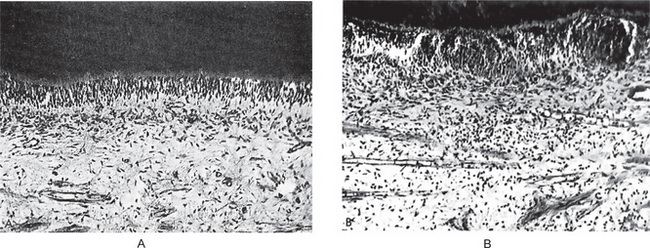
Figure 12-1 Effect on dental pulp of cavity preparation by steel bur.
Cavities were prepared in human teeth and filled with gutta-percha. A section of pulp from an intact normal tooth is shown in (A), while the injured area in the pulp six days after cavity preparation is seen in (B) Courtesy of Drs David F Mitchell and Jensen JH. J Am Dent Assoc, 55:57, 1957.
Even after such severe injuries the majority of damaged pulps undergo spontaneous healing or at least enter a quiescent phase and produce no signs or symptoms of persisting damage (Fig. 12-2). The factors responsible for this phenomenon, especially from the clinical aspect, are unknown.
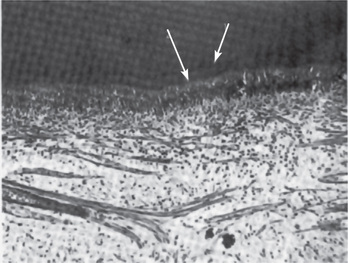
Figure 12-2 Effect of cavity preparation by steel bur on dental pulp.
A calciotraumatic line (1) and reparative dentin (2) are found beneath the cavity nine weeks after preparation Courtesy of Drs David F Mitchell, JH Jensen. J Am Dent Assoc, 55: 57, 1957.
It appears that dentin has a heat-dissipating action which reduces the temperature rise within the pulp to only a fraction of the actual temperature applied to the tooth. This is due to the low thermal conductivity of dentin, which acts as an effective insulating medium. Nevertheless the application of heat to a dental pulp already injured from a carious lesion of the dentin, but not an actual pulp exposure, may be sufficient to affect adversely the repair or healing of the pulp even though an apparently successful restoration is given to the tooth.
Lasers
Laser is an acronym for Light Amplification by Stimulated Emission of Radiation. It is an electro-optical device which, upon stimulation, can convert jumbles of light waves into an intense, concentrated, uniform, narrow beam of monochromatic light with an energy source of great intensity and exceptional flexibility. The radiation may be continuous or modulated, or the emission may occur in short pulses. This high-intensity radiation can be focused on an extremely small area, approximately 1 micron in diameter, because of the small angle of divergence and coherency of the beam. Light photons of characteristic wavelengths are produced, amplified, and filtered to produce the laser beam. Carbon dioxide and neodymium:yttrium-aluminum-garnet (Nd:YAG) lasers are most commonly used. The main problem with laser cutting of hard dental tissues is the generation of heat and forbidden tactile control.
Effect of Restorative Materials
Glass-ionomer
Conventional Composite Resins
These are restorative materials developed chiefly because methyl methacrylate or unfilled acrylic resins have restrictive characteristics such as low hardness and strength, a high coefficient of thermal expansion and a lack of adhesion to tooth structure. The resin matrix is a compromise between epoxy and methacrylate resins. This resin is combined with a filler of dispersed particles of varying types in relatively high concentration. While most conventional composite resins are chemically activated, some are now marketed whose cure is based on light activation.
Microfilled Composite Resins
The many experimental studies cited would indicate superficially that the majority of restorative materials used in dentistry today are dangerous because of the serious effects on the dental pulp which they often induce. It is true that many of these materials are potentially injurious. Nevertheless, literally millions of restorations with these substances are placed each year, and clinical experience has shown that, unless actual pulp exposure has occurred, the death rate of dental pulps directly attributable to the restorative material is extremely low. Even the occurrence of clinical symptoms of pulp injury is uncommon. Although this seems contradictory to experimental evidence, it should be appreciated that most cavities prepared by the dentist in which these materials are inserted are to repair a destructive carious lesion. The presence of this carious lesion, in contrast to the experimental cavities prepared in sound human and animal teeth, has usually induced the deposition of secondary dentin and has caused a certain amount of dentinal sclerosis, and these reactions offer considerable protection to the pulp. It is on this basis that the dentist is justified in continuing to use these filling materials. There is a need, however, for continued study of this general problem.
Effect of Cement Bases, Cavity Liners, Varnishes and Primers
• To serve as a bacteriostatic agent.
• To provide thermal insulation, particularly under metallic restorations.
• To provide electrical insulation under metallic restorations.
• To prevent discoloration of tooth structure adjacent to certain types of restorative materials.
• To prevent the penetration of deleterious constituents of restorative materials into the dentin and pulp.
• To improve the marginal seal of certain restorative materials by preventing microleakage and the ingress of saliva and debris along the tooth-restoration interface.
Cavity Liners
Cavity liners are aqueous or volatile organic liquid suspensions or dispersions of zinc oxide or calcium hydroxide that can be applied in a relatively thin film to the surface of a cavity. They may also be solutions of resins in an organic solvent to which has been added calcium hydroxide or zinc oxide, or aqueous suspensions of calcium hydroxide in methylcellulose. The cavity liner provides the beneficial effects of zinc oxide and calcium hydroxide as thin films in shallow cavities and, in addition, neutralizes the free acid of zinc phosphate and silicate cements. The cavity liners themselves have no effect on dental pulp and, in fact, actually form a chemical barrier to provide reliable protection for the pulp under certain deep restorations.
Physical Injuries of the Teeth
Bruxism: (‘Night-grinding’, bruxomania)
Etiology
Local factors are generally associated with some form of mild occlusal disturbance which produces mild discomfort, and chronic, even though unrecognized, tension. It has been suggested that in many cases bruxism becomes a firm habit as a result of an unconscious attempt by the patient to establish a greater number of teeth in contact or to counteract a local irritating situation. In children the habit is frequently associated with the transition from the deciduous to the permanent dentition and may result from an unconscious attempt to place the individual tooth planes so that the musculature will be at rest.
Fractures of Teeth
Clinical Features
Although fracture of teeth may occur at any age, children are especially prone to sustain this type of injury. The prevalence of tooth fracture is difficult to assess or evaluate, particularly since minor chipping of teeth is common. As might be expected, boys are more frequently involved than girls. There is a definite predilection for involvement of maxillary teeth, with between 75 and 90% of fractures occurring there (Fig. 12-3).
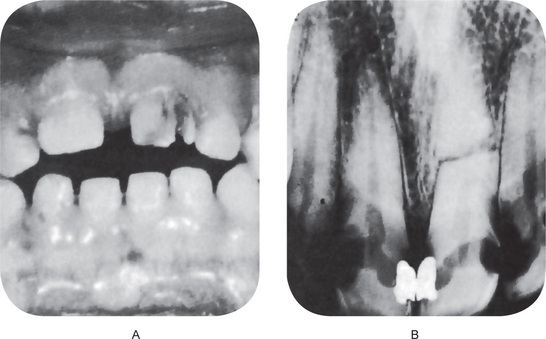
Figure 12-3 Fractured teeth after traumatic injury.
(A) Fracture of crown with pulp exposure. (B) Root fracture.
Class 1: Simple fracture of the crown, involving little or no dentin.
Class 2: Extensive fracture of the crown, involving considerable dentin but not the dental pulp.
Class 3: Extensive fracture of the crown, involving considerable dentin and exposing the dental pulp.
Class 4: The traumatized tooth becomes nonvital, with or without loss of crown structure.
Class 5: Teeth lost as a result of trauma.
Class 6: Fracture of the root, with or without loss of crown structure.
Class 7: Displacement of a tooth, without fracture of crown or root.
Class 8: Fracture of the crown en masse and its replacement.
Cracked Tooth Syndrome
Cracked tooth syndrome (CTS) is characterized by sharp pain on chewing without any obvious reason, which is actually caused by a ‘hidden’ crack of the tooth. These are incomplete fractures that are too small to be seen on radiographs. The typical symptom is sharp fleeting pain when releasing biting pressure on an object. This is because when biting down, the segments are usually moving apart and thereby reduce the pressure in the nerves of the pulp. When the bite is released, the ‘segments’ snap back together sharply increasing the pressure causing pain. The pain is often inconsistent, and frequently hard to reproduce. Causes of CTS include attrition, bruxism, trauma, accidental bitting on a hard object, presence of large restoration, and improper endodontic treatment. The American Association of Endodontists have classified five specific variations of cracked teeth; craze line, fractured cusp, cracked tooth, split tooth, and vertical root fracture.
Abrasion
Wearing away of tooth substance due to mechanical means is known as abrasion. The most common cause is the faulty brushing techniques. Habits such as opening the hairpin constantly using anterior teeth, holding bobby pins, and holding pipe also produce a characteristic form of abrasion. This is described in Chapter 13 on Regressive Alterations of the Teeth.
Injuries to the Supporting Structures of the Tooth
Treatment consists of selective grinding of the tooth to eliminate occlusal forces.
Tooth Ankylosis
Fusion between the tooth and bone, termed ankylosis is an uncommon phenomenon in the deciduous dentition and even more rare in permanent teeth. The condition of deciduous tooth ankylosis (submerged tooth) has been described in Chapter 1 on Developmental Disturbances of Oral and Paraoral Structures.
Physical Injuries of the Bone
The most common physical injury involving the bone is fracture.
Traumatic Cyst: (Solitary bone cyst, hemorrhagic cyst, extravasation cyst, unicameral bone cyst, simple bone cyst, idiopathic bone cavity)
Etiology
It is not at all unusual; however, for the patient to be unable to recall any traumatic injury to the jaw. This may indicate that an injury so mild that the patient would not be aware of it or remember it, is sufficient to cause this lesion to develop. In the series reported by Howe, only slightly over 50% of the patients gave a history of trauma, the time lag between injury and discovery of the lesion varying from one month to 20 years.
Other theories of origin, reviewed by Whinery, have included:
• Cystic degeneration of primary bone tumors.
• A result of faulty calcium metabolism such as that induced by parathyroid disease.
• Ischemic necrosis of fatty marrow.
• The end result of a low-grade chronic infection.
• A result of osteoclasis resulting from a disturbed circulation caused by trauma creating an unequal balance of osteoclasis and repair of bone.
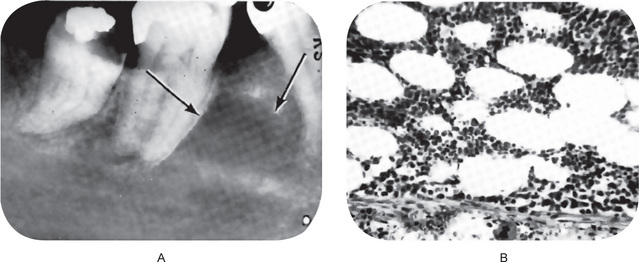
Radiographic Features
Radiographic examination usually reveals a rather smoothly outlined radiolucent area of variable size, sometimes with a thin sclerotic border, depending upon the duration of the lesion. Some traumatic cysts may measure only a centimeter in diameter (Fig. 12-5), whereas others may be so large that they involve most of the molar area of the body of the mandible as well as part of the ramus. When the radiolucency appears to involve the roots of the teeth, the cavity may have a lobulated or scalloped appearance extending between the roots of these teeth (Fig. 12-6). Seldom is there any displacement of teeth and, in many cases, the lamina dura appears intact. Rodrigues and Estrela reported a case of traumatic bone cyst in upper premolar-molar region, mimicking a large periapical lesion.
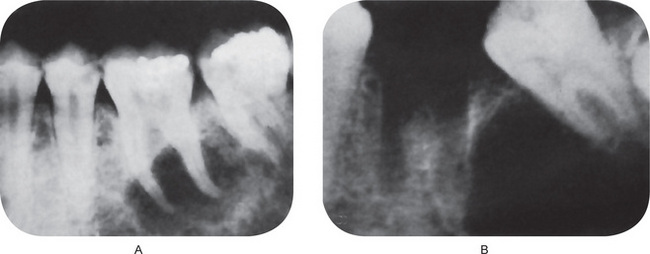
Figure 12-5 Traumatic bone cyst.
The radiolucent area in both cases was entirely empty and devoid of any lining. The molar teeth were vital.
Histologic Features
Histologic examination of the solitary bone cyst may reveal a thin connective tissue membrane lining the cavity, but no other significant features. Sometimes no such membrane is demonstrable. Waldron had the opportunity to study a solitary bone cyst in toto in a resected mandible. His case exhibited a thin connective tissue membrane and, in addition, an extensive osteophytic reaction on the outer surface of the cortical plate (Fig. 12-7). There may be presence of few red blood cells, blood pigments, or giant cells adhering to the bone surface.
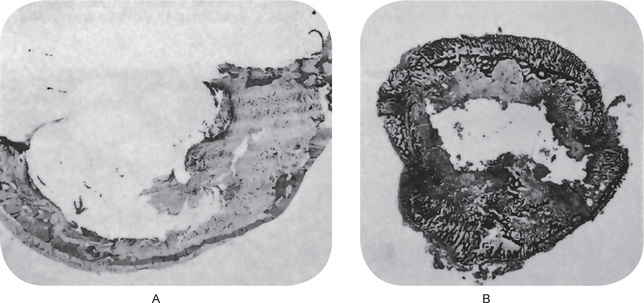
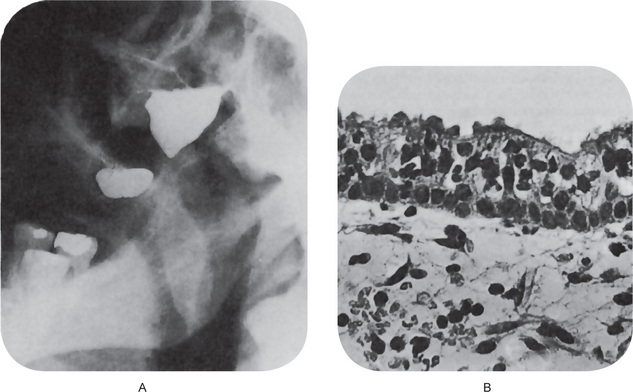
Figure 12-7 Traumatic bone cyst.
Traumatic cyst of mandible (A) and fibula (B). Only a thin shell of the cortical plates of the jaw remains with limited peripheral osteophyte reaction. The fibula shows a similar empty central cavity and thinning of the cortex, although osteophyte reaction is pronounced A, Courtesy of Dr Charles A Waldron and B, of Dr William C Sprague.
Treatment and Prognosis
Since the definitive diagnosis of the solitary bone cyst cannot be established without surgical exploration, the dentist usually opens into the cavity, attempts to enucleate a lining and, in the course of manipulation, reestablishes bleeding into the lesion. If the cavity is then closed, it has been found that healing and filling of the space by bone occur in most cases in 6–12 months. Seldom is a second surgical procedure necessary. If the space is a large one, bone chips have been used to aid in filling the defect with good results.
Focal Osteoporotic Bone-marrow Defect of the Jaw
The focal osteoporotic bone-marrow defect of the jaw is an uncommon lesion producing a focal radiolucency away from normal hematopoietic marrow. Hematopoietic marrow occurs normally in the jaws at the angle of the mandible, the maxillary tuberosity and occasionally other areas. It is well recognized that bone marrow may be stimulated in response to unusual demands for increased blood cell production and that this hyperplastic marrow may extend between adjacent trabeculae of bone, producing radiographically obvious osteoporosis and even thinning of the cortex. Other views regarding its pathogenesis include abnormal healing following tooth extraction since these lesions are most common in extracted sites, and persistence of remnants of fetal marrow.
Radiographic Features
This lesion, which has a predilection for the mandibular molar area, generally appears as a radiolucency of variable size, a few millimeters to a centimeter or more, with a poorly defined periphery indicative of lack of reactivity of adjacent hone (Fig. 12-8A).
Histologic Features
The tissue removed from these defects consists of either normal red marrow, fatty marrow or a combination of the two (Fig. 12-8B). Megakaryocytes and small lymphoid aggregates may be present. The trabeculae of bone usually present in the sections are long, thin, irregular, and devoid of an osteoblastic layer.
Surgical Ciliated Cyst of Maxilla: (Sinus mucocele)
Clinical Features
Radiographic Features Radiographic examination shows a well-defined unilocular radiolucent area closely related to the maxillary sinus, often appearing to encroach upon the sinus but anatomically separate from it, as may be demonstrated by injection of the sinus with a radiopaque material. A filling defect of the cyst can then be seen (Fig. 12-9A).
Histologic Features
The surgical cyst is lined by pseudostratified ciliated columnar epithelium identical with that of the maxillary sinus (Fig. 12-9B). If infection or inflammation is present, squamous metaplasia may be found. The wall of the cyst is composed of fibrous connective tissue with or without inflammatory cell infiltration.
Effects of Orthodontic Tooth Movement
The science of orthodontics is based upon the ability of teeth to be moved through bone, without their subsequent extrusion or loss, by the application of pressure or tension under appropriate and controlled circumstances. Although the exact biologic mechanism responsible for this phenomenon is unknown, it is generally agreed that bone under pressure responds by resorbing, whereas the application of tension results in deposition of new bone. The periodontal ligament transfers the pressure or tension applied through orthodontic appliances.
Tipping Movement
The exact movements which a tooth will undergo and the exact position it will assume after the application of orthodontic force will depend upon the degree and direction of the force and the position of the fulcrum around which the force acts. The general statement can be made, however, that pressure upon a tooth results in the resorption of bone in the direction of the application of force and compensatory new bone formation on the opposite side of the tooth, the tension side (Fig. 12-10).
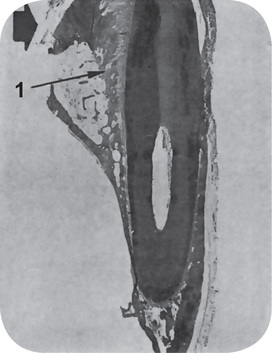
Figure 12-10 Tipping tooth movement.
Force was applied to this dog’s tooth in the direction of the arrow, and even at this magnification, widening of the periodontal ligament space (1) is noted.
The initial reaction on the pressure side is a compression of the periodontal ligament which, if excessive and prolonged, may result in ischemia with hyalinization and/or actual necrosis of tissue (Fig. 12-11B). On the opposite side under excessive force there may be actual tearing of the periodontal fibers and small capillaries with hemorrhage into the area. With reasonable forces, the periodontal ligament on the tension side of the tooth demonstrates stretching and widening of the periodontal space. Within a matter of hours or at the most a few days, large numbers of osteoclasts make their appearance along the surface of the bone under pressure, and resorption begins. This continues until the force of the pressure has been entirely dissipated.
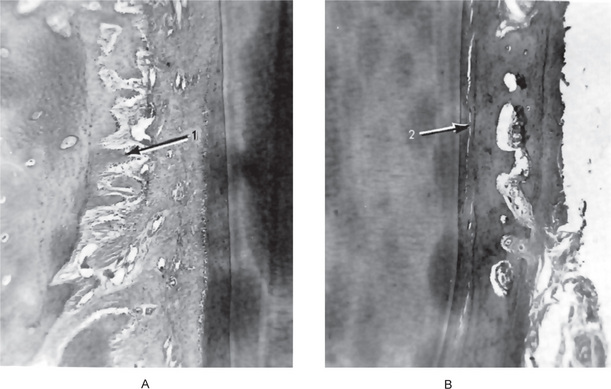
Figure 12-11 Tipping tooth movement.
There is widening of the periodontal ligament with formation of new spicules of bone (1) on the tension side of the tooth (A) and compression of the periodontal ligament (2) on the pressure side (B).
New trabeculae of bone on the tension side become evident early and appear as thin, elongated spicules arranged parallel to the periodontal fibers and confluent with them at their bony attachment (Fig. 12-11A). These spicules show evident osteoblastic activity along the sides and the end adjacent to the tooth, but usually there is intense osteoclastic activity at the ends of the spicules away from the tooth. As stabilization occurs, the alveolar bone gradually assumes its compact pattern that existed before movement occurred.
Tissue Reactions during Retention Period
Discontinuance of the active phase of orthodontic force signals the beginning of alterations in the bone characteristic of the retention period. During this period there is gradual reformation of the normal dense pattern of the alveolar bone by apposition of bone around the bony spicules until they meet, fuse, and gradually remodel. The studies of Oppenbeim indicated that this reformation is slower around teeth held in position during the retention period by a retaining appliance as compared to teeth which remained free during this time. In any event, the final remodeling and the attainment of absolute bone-tooth equilibrium following orthodontic movements involve an extremely slow process, and a breakdown in this process is probably one of the most important contributing factors in cases of orthodontic failure due to relapse during the retention period.
Physical Injuries of Soft Tissues
Linea Alba
Linea Alba is a white line seen on the buccal mucosa extending from the commissures posteriorly at the level of the occlusal plane (Fig. 12-12). It is caused by the physical irritation and pressure exerted by the posterior teeth. It is usually bilateral and is more pronounced in persons who have clenching habit or bruxism. Histologically hyperkeratosis and intracellular edema of the epithelium is seen.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 . Effect of Tooth Preparation
. Effect of Tooth Preparation . Effect of Heat
. Effect of Heat . Occupational Injuries of the Oral Cavity
. Occupational Injuries of the Oral Cavity . Occlusal Trauma
. Occlusal Trauma