chapter 12
Pains of Muscle Origin
Pains of muscular origin are the most frequent cause of discomfort about the head and neck. Very few humans have escaped this type of pain experience. Since dental pain is the most frequent oral pain, a good rule to follow in diagnosing pains about the face and mouth is initially to assume that it is dental until proved otherwise, then muscular until proved otherwise. The possibility of orofacial pain being of muscular origin should be taken into account with every complaint. Even when the primary cause is not muscular, central excitatory effects tend to be expressed in the muscles, which makes this a frequent complication accompanying other sources of pain.
Muscle pain emanates from the skeletal muscles, tendons, and fascia. Although the exact origin of this type of muscle pain is debated, some authors suggest it is related to vasoconstriction of the relevant nutrient arteries and the accumulation of metabolic waste products in the muscle tissues. Within the ischemic area of the muscle, certain algogenic substances (eg, bradykinins, prostaglandins) are released, causing muscle pain.1,2,3
Muscle pain, however, is far more complex than simple overuse and fatigue. In fact, muscle pain associated with the muscles of mastication does not seem to be strongly correlated with increased activity, such as spasm.4,5,6,7,8 It is now appreciated that muscle pain can be greatly influenced by central mechanisms,9,10 as will be discussed later in this chapter.
Muscle pain usually is felt as a nonpulsatile, variable, dull, aching sensation, sometimes with a boring quality. This more constant background discomfort may escalate to or be punctuated by sharper, more severe lancinating pains occurring both spontaneously and in response to stretching, contraction, manipulation, or manual palpation. Sometimes the pain is no more than a feeling of pressure. At other times, it may increase to excruciating intensity. It may be transitory or persistent, constant, intermittent, or recurrent. Its behavior is labile, characterized by suddenness of onset and rapidity of change. It follows no time frame unless it has an inflammatory origin, which is relatively rare. Accompanying dysfunction may be expressed as tightness and weakness, or it may relate to impairment of muscle function, for example, stiffness, rigidity, swelling, or shortening. Pain decreases the biting strength of masticatory muscles by 33% to 50%11 and induces a feeling of muscular weakness. Muscle pain also impairs the proprioceptive feedback mechanism, thus leading to less precise muscle action.12 Palpable muscle tenderness and the fact that movement and functioning modify the pain and stiffness are clinical indications of the presence of muscle pain.13
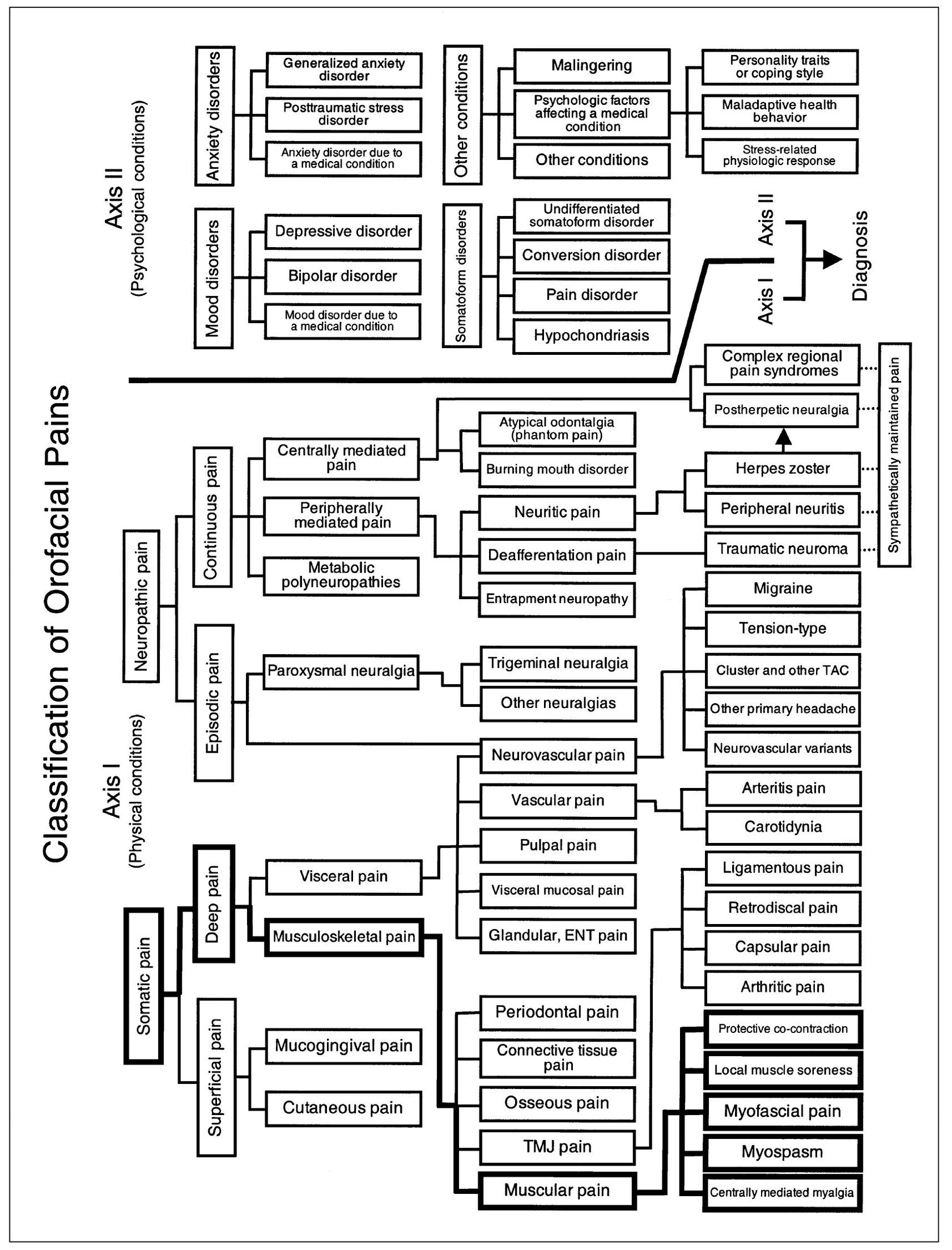
Fig 12-1 Pain classification chart highlighted to show the relationship of muscular pains to other orofacial pain disorders.
Myogenous pains of different types may involve muscles of the mouth, face, and neck, with the symptom complex depending on the kind, number, and location of muscles involved and the degree to which they are affected. The likelihood of secondary central excitatory effects should be considered. When the primary pain remains relatively silent, the secondary referred pain may constitute most of the complaint. Referred pain from muscles can be the source of considerable diagnostic confusion. For example, more or less silent pain arising in the sternocleidomastoid muscle may be felt in and about the ear as earache or as temporomandibular joint (TMJ) pain. Cardiac muscle pain may be referred to the mandible.14
Behavior of Muscular Pain
Myogenous pains that emanate from the orofacial structures are classified as musculoskeletal pains of the deep somatic category (Fig 12-1). The general features exhibited by muscle pain include those of deep somatic pain, namely: (1) the pain has a dull, depressing quality; (2) subjective localization is variable and somewhat diffuse; (3) the site of pain may or may not identify the correct location of the source of pain; (4) response to provocation at the site of pain is fairly faithful in incidence and intensity, but not in location; and (5) central excitatory effects often accompany the pain. To these features are added characteristics peculiar to musculoskeletal pain, namely: (1) the pain relates reasonably to the demands of biomechanical function, and (2) manual palpation at the site of pain, or functional manipulation, produces a graduated response of pain that is proportionate to the stimulus.
The stimulation of skeletal muscle tissue induces a dull, aching pain felt deeply and diffusely in a broad region of the muscle. It is mediated by group III (A-delta fiber) and group IV (C-fiber) afferent neurons. A crescendo of intensity indicates some temporal summation.15 Regardless of the true source of muscle pain, movements that actively stretch the muscle or increase its isometric tension increase the patient’s awareness of pain. If passive movement is painful, one or more antagonists should be suspected of containing an abnormally tender muscle region.16
The term temporomandibular disorders (TMD) refers to a collective term embracing a number of clinical problems that involve the masticatory musculature, the TMJ and associated structures, or both.17 Pain associated with TMD therefore originates from either muscle or joint sources. This chapter will highlight muscle pain, which is by far the most common type of TMD. TMJ pain will be discussed in the next chapter.
When masticatory muscle pain is present, the patient reports discomfort about the face and mouth that is induced by chewing and other jaw use but is independent of local disease involving the teeth and oral cavity proper.
Types of Masticatory Muscle Pains
Not all masticatory muscle disorders are the same clinically. There are at least five different types, and it is important to develop the ability to distinguish among them, because the treatment of each is quite different. The five types are protective co-contraction (muscle splinting), local muscle soreness, myofascial (trigger point) pain, myospasm, and chronic centrally mediated myalgia. A sixth condition known as fibromyalgia also needs to be discussed. The first three conditions (protective co-contraction, local muscle soreness, and myofascial pain) are commonly seen in the dental office. Myospasm and chronic centrally mediated myalgia are seen less frequently. Many of these muscle disorders occur and resolve within a relatively short period of time. When these conditions are not resolved, more chronic pain disorders may result. Chronic masticatory muscle disorders become more complicated, and treatment is generally oriented differently than for acute problems. It therefore becomes important that the clinician be able to differentiate acute muscle disorders from chronic muscle disorders so that proper therapy can be applied. Fibromyalgia is a chronic myalgic disorder that presents as a systemic musculoskeletal pain problem; it needs to be recognized by the dental practitioner and is best managed by referral to appropriate medical personnel.
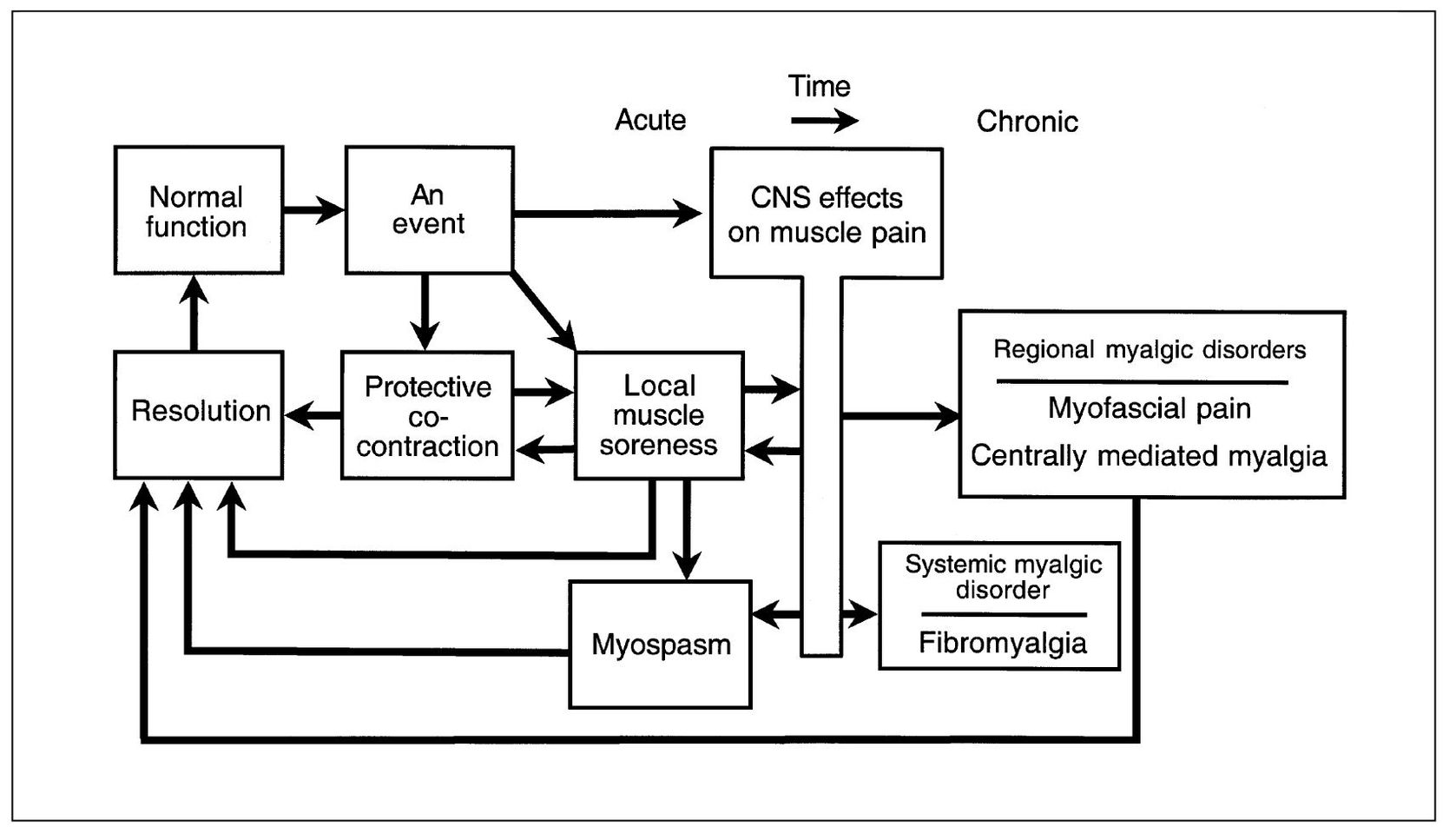
Fig 12-2 A masticatory muscle pain model. This model depicts the relationship between various clinically identifiable muscle pain disorders along with some etiologic considerations. (From Okeson JP. Management of Temporomandibular Disorders and Occlusion, ed 5. St Louis: Mosby, 2003:194. Used with permission.)
Masticatory Muscle Pain Model
To understand the relationship between different muscle pain disorders, a masticatory muscle pain model will be presented (Fig 12-2). Once the model is presented and the clinical characteristics of each subcategory of muscle pain described, the management of each condition will be explained. The model begins with the assumption that the muscles of mastication are healthy and functioning normally. Normal muscle function can be interrupted by certain types of events. If an event is significant, a muscle response occurs, known as protective co-contraction (muscle splinting). In many instances the consequence of the event is minor and the co-contraction quickly resolves, allowing muscle function to return to normal. If, however, protective co-contraction is prolonged, local biochemical and later structural changes can occur, creating a condition known as local muscle soreness. This condition may resolve spontaneously with rest or may require treatment.
If local muscle soreness does not resolve, changes in the muscle tissues may develop, resulting in prolonged pain input. This constant deep pain input can affect the central nervous system (CNS), leading to certain muscle responses. Two examples of CNS-influenced muscle pain disorders are myofascial pain and myospasm. In some instances, the CNS responds to certain events or local conditions by inducing an involuntary contraction, seen clinically as a muscle spasm. Myospasms are not chronic but instead represent a condition of relatively short duration. At one time, myospasm was thought to be the primary condition responsible for myalgia. Recent studies8,18,19,20,21 suggest that true myospasms are not common in patients suffering from masticatory muscle pain.
These masticatory muscle disorders usually present as relatively acute problems and, once identified and treated, the muscle returns to normal function.22 If, however, these acute myalgic disorders are not recognized or appropriately managed, certain perpetuating conditions can advance the problem into a more chronic myalgic disorder. As the myalgic disorder becomes more chronic, the CNS contributes more to maintaining the condition. Because the CNS is an important factor in this condition, it is referred to as centrally mediated myalgia. Chronic centrally mediated myalgia is often very difficult to resolve, and treatment strategies must be changed from those used with the acute myalgic disorders.
Another example of a chronic musculoskeletal pain disorder is fibromyalgia. Although this is not primarily a masticatory pain disorder, the dental clinician needs to recognize this condition so as to avoid unnecessary dental therapy. Unlike the other muscle pain disorders, which are regional, fibromyalgia is a widespread, global musculoskeletal pain condition. Dental practitioners need to be aware that the management of these chronic pain disorders is quite different from that of the relatively acute muscle disorders.
To better understand the masticatory muscle pain model, each component of the model will be discussed in detail.
An Event
Normal muscle function can be interrupted by various types of events. These events can arise from either local or systemic factors. Local factors represent any events that acutely alter sensory or proprioceptive input in the masticatory structures, for example, the fracture of a tooth or the placement of a restoration in supraocclusion. Trauma to local structures, such as tissue damage caused by a dental injection, represents another type of local event. Trauma might also arise from excessive or unaccustomed use of masticatory structures, such as chewing unusually hard food or chewing for a long period of time (eg, gum chewing). Opening too wide may strain the ligaments supporting the joint and/or muscles. This may occur as a result of a long dental procedure or even by simply opening too wide (eg, yawning).
Any source of constant deep pain input may also represent a local factor that alters muscle function. This pain input may have its source in local structures such as the teeth, joints, or even the muscles themselves. The source of the pain, however, is not significant, since any constant deep pain, even idiopathic pain, may create a muscle response.
Systemic factors may also represent events that can interrupt normal muscle function. One of the most commonly recognized systemic factors is emotional stress.23,24,25,26 Stress seems to alter muscle function, either through the gamma efferent system to the muscle spindle or by means of sympathetic activity to the muscle tissues and related structures.27,28,29 Of course, responses to emotional stress are quite individualized. Therefore, patients’ emotional reactions and psychophysiologic responses to stressors may vary greatly. It has been demonstrated that exposure of a subject to an experimental stressor can immediately increase the resting electromyographic (EMG) activity of masticatory muscles. 8,18 This physiologic response provides direct insight about how emotional stress directly influences muscle activity and muscle pain.
Other systemic factors can influence muscle function and are more poorly understood, such as acute illness or viral infections. Likewise, there is a broad category of poorly understood constitutional factors that are unique to each patient. Such factors include immunologic resistance and autonomic balance of the patient. These factors seem to reduce the individual’s ability to resist or combat the challenge or demand created by the event. Constitutional factors are likely to be influenced by age, gender, diet, and perhaps even genetic predisposition. Clinicians realize that individual patients often respond quite differently to similar events. It is assumed, therefore, that certain constitutional factors do exist and can influence an individual’s response. At this time these factors are poorly understood and not well defined as they relate to muscle pain disorders.
As with local factors, constant deep pain input can represent a systemic factor that may influence muscle function. Although pain is often felt in local structures, it may not necessarily have its source in these same structures. As mentioned in earlier chapters, pain can be felt not only as a result of peripheral causes, but as a result of a CNS effect.30 The CNS has the ability to alter pain sensations, both moving toward and away from the cortex.31,32 If the CNS enhances sensory input, pain may be felt even without organic cause. This pain modulation phenomenon can create a site of pain felt in muscle tissues. One must appreciate, therefore, that this pain modulation phenomenon can represent a systemic event that produces muscle pain and ultimately affect function.
Protective Co-contraction (Muscle Splinting)
The first response of the masticatory muscles to one of the previously described events is protective co-contraction. Protective co-contraction is a CNS response to injury or threat of injury. This response has also been called protective muscle splinting.33 It has been described for many years but only recently documented.34,35,36,37,38 In the presence of an injury or threat of injury, normal sequencing of muscle activity seems to be altered so as to protect the threatened part from further injury. Protective co-contraction can be likened to the co-contraction39 observed during many normal functional activities, such as bracing the arm when attempting a task with the fingers. In the presence of altered sensory input or pain, antagonistic muscle groups seem to fire during movement in an attempt to protect the injured part. In the masticatory system, for example, a patient experiencing co-contraction will demonstrate an increase in the activity of the elevator muscles during mouth opening.34,40,41 During closing of the mouth, an increase in activity is noted in the depressing muscles. This co-activation of antagonistic muscles is thought to be a normal protective or guarding mechanism and needs to be recognized by the clinician. Protective co-contraction is not a pathologic condition, although it may lead to muscle symptoms when prolonged.
The etiology of protective co-contraction can be any change in sensory or proprioceptive input from associated structures. An example of such an event in the masticatory system is the placement of a high crown. Protective co-contraction can also be caused by any source of deep pain input or an increase in emotional stress.
Co-contraction is reported clinically as a feeling of muscle weakness directly following some event. There is no pain reported when the muscle is at rest, but use of the muscle usually increases the pain. The patient often presents with limited mouth opening, but when asked to open slowly, he or she can achieve full opening. The key to identifying co-contraction is that it immediately follows an event; therefore, the history is very important. If protective co-contraction continues for several hours or days, the muscle tissue can become compromised and a local muscle problem may develop.
Local Muscle Soreness
Local muscle soreness is a primary, noninflammatory, myogenous pain disorder. It is often the first response of the muscle tissue to prolonged co-contraction. While co-contraction represents a CNS-induced muscle response, local muscle soreness represents a condition that is characterized by changes in the local environment of the muscle tissues. These changes are characterized by the release of certain algogenic substances (ie, bradykinin, substance P, even histamine42) that produce pain. These initial changes may be expressed as nothing more than fatigue. Along with protracted co-contraction, other causes of local muscle soreness are local trauma or excessive use of the muscle. When excessive use is the etiology, a delay in the onset of muscle soreness can occur.43 This type of local muscle soreness is often referred to as delayed-onset muscle soreness or postexercise muscle soreness.44
Since local muscle soreness itself is a source of deep pain, an important clinical event can occur. Deep pain produced by muscle soreness can, in fact, produce protective co-contraction. This additional co-contraction can, in turn, produce more muscle soreness. Therefore, a cycle can be created whereby muscle soreness produces more co-contraction and so on. This condition is called cyclic muscle pain and needs to be recognized by the clinician. The important feature of this condition is that the pain condition becomes wholly independent of the original source of pain. If the clinician attempts to continue to treat the original cause, the pain condition will not be resolved. This concept is very often overlooked or not appreciated by the clinician, but it is basic to successful management of muscle pain.
The clinician needs to be aware of the complications that cyclic muscle pain might pose with diagnosis. For example, the medial pterygoid muscle is injured by an inferior alveolar nerve block. This trauma causes local muscle soreness. The pain associated with the soreness in turn produces protective co-contraction. Since protective co-contraction can lead to muscle soreness, a cycle begins. During this cycling, the original tissue damage produced by the injections resolves. When tissue repair is complete, the original source of pain is eliminated; however, the patient may continue to suffer with a cyclic muscle pain disorder. Since the original cause of the pain is no longer part of the clinical picture, the clinician can easily be confused during the examination. The clinician needs to recognize that even though the original cause has resolved, a cyclic muscle pain condition exists and needs to be treated. This condition is an extremely common clinical finding and if not recognized often leads to mismanagement of the patient.
Local muscle soreness presents clinically with muscles that are tender to palpation and reveal increased pain with function. Structural dysfunction is common, and when the elevator muscles are involved, limited mouth opening results. Unlike protective co-contraction, the patient has great difficulty opening any wider. With local muscle soreness, there is actual muscle weakness.45,46,47 Muscle strength returns to normal when the muscle soreness is resolved. 46,47,48
CNS Effects on Muscle Pain
The muscle pain conditions described to this point are relatively simple, with their origins predominantly in the local muscle tissues. Unfortunately, muscle pain can become much more complex. In many instances, activity within the CNS can either influence or actually be the origin of the muscle pain. This may occur secondary to ongoing deep pain input or altered sensory input, or it may arise from central influences, such as up-regulation of the autonomic nervous system (eg, emotional stress). This occurs when conditions within the CNS excite peripheral sensory neurons (primary afferents), creating the antidromic release of algogenic substances into the peripheral tissues and resulting in muscle pain (ie, neurogenic inflammation) (chapter 4).10,49,50,51 These central excitatory effects can also lead to motor effects (primary efferents), resulting in an increase in muscle tonicity (co-contraction).7,8
Therapeutically, it is important that the clinician appreciate that the muscle pain now has a central origin. The CNS responds in this manner secondary to: (1) the presence of ongoing deep pain input, (2) increased levels of emotional stress (ie, an up-regulation of the autonomic nervous system), or (3) changes in the descending inhibitory system that lead to a decrease in the ability to counter the afferent input, whether nociceptive or not.
Myospasm (tonic contraction myalgia)
Myospasm is a CNS-induced tonic muscle contraction. For many years the dental profession felt that myospasms were the most common source of myogenous pain. More recent studies, however, shed new light on muscle pain and myospasms.
It is reasonable to expect that a muscle in spasm or tonic contraction would reveal a relatively high level of electromyographic activity. Studies, however, do not support the assumption that painful muscles have a significant increase in their EMG output. 4,7,8,19,35 These studies have forced us to rethink the classification of muscle pain and differentiate myospasms from other muscle pain disorders. Although myospasms of the muscles of mastication do occur, this condition is not common; when present it is usually easily identified by clinical characteristics.
The etiology of myospasms has not been well documented. Several factors are likely to combine to promote myospasms. Local muscle conditions certainly seem to foster myospasms. These conditions involve muscle fatigue and changes in local electrolyte balances. Deep pain input may also precipitate myospasms.
Myospasms are easily recognized by the structural dysfunction that is produced. Since a muscle in spasm is contracted, major jaw positional changes result according to the muscle or muscles in spasm. These changes in the position of the jaw create what is known as an acute malocclusion . An acute malocclusion is a sudden change in the occlusal condition as a result of a disorder. Since the malocclusion is secondary to a disorder, the clinician should not focus treatment on correcting the malocclusion, but instead on the disorder that has caused the malocclusion. Myospasms are also characterized by very firm muscles, as noted by palpation.
When the inferior lateral pterygoid muscle shortens due to myospastic activity, acute malocclusion results. This is recognized as disclusion of the ipsilateral posterior teeth and premature occlusion of the contralateral anterior teeth. The presence of pain sites within the muscle is identified by functional manipulation: pain is accentuated by maximum intercuspation (stretching the muscle) and by protrusion against resistance (contracting the muscle). It should be noted that pain with clenching of the teeth is relieved by biting ipsilaterally on a tongue blade, because this prevents intercuspation of the teeth and stretches the muscle. Unless acute malocclusion can be identified and pain induced by functional manipulation, a diagnosis of spasm of this muscle is invalid.
Local analgesic blocking of the inferior lateral pterygoid muscle promptly arrests all pain emanating from this source and offers the best clinical means of accurately locating the source of pain.
Regional myalgic disorders
Myofascial pain (trigger point myalgia)
Myofascial pain is a regional myogenous pain condition characterized by local areas of firm, hypersensitive bands of muscle tissue known as trigger points. This condition is sometimes referred to as myofascial trigger point pain. It is a type of muscle disorder that is not widely appreciated or completely understood, yet it commonly occurs in patients with myalgic complaints. In one study,52 more than 50% of the patients reporting to a university pain center were diagnosed as having this type of pain.
Myofascial pain was first described by Travell and Rinzler53 in 1952, yet the dental and medical communities have been slow to appreciate its significance. In 1969, Laskin 54 described the myofascial pain dysfunction (MPD) syndrome as having certain clinical characteristics. Although he borrowed the term myofascial, he was not describing myofascial trigger point pain. Instead MPD syndrome has been used in dentistry as a general term to denote any muscle disorder (not an intracapsular disorder). Since the term is so broad and general, it is not useful in the specific diagnosis and management of masticatory muscle disorders. MPD syndrome should not be confused with Travell and Rinzler’s description, which will be used in this textbook. It is this author’s suggestion that if a general term is need to describe muscle pain, the term masticatory muscle pain should be used as a generic term for all types of masticatory muscle pain and myofascial pain, unless the condition meets the original description in the medical literature, which will be discussed below.
Myofascial pain arises from hypersensitive areas in muscles called trigger points. These very localized areas in muscle tissues and/or their tendinous attachments are often felt as taut bands when palpated, which elicits pain. The exact nature of a trigger point is not known. It has been suggested 1,55 that certain nerve endings in the muscle tissues may become sensitized by algogenic substances that create a localized zone of hypersensitivity.56 There may be a local temperature rise at the site of the trigger point, suggesting an increase in metabolic demand and/or reduction of blood flow to these tissues.57 A trigger point is a very circumscribed region in which relatively few motor units seem to be contracting. 58,59 If all the motor units of a muscle contract, the muscle will of course shorten in length. This condition is called myospasm and has already been discussed in this chapter. Since a trigger point has only a select group of motor units contracting, no overall shortening of the muscle results, as occurs with myospasm.
The unique characteristic of trigger points is that they are a source of constant deep pain and therefore can produce central excitatory effects (see chapter 4). If a trigger point centrally excites a group of converging afferent interneurons, referred pain will often result, generally in a predictable pattern according to the location of the involved trigger point. The pain is often reported by the patient as headache pain.
The etiology of myofascial pain is complex. Unfortunately, we lack a complete understanding of this myogenous pain condition. It is therefore difficult to be specific concerning all etiologic factors. Travell and Simons have described certain local and systemic factors that seem to be associated, such as trauma, hypovitamintosis, poor physical conditioning, fatigue, and viral infections. 60 Other important factors are likely to be emotional stress and deep pain input.
The most common clinical feature of myofascial pain is the presence of trigger points. Although palpation of trigger points produces pain, local muscle sensitivity is not the most common complaint of patients suffering from myofascial trigger point pain. The most common symptom is usually associated with the central excitatory effects created by the trigger points. In many instances, patients may be aware only of the referred pain and not even acknowledge the trigger points. A perfect example is the patient suffering from myofascial trigger point pain in the trapezius muscle that creates referred pain to the temple region (see Fig 12-9).61,62 The chief complaint is temporal headache, with very little acknowledgment of the trigger point in the shoulder. This clinical presentation can easily distract the clinician from the source of the problem. The patient will draw the clinician’s attention to the site of the pain (the temporal headache) and not the source. The clinician must always remember that for treatment to be effective it must be directed toward the source of the pain, not the site. Therefore, a clinician must always search for the true source of the pain.
Since trigger points can create central excitatory effects,63,64,65 it is also important to be aware of all the possible clinical manifestations. As stated in chapter 4, central excitatory effects can appear as referred pain, secondary hyperalgesia, protective co-contraction, or even autonomic responses. These conditions must be considered when evaluating the patient.
An interesting clinical feature of a trigger point is that it may present in either an active or a latent state. In the active state, it produces central excitatory effects. Therefore, when a trigger point is active, a headache is commonly felt. Since referred pain is wholly dependent on its original source, palpation of an active trigger point (local provocation) often increases such pain. Although not always present, when this characteristic appears it is an extremely helpful diagnostic aid. In the latent state, a trigger point is no longer sensitive to palpation and therefore does not produce referred pain. When trigger points are latent, they cannot be found by palpation and the patient does not complain of headache pain. In this case the history is the only data that leads the clinician to make the diagnosis of myofascial pain. In some instances the clinician should consider asking the patient to return to the office when the headache is present so that confirmation of the pattern of pain referral can be verified and the diagnosis confirmed.
It is thought that trigger points do not resolve without treatment. They may in fact become latent or dormant, creating a temporary relief of the referred pain. Trigger points may be activated by various factors, 66 such as increased use of a muscle, strain on the muscle, emotional stress, or even an upper respiratory infection. When trigger points are activated, the headache returns. This is a common finding with patients who complain of regular late afternoon headaches following a very trying and stressful day.
Along with referred pain, other central excitatory effects may be felt. When secondary hyperalgesia is present, it is commonly felt as an increased sensitivity to touching of the scalp. Some patients will even report that their “hair hurts” or that it is painful to brush their hair. Co-contraction is another common condition associated with myofascial pain. Trigger points in the shoulder or cervical muscles can produce co-contraction in the muscles of mastication. 7 If this continues, local muscle soreness in the masticatory muscles can develop. Treatment of the masticatory muscles will not resolve the condition, because its source is the trigger points of the cervicospinal and shoulder muscles. However, treatment of the trigger points in the shoulder muscles will resolve the masticatory muscle disorder. Management may become difficult when muscle soreness has been present for a long time, because it can initiate cyclic muscle pain. In these cases, extending treatment to both the muscles of mastication and the trigger points in the cervicospinal and shoulder muscles will usually resolve the problem.
On occasion, autonomic effects are produced by deep pain input from trigger points. These may result in such clinical findings as tearing or drying of the eyes, or vascular changes (eg, blanching and/or reddening of tissue) may occur. Sometimes the conjunctivae will become red. There may even be mucosal changes that produce nasal discharge similar to an allergic response. The key to determining whether the autonomic effects are related to central excitatory effects or to a local reaction such as allergies is the unilateral appearance. Central excitatory effects in the trigeminal area rarely cross the midline. Therefore, if the deep pain is unilateral, the autonomic effects will be on the same side as the pain. In other words, one eye will be red and the other normal, one nostril draining mucus and the other not. With allergic responses, both eyes or both nostrils will be involved.
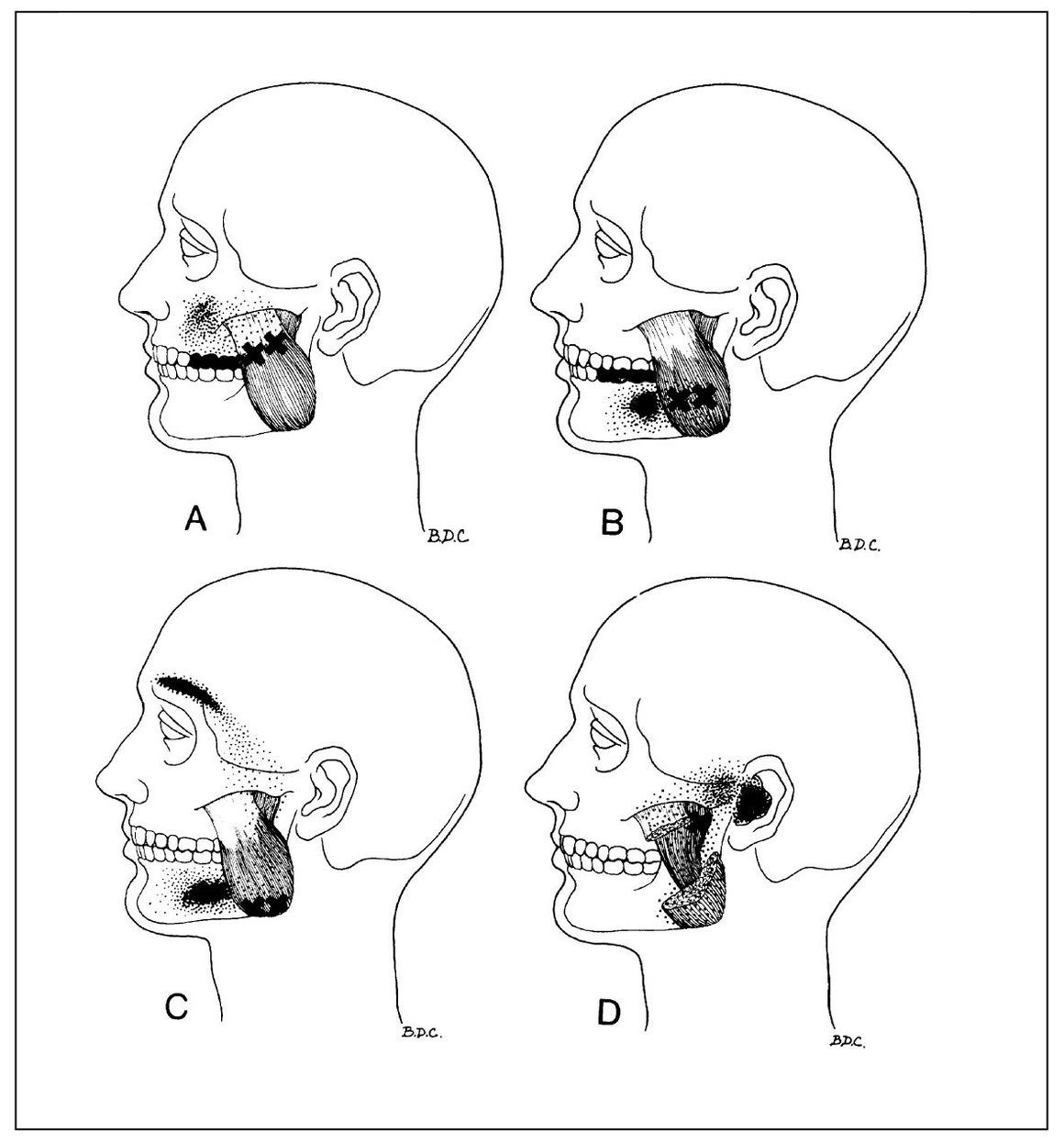
Fig 12-3 Trigger points (x) located in various parts of the masseter muscle. Solid black shows essential reference pain zones; stippled areas are spillover pain zones. A = Superficial layer, upper portion; B = superficial layer, midbelly; C = superficial layer, lower portion; D = deep layer, upper part. (From Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. Baltimore: Williams & Wilkins, 1983:220. Used with permission.)
By way of summary, the clinical symptoms reported with myofascial pain are most commonly associated with the central excitatory effects created by the trigger points and not the trigger points themselves. The clinician must be aware of this and find the involved trigger points. When these are palpated, they appear as hypersensitive areas often felt as taut bands within the muscle. There is usually no local pain when the muscle is at rest but some when the muscle is used. Often slight structural dysfunction will be seen in the muscle harboring the trigger points. This is commonly reported as a “stiff neck.”
Referral patterns of myofascial pain in the orofacial region.
The clinician treating orofacial pain disorders needs to have a sound understanding of myofascial pain since it is so common in pain populations. The following section will review the most common muscles of the head and neck and the typical referral pattern for each. Familiarity with these patterns can be extremely helpful during history taking, examination, and diagnosis.
Masseter muscle. Trigger points located at sites in the superficial layer of the masseter muscle refer to the posterior mandibular and maxillary teeth, the jaw, and the face (Fig 12-3). Toothache is a common complaint from this source. The deep portion refers to the ear and TMJ area. Earache and preauricular pain thought to be emanating from the joint are common complaints. Moderate restriction of opening associated with ipsilateral deflection of the midline incisal path may be observed. Tinnitus described as a “low roaring noise” may occur from deep masseter trigger points. The muscle is accessible for manual palpation to identify trigger sites.
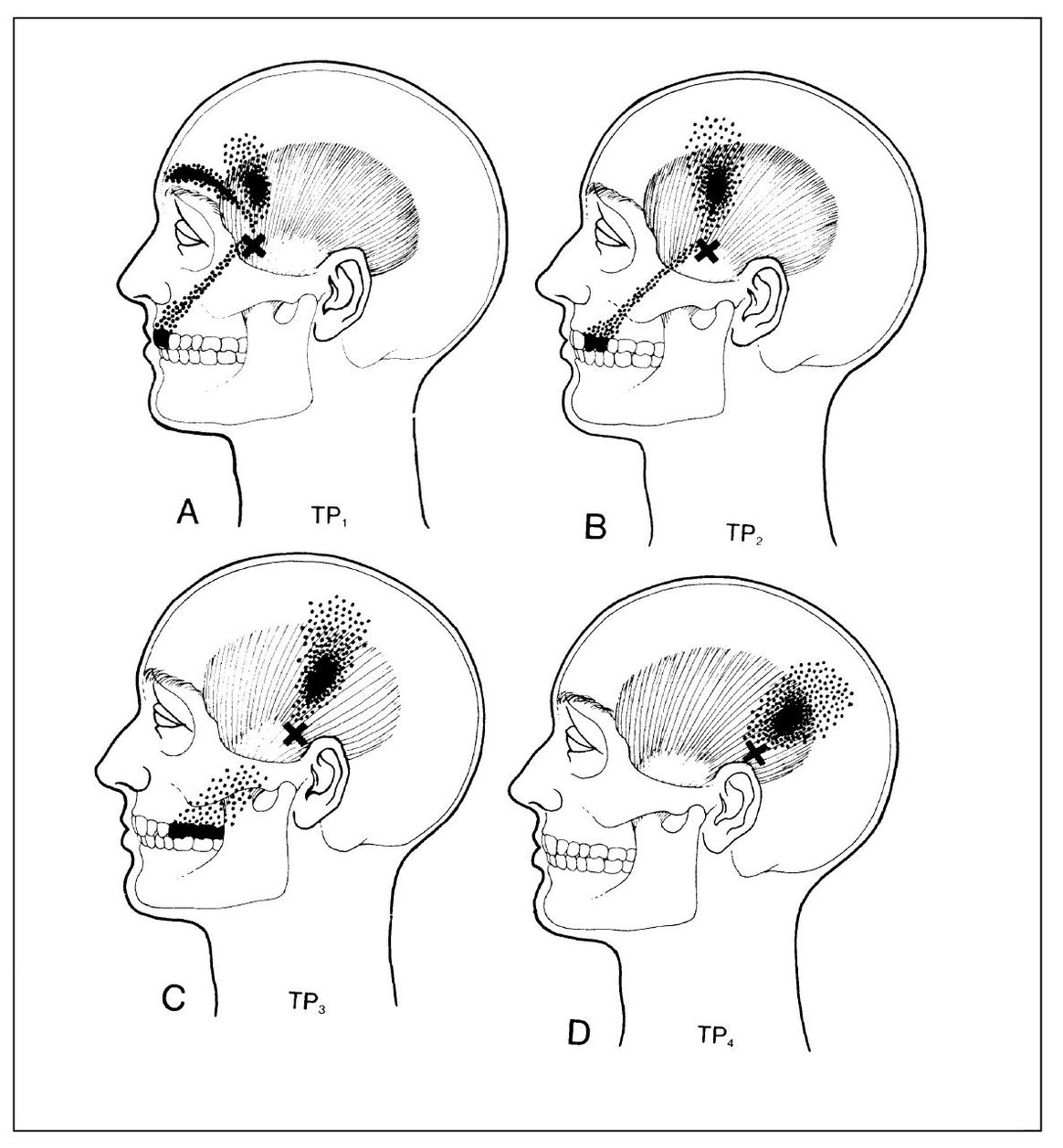
Fig 12-4 Referred pain patterns from trigger points (x) in the temporalis muscle. A = Anterior fibers; B and C = middle fibers; D = posterior fibers. (From Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. Baltimore: Williams & Wilkins, 1983:237. Used with permission.)
Temporalis muscle. The reference zone of the temporalis muscle includes all the maxillary teeth and upper portion of the face (Fig 12-4). Headache and toothache (see chapter 11) are the common complaints. A restricted opening is rarely displayed. The muscle is accessible for manual palpation to identify trigger sites.
Medial pterygoid muscle. The reference zone for the medial pterygoid muscle includes the posterior part of the mouth and throat, as well as the temporomandibular and infra-auricular areas (Fig 12-5). Throat and postmandibular (infra-auricular) pain is the common complaint. Eustachian tube symptoms may be displayed. Moderate restriction of the mouth opening associated with contralateral deflection of the midline incisal path may be observed. The muscle is only partially accessible for intraoral manual palpation to identify trigger sites. Functional manipulation therefore may be needed for this purpose: A pain source within the muscle will be accentuated by opening widely (stretching the muscle) and by biting firmly (contracting the muscle).
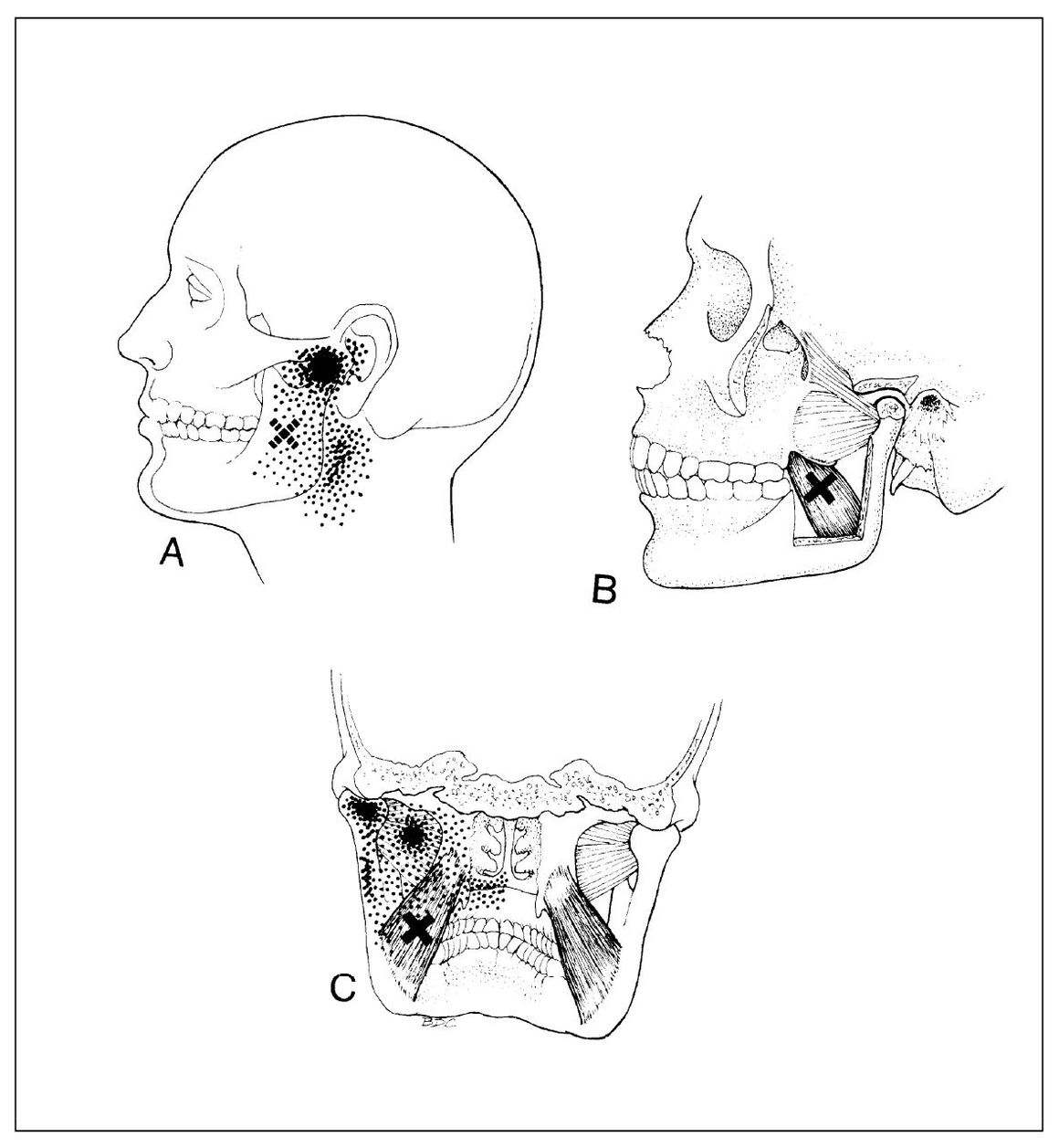
Fig 12-5 Referred pain pattern and location of responsible trigger point (x) in the medial pterygoid muscle. A = External areas of pain to which the patient can point; B = anatomic cutaway to show the location of the trigger point; C = coronal section showing internal areas of pain. (From Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. Baltimore: Williams & Wilkins, 1983:250. Used with permission.)
Inferior lateral pterygoid muscle. The lateral pterygoid muscle has been incriminated as the cause of numerous temporomandibular complaints. This probably stems from a lack of understanding of how the muscle is constructed and what its normal functions are. No doubt, the difficulty of adequately examining the muscle clinically has provided good cover for these incriminations. Several hard facts need to be considered in evaluating the effects of this muscle on masticatory symptoms. It should be understood first that there are two lateral pterygoid muscles: the inferior lateral pterygoid and the superior lateral pterygoid. Only the inferior lateral pterygoid muscle protracts the mandible, and therefore it can act to create acute occlusal disharmony when it is shortened. The superior muscle remains inactive at all times except during power strokes in conjunction with elevator muscle action.67,68 Even when shortened, the superior lateral pterygoid muscle cannot disrupt joint functioning in the absence of structural joint disease.
The dearth of muscle spindles in the lateral pterygoid muscles reduces the chance of reflex contraction when this muscle is stretched. Then too, this muscle is composed chiefly of slow-twitch fibers69 that resist fatigue and seldom undergo spastic activity. The prime reason that a diagnosis of this muscle is so difficult is because it is inaccessible for manual palpation.70 Despite voluminous testimony to the contrary, the possibility of diagnostically accurate manual or instrument palpation of the muscle is remote.71
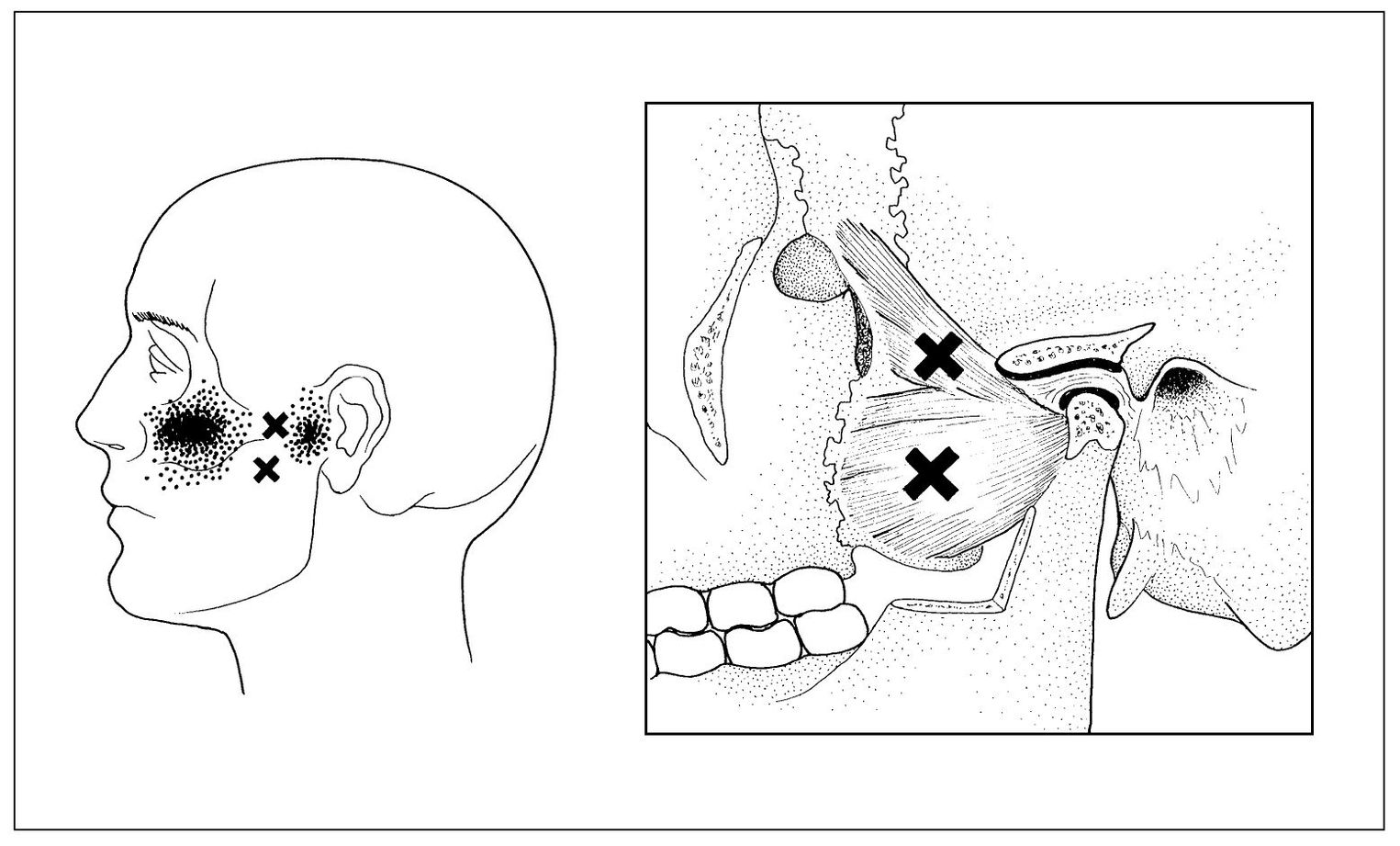
Fig 12-6 Referred pain patterns of trigger points (x) in the superior and inferior lateral pterygoid muscles. (From Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. Baltimore: Williams & Wilkins, 1983:261. Used with permission.)
Trigger points in the inferior lateral pterygoid muscle refer to the TMJ area (Fig 12-6). Slight acute malocclusion may be sensed as disclusion of the ipsilateral posterior teeth and premature occlusion of the contralateral anterior teeth (Cases 3 and 4). Since this muscle is inaccessible for palpation, functional manipulation is required to help identify the presence of myofascial pain: A pain source within the muscle will be accentuated by maximum intercuspation (stretching the muscle) and by protruding the jaw against resistance (contracting the muscle).71
Superior lateral pterygoid muscle. Trigger points in the superior lateral pterygoid muscle refer to the zygomatic area (Fig 12-6). No dysfunction is observed unless there is extensive deterioration in the TMJ that is sufficient to permit anterior displacement of the articular disc. Diffuse pain in the malar area is the usual complaint. Since this muscle is inaccessible for manual palpation, 70 functional manipulation is required to identify the presence of myofascial pain: A pain source within the muscle will be accentuated by maximum intercuspation (stretching the muscle) and by biting on a separator (contracting the muscle). Opening widely and protruding against resistance do not involve this muscle functionally and therefore are painless.
Case 3 Cycling masticatory muscle pain secondary to chronic ear pain
Chief Complaint Diffuse left side facial pain.
History
A 47-year-old woman presented with mild, continuous, protracted, variable but steady, dull, aching pain diffusely located in the right ear, preauricular area, face, and temple, aggravated by opening widely, chewing food, and clenching the teeth. The pain was also accompanied by acute malocclusion and restricted opening.
The patient had had recurring episodes of earache associated with acute upper respiratory infections for several years. About 3 weeks earlier, she had such an episode with continuous severe earache on the right side. After about 7 days, she noticed her “bite was off,” she could not open normally, and she had pain with opening, chewing, and occluding the teeth. This had become progressively worse, even though antibiotic therapy by her ear, nose, and throat (ENT) physician eliminated the ear infection completely. He referred her to her dentist, who recognized the protective co-contraction and occlusal disharmony but declined to adjust the occlusion pending further investigation of the />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


