12 Orofacial Pain Conditions
12.0 INTRODUCTION
Pain is a subjective symptom defined by the International Association for the Study of Pain (IASP) as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.” The diagnostic process to investigate a pain complaint may be straightforward, such as a toothache with clinically obvious caries and an acute pulpitis, or complex, which may involve physical, psychological, and social factors that can combine to create unique pain experiences. Orofacial pain is a presenting symptom of a broad spectrum of conditions affecting the orofacial complex (Table 12.1). There are numerous etiologies for pain symptoms, and, as with all pain conditions, the pain presentation can vary significantly. Some conditions are easily recognized and treated, while others are challenging to localize, and diagnosis and management may be difficult.
Orofacial pain complaints may involve teeth and their supporting structures or may be due to non-odontogenic causes. When assessing orofacial pain, the dental practitioner must first rule-out odontogenic etiology. Common odontogenic conditions such as dental caries and acute periodontal disease should be considered, as well as dentin hypersensitivity and cracked tooth syndrome. Further, inflammatory and/or infectious orofacial conditions often present with pain and may affect extraoral and/or intraoral hard and soft tissues. For example, lichen planus may be accompanied by tissue inflammation and ulceration, with common presenting symptoms being mucosal tissue pain or sensitivity. Another condition, osteomyelitis, is an acute or chronic bone infection that can occur in patients secondary to mandible fractures, odontogenic or soft tissue infection, or as a complication of a local or regional surgical procedure. Symptoms include deep pain and tenderness, swelling, erythema, and, in acute cases, fever. In general, extraoral and/or intraoral hard and soft tissue pathology typically presents with tissue changes or damage that corresponds to the pain complaint.
Other orofacial pain conditions are more complex, as they may represent pain referred to orofacial structures, pain that mimics toothache symptoms, or pain originating in orofacial structures that are not easy to visualize, such as muscular, vascular, and neural structures. These pain conditions will be addressed in this chapter. Diagnosis and management of orofacial pain conditions can be challenging since the differential diagnosis is complex, multifactorial etiologic factors may contribute to the pain experience, and achievement of pain relief may be difficult. Complex orofacial pain conditions often require referral to pain specialists, and a timely and appropriate referral can minimize unnecessary dental procedures as well as improve quality of life and associated morbidity. An understanding of pain perception and pathways is necessary for the clinician to recognize these disorders when they present in the orofacial region.
Table 12.1 Categories of non-odontogenic orofacial pain conditions.
| System | Diagnosis | Signs and symptoms |
| Musculoskeletal | Temporomandibular disorders | Facial pain TMJ pain Pain in muscles of mastication |
| Headache (muscular origin) | Bilateral pain in temporalis and/or pericranial muscles | |
| Vascular | Giant cell arteritis (temporal arteritis, cranial arteritis) | Severe headache Tenderness in temporal region Visual disturbance Jaw claudication |
| Migraine headache | Unilateral, severe facial pain May be associated with aura |
|
| Trigeminal autonomic cephalgias (TACs) | Cluster headache unilateral, severe pain, rapid onset duration up to 3 hours assocated with periods of oxygen desaturation (e.g., sleep) autonomic changes: facial flushing, rhinorrhea, lacrimation, salivation, facial edema Chronic paroxysmal hemicrania unilateral, severe pain, rapid onset duration up to 45 minutes, multiple episodes per day may occur autonomic changes: sinus stuffiness, rhinorrhea, lacrimation, edema aborted with indomethacin Short-lasting unilateral neuralgiform headache with conjunctival injection and tearing/cranial autonomic features (SUNCT/SUNA) unilateral, severe pain, rapid onset duration a few seconds, high frequency of episodes orbital, supraorbital, temporal and frontal location autonomic changes: conjunctival injection and tearing |
|
| Neurologic | Trigeminal neuralgia | Severe, episodic, unilateral pain in nerve distribution |
| Post-herpetic neuralgia | History of herpes zoster Constant pain in nerve distribution corresponding to dermatome of herpes zoster presentation |
|
| Chronic trigeminal neuropathy (post-traumatic neuropathic pain, atypical odontalgia) | Persistent pain, varies in intensity No odontogenic pathology |
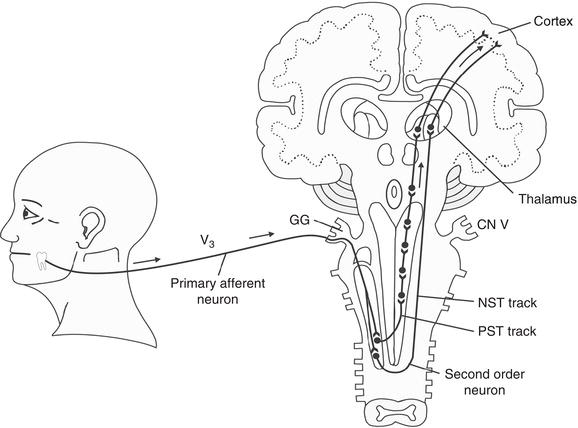
Figure 12.1 Afferent pain pathway. The impulse follows the primary afferent neuron of V3 through the gasserian ganglion (GG) into the subnucleus caudalis region of the trigeminal spinal tract, where it synapses with a second-order neuron and travels through the neospinothalamic tract (NST Tract) or paleospinothalamic tract (PST Tract) to the thalamus and cortex.
Reproduced with permission from Okeson JP. Bell’s Orofacial Pains, 5th ed., Figure 3.2, page 54, Quintessence Publishing Co. Inc., Chicago.
12.1 Pain mechanisms
Pain is initiated through noxious stimulation of primary afferent neurons at the site of injury, and the signal is carried centrally through complex neurochemical processes (Figure 12.1). Orofacial pain is generated by sensory innervation supplied predominantly by the trigeminal nerve, though the facial (CNVII), glossopharyngeal (CNIX), vagus (CNX), and/or branches of the higher cervical nerves may also be involved. In the trigeminal nerve (CNV), most primary afferents converge in the trigeminal sensory ganglion, communicate with second-order neurons in the spinal nucleus of CNV, and transmit nociceptive input centrally to the thalamus and then the primary somatosensory cortex. Several primary afferents can converge to signal a single second-order neuron in the brain stem complex, resulting in pain referral and difficulties in pain localization. The autonomic nervous system also responds to painful stimulus through sympathetic and parasympathetic innervation, causing increased heart rate and other physiologic activities, including control over sweat glands, salivary flow, and pupil activity.
12.2 General classification of pain
Orofacial pain can be broadly classified as being either nociceptive or neuropathic. Nociceptive, or inflammatory, pain is transmitted by normal physiologic pathways in response to potentially tissue-damaging stimuli and typically ends when the underlying tissue injury resolves. Pain may also be classified as neuropathic, in which pain is initiated or caused by a primary lesion, disease, or dysfunction in the nervous system, and nociceptor stimulation is not necessary (Table 12.2). While tissue and nerve injury may initiate processes that lead to pain, neuropathic pain persists once the initial injury heals due to damage and/or dysfunction in the pain-generating pathways. These alterations in pain processing at the peripheral and central levels produce characteristic symptoms such as hyperalgesia (an increased response to a stimulus that is normally painful), allodynia (pain due to a stimulus that does not normally provoke pain), dysesthesia (an unpleasant and abnormal sensation, whether spontaneous or evoked), and paresthesia (an abnormal sensation, whether spontaneous or evoked). Neuropathic pain can be an extremely debilitating form of pain that occurs when peripheral, autonomic, and/or central nerves are affected.
Table 12.2 Characteristics of neuropathic pain.
| Signs and Symptoms | Persistent pain caused by a lesion (including trauma) or disease of the somatosensory nervous system |
| Diagnostic investigations reveal a sensory abnormality of affected nerve(s) and/or clinical history reveals trauma or disease that justifies diagnosis | |
| Clinical absence of pathology that may cause pain symptoms | |
| May affect central, peripheral, and/or autonomic nerves | |
| Characteristics | Hyperalgesia: Increased response to a stimulus that is normally painful |
| Allodynia: Pain due to a stimulus that does not normally provoke pain | |
| Paresthesia: Abnormal sensory sensation | |
| Dysesthesia: Abnormal and unpleasant sensation, whether spontaneous or evoked | |
| Temporal Pattern | Episodic: Intense pain that varies in frequency and duration, associated with pain-free episodes |
| Continuous: Constant pain that presents with varying intensities |
12.3 Pain assessment
Assessment of a pain patient involves numerous steps that begin with obtaining a pain history, followed by clinical assessment of the pain condition to include physical and functional assessment as well as possible imaging and laboratory studies. Finally, the behavioral contributions to the pain condition must be considered in all patients.
12.3.1 Pain history
Assessment of the patient with an orofacial pain complaint begins with a pain history and description of pain characteristics. This portion of the evaluation is critical in determining etiologic factors, orofacial structures that may be involved, and, ultimately, a definitive pain diagnosis. The pain history should involve a patient’s description (self-report) of the intensity, persistence (continuous vs. episodic), and duration of overall pain, as well as duration of pain episodes and functional impact upon daily activities such as eating and sleeping. Pain intensity should be reported as “current,” “worst,” and “average” pain using a pain scale. For example, a categorical scale may classify the pain as none/mild/moderate/severe, or a numerical 0 to 10 scale may be utilized, with “0” representing no pain and “10” representing the worst pain one can imagine (Figure 12.2). The patient should also use adjectives to describe his/her pain experience, such as “dull and achy” or “sharp and electrifying.” Activities and/or treatments that increase the pain as well as those that decrease the pain experience, and to what degree the changes in pain occur, should be ascertained. Orofacial pain conditions that have been present for less than 3 months are generally categorized as acute conditions, while those that have persisted for at least 3 months are considered chronic pain conditions.
Figure 12.2 Numeric rating scale.
Potential etiologic factors contributing to the pain presentation should be elicited from the history, including recent dental procedures or a history of direct trauma to orofacial structures. The history should also recognize systemic conditions that may affect orofacial structures (e.g., arthritis conditions may affect the temporomandibular joints [TMJs]) and pain conditions that may present in orofacial structures (e.g., migraine headache). Parafunctional activities and recent stressful events should also be identified in the orofacial pain work-up.
12.3.2 Clinical pain assessment
The physical assessment involves thorough evaluation of the orofacial structures associated with the pain complaint and should begin with a patient pointing to the area(s) where s/he is experiencing the greatest source of pain. Extraorally, basic tests of balance and proprioception (standing without swaying, touching hand to nose) as well as sensory and motor function of cranial nerves should be assessed. Sensory evaluation involves determining if symptoms of hyperalgesia, allodynia, paresthesia, and/or anesthesia are present and should be performed when the pain history indicates altered sensory function, particularly along the three trigeminal nerve branches. For example, brushing a cotton-tipped applicator lightly along the CNV distribution may result in a sensation of light touch (normal), increased itchy or pain sensation (allodynia), decreased sensation (paresthesia), or no sensation (anesthesia). To assess for hyperalgesia, utilizing a “sharp” pointed instrument (e.g., the wooden end of a cotton-tipped applicator) along the nerve distribution may result in an increased pain response. Altered sensory function extending beyond the trigeminal nerve should be recorded during the examination and may warrant referral to a neurologist for further evaluation.
Next, the TMJs and surrounding structures should be assessed. During evaluation, the patient should report the pain presence and intensity using a ranking (e.g., none/mild/moderate/severe) or scale (e.g., 0-10 scale). The patient is instructed to open his/her mouth as wide as possible without pain, and the interincisal distance, known as the range of mandibular movement (ROM), is recorded (e.g., using a ruler or other measurement device). The patient is asked to close and then open as wide as possible even if there is pain and point to the area(s) that are most painful. A second measurement, the ROM with pain, is recorded. If the opening appears to be limited (less than 40 millimeters), the clinician should use the thumb and index finger to gently assist the patient to open farther. This is the passive stretching value and is helpful in distinguishing between limitations of ROM due to disc displacement without reduction (unable to assist the patient to open further; section 12.4.1) or other rare pathology (such as neoplasm) and muscular dysfunction (ability to increase ROM at least 5 millimeters with passive assistance). The open/close pattern of the mandible is recorded (straight, corrected deviation [S curve], uncorrected deviation). Next, the lateral poles of the TMJs, located anterior to the external meatus, are palpated for the presence of pain, indicating joint inflammation, and then opening and closing movements are performed to assess for the presence and timing (e.g., early or late in the masticatory cycle) of TMJ sounds (clicking, popping, and/or crepitus), pain, and palpable differences in joint form. Lateral and protrusive excursions are measured, and pain and/or joint sounds that occur during these movements should be recorded. Normal lateral and protrusive movements are at least 7 millimeters. Lastly, the bilateral extraoral muscles of mastication (temporalis, masseter) and cervical muscles (sternocleidomastoid, platysma, occipital, trapezius) are palpated using firm pressure and the patient is asked to report upon the presence and intensity of pain at each site of muscle palpation and whether or not palpation produces pain beyond the site being evaluated (pain referral).
Intraoral examination begins with palpation of bilateral intraoral muscles of mastication (masseter, lateral pterygoid) and recording the presence and intensity of pain. Changes in occlusion manifesting as a unilateral or bilateral open bite should be recorded, as they may indicate joint remodeling or destruction and can be slowly progressive or rapid in development. If indicated by the history of the pain complaint, evaluation of odontogenic structures may include palpation, percussion, thermal sensitivity testing, periodontal probing, and/or factors related to occlusion. Finally, if sensory alterations of the intraoral CNV maxillary and/or mandibular nerve branches are suspected from the pain history, evaluation of hyperalgesia, allodynia, paresthesia, and/or anesthesia should be performed.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


