2 Basic Tests and Evaluation Methods of Systemic Health
2.0 INTRODUCTION
Physical health indicators can provide useful information about the systemic health of patients. Some of the most basic physical assessment measures are vital signs, which should be performed routinely in the dental setting. Testing vitals can corroborate findings from the health history or identify conditions that may need to be further evaluated by medical professionals. For example, taking the blood pressure and pulse at the beginning of a dental appointment can identify patients at risk for hypertension who may need to be referred to a physician for further assessment and management. Other testing measures involve blood sampling, which may be indicated in the dental setting in certain circumstances, such as evaluating the risk for bleeding prior to a surgical procedure. Assessment of a blood glucose level in a diabetic patient may prompt modifications in the planned dental appointment to prevent a hypoglycemic episode. Since dental patients are typically seen at routine intervals, oral health care providers can play an active role in monitoring physical health measures of their patients and can encourage follow-up with medical personnel when indicated.
Basic blood measurements are useful screening tools for systemic disease. These tests involve assessment of cells, chemistry values, and electrolytes in blood and can provide information pertaining to diagnosis and monitoring of disease. Tests of red and white blood cells may be indicators of anemias and the body’s ability to fight infection. Serum chemistry and electrolyte analytes provide insight regarding kidney and liver function, acid-base and fluid balance, nutritional and endocrine status, and pH homeostasis. Test results can alert the oral health care practitioner regarding potential for bleeding, infection, and systemic function, so it is important to become familiar with these clinical investigations. This chapter will introduce basic health indicators that serve as proxy measures of systemic function and will guide the oral health care provider in ordering and interpreting the results as they relate to physiologic function.
2.1 Vital signs
Vital signs include respiratory rate, temperature, pulse, blood pressure, and height and weight are recorded as part of a routine physical examination. Vital signs can serve as screening tools for systemic disease and provide baseline measures of body function. It is good practice to take vital signs at new patient visits and record pulse and blood pressure at recall appointments. Assessment of the respiratory rate is usually not necessary in the dental setting unless cardiopulmonary disease is suspected or sedation is planned. The respiratory rate is determined by counting the number of times the chest rises and falls for 30 seconds. A normal rate is 12–15 respirations per minute. Measurement of a patient’s temperature may be warranted when an infection is suspected. Normal body temperature is 98.6ºF (37ºC), and an elevated temperature indicates a systemic illness or infection.
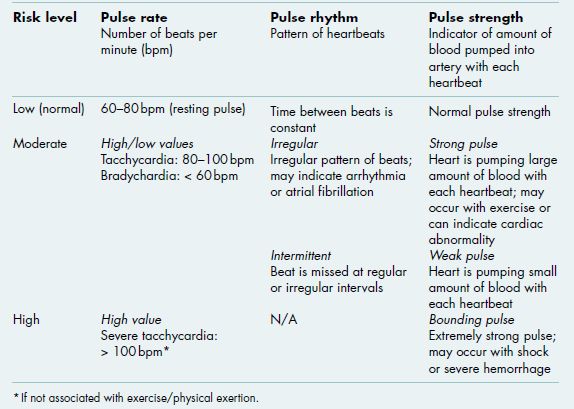
Radial or carotid artery pulse is a measure of cardiac rate, rhythm, and strength. Carotid pulse is obtained using the first two fingers in the region of the carotid bulb, just below the angle of the mandible and anterior to the sternocleidomastoid muscle. Alternatively, radial pulse can be determined by placing the fingers between the radius and flexor tendons on the ventral wrist. The pulse rate is determined by counting the number of beats for 15 seconds. Normal heart rate is 60–80 beats per minute (bpm). A high pulse (greater than 100 bpm) is tachycardia and may be an indicator of a cardiac condition, while a low pulse (less than 60 bpm) is bradycardia (Alert Box 2.1). The pulse rhythm refers to the pattern of the beats. In a regular pulse rhythm, the time between beats is constant, while an irregular rhythm does not have an even pattern and can signify an abnormal cardiac condition, such as an arrhythmia or atrial fibrillation. An intermittent pulse is an irregular rhythm in which the beat is missed at regular or irregular intervals. Finally, the pulse strength (force) is an indicator of the amount of blood forced into the artery by the heartbeat. A normal pulse has normal strength. A very strong or bounding pulse occurs when the heart is pumping a large amount of blood with each heartbeat. This can occur normally with heavy exercise, high anxiety, or alcohol consumption, or it could be a sign of a cardiac abnormality. A strong pulse is stronger than a normal pulse, but is less than bounding and may occur with shock or severe hemorrhage. A weak pulse is hard to detect and indicates that the heart is pumping only a small amount of blood with each heartbeat.
Table 2.1 Classification of hypertension.*,†
| Category | Systolic blood pressure (mm Hg) | Diastolic blood pressure (mm Hg) |
| Normal | < 120 | and < 80 |
| Pre-hypertension | 120–139 | or 80–89 |
| Hypertension Stage 1 | 140–159 | or 90–99 |
| Hypertension Stage 2 | ≥ 160 | or ≥ 100 |
| Isolated systolic hypertension | ≥ 140 | and < 90 |
* Medical management using antihypertensive drugs is recommended at or above hypertension Stage 1. In patients with chronic kidney disease or diabetes, medical management is recommended if blood pressure is ≥ 130/80 mm Hg.
† Adapted from National Heart, Lung and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. NIH Publication, December 2003.
Blood pressure assesses pressure within the arteries during cardiac contraction (systole) and cardiac pause (diastole). This is measured using a manual or electronic sphygmomanometer placed around the upper arm. The pressure generated by the cuff exceeds that within the arteries and is slowly released to detect the pulse as blood is again pumped through the vessels. The pressure at which the first evidence of a pulse is detected is the systolic, and the pressure at which a pulse can no longer be detected is the diastolic. The auscultatory gap is the interval of pressure where sounds indicating systolic pressure fade away and reappear at a lower pressure point during the manual measurement of blood pressure. Improper interpretation of this gap may lead to an underestimation of systolic blood pressure and/or an overestimation of diastolic readings. It is therefore recommended to palpate the radial artery and inflate the blood pressure cuff until the radial artery pulse disappears to obtain the true systolic pressure when manually recording a patient’s blood pressure.
Blood pressure values are a standard screening tool for hypertension, and the Seventh Report of the Joint National Committee (JNC7) has developed a simple classification system for blood pressure levels and categories of hypertension (Table 2.1). A systolic or diastolic blood pressure measurement higher than the accepted normal values (less than 120/80 mm Hg) is classified as pre-hypertension (120–139/80–89 mm Hg) or hypertension (140/90 mm Hg or greater). Isolated systolic hypertension refers to elevated systolic pressure with normal diastolic pressure and is common in older adults. Individuals with blood pressures 130/80 mm Hg or greater with concomitant diabetes mellitus or chronic kidney disease are classified as having hypertension. Patients on whom abnormal blood pressure readings are detected should be referred to a physician for further evaluation and management. Medical management with antihypertensive medication is recommended for all patients with hypertension (as specified in JNC7), and dental procedures should be delayed in patients with uncontrolled Stage 2 hypertension since these individuals are at increased risk for cardiac events, such as myocardial infarction and/or cerebrovascular accident.
Oxygen saturation is a percentage indicating the ratio between the actual oxygen content of hemoglobin (Hgb) and the potential maximum oxygen-carrying capacity of Hgb. It is determined using a pulse oximeter, a small, clip-like sensor that is placed on a digit over the fingernail. Normal levels range from 95% to 100%. Oxygen level below 86% requires emergency medical intervention (i.e., administer oxygen, send to urgent care facility or emergency room). Measuring oxygen saturation in the dental environment is mandatory when sedation is used to monitor breathing, and may be considered during surgical procedures, particularly in patients with medical conditions that can cause hypoxia (e.g., chronic obstructive pulmonary disorder, emphysema, congestive heart failure).
2.2 Diagnostic fluids
2.2.1 Blood
Blood is the most commonly used diagnostic fluid, particularly because it is obtained in a simple, relatively non-invasive manner and has tremendous potential for basic screening, diagnosis, and monitoring of disease. Blood is typically drawn through venipuncture, in which an adequate volume of venous blood can be obtained for most laboratory tests. Capillary puncture (skin puncture) may be performed when smaller quantities of blood are sufficient. Whole blood is composed of blood cells suspended in a liquid called blood plasma. Plasma is mostly water and also contains dissolved proteins, electrolytes (mainly sodium and chloride ions), blood-clotting factors, hormones, glucose, and carbon dioxide. The blood cells present in blood are white cells (leukocytes), red cells (erythrocytes), and platelets (thrombocytes). The term serum refers to plasma from which the clotting proteins have been removed. Most of the proteins remaining in serum are albumin and immunoglobulins (antibodies). Blood tests can screen for systemic disease and dysfunction (e.g., diabetes, kidney/liver dysfunction), certain blood disorders (e.g., anemia, leukemia), abnormal bleeding and clotting (e.g., hemophilia, thrombocytopenia), inflammation (e.g., autoimmune disorders) and infection (e.g., HIV).
2.2.2 Saliva as a diagnostic fluid
Point-of-care (POC) diagnostics refers to tests performed in the primary care setting to provide results rapidly and accelerate clinical decision making. Some advantages of using saliva for POC testing include non-invasive collection, possibility for self-collection, and the fact that salivary levels of many molecules reflect that in blood and urine, though in lower concentrations. Perhaps the most widespread use of these tests is the oral fluid-based test for antibodies to HIV. This test is safe and easy to use, though positive results should be confirmed with serum tests. Saliva can also be used to identify and monitor the presence of chemicals and molecules used in the health care setting such as drugs (illicit, over-the-counter, prescription), steroid hormones, and tobacco (see chapter 8).
Researchers are studying the potential of using saliva to diagnose oral and systemic conditions. The presence of antibodies in saliva may aid with the diagnosis of other infectious diseases such as hepatitis and bacterial infections, and proteins, hormones, and RNA transcripts in saliva may be associated with certain cancers, including oral, breast, and ovarian cancer. In addition, specific inflammatory mediators and enzymes in saliva may serve as biomarkers for the diagnosis of oral disease such as periodontitis and dental caries as well as systemic disease such as acute myocardial infarction. The field of salivary diagnostics is emerging research, and in the future saliva may contribute to POC diagnosis of numerous oral and systemic conditions as well as monitoring health and response to treatment.
Table 2.2 Complete blood count (CBC) tests.
| Test | Conventional abbreviation | Clinical significance of values |
| White blood cell count | WBC | Ability to fight infection; hematologic dysfunction or malignancy; presence of infection (leukocytosis) or allergy (eosinophilia) |
| Differential white blood cell count | Diff | Specific patterns of WBCs; type of infection; ability to fight infection |
| Red blood cell count | RBC | Ability to carry oxygen from lungs to blood tissues and carbon dioxide from tissue to lungs; anemia |
| Hematocrit | Hct | RBC mass |
| Hemoglobin | Hgb | Main component of RBCs; ability to transport oxygen and carbon dioxide |
| Red blood cell indices | Diagnosis of anemias | |
| – Mean corpuscular volume | MCV | Hct% x 10/RBC |
| – Mean corpuscular hemoglobin concentration | MCHC | Hgb x 100/Hct% |
| – Mean corpuscular hemoglobin | MCH | Hgb x 10/RBC |
| Stained red cell examination | ||
| – Red blood cell distribution width | RDW | SD of RBC size x 100/MCV |
| – Reticulocyte % | Retic % | Total retic/,1000 RBCs x 100 |
| Platelet count | Plt | Ability to clot and control bleeding |
| Mean platelet volume | MPV | Uniformity of platelet size |
SD = standard deviation.
2.2.3 Other diagnostic fluids
Urine is composed of urea and other organic and inorganic waste products and can provide information about the body’s major metabolic functions. It is readily available and easily collected, so urinalysis can be a valuable metabolic screening procedure. Stool studies may be helpful in diagnosing gastrointestinal disorders. Cerebrospinal fluid (CSF) is a clear fluid formed within the ventricles of the brain, which circulates from the ventricles into the space surrounding the brain and spinal cord, helping to regulate intracranial pressure, supply nutrients to tissues, and remove waste products. Most CSF constituents are present in the same or lower concentrations as in the blood plasma; however, disease can cause elements typically restrained by the blood-brain barrier to enter the spinal fluid. CSF can be obtained by lumbar puncture and is the main diagnostic tool for neurologic disorders such as meningitis, subarachnoid hemorrhage, CNS malignancy, and multiple sclerosis.
2.3 General blood tests
The complete blood count (CBC) is a basic screening tool and is one of the most frequently ordered laboratory tests. The findings in the CBC give valuable diagnostic information about the hematologic and other body systems, prognosis, and response to treatment. The CBC consists of a series of tests that determine number, variety, percentage, concentrations, and quality of each of the basic types of blood cells (Table 2.2). The shorthand notation for common hematology values is illustrated in Figure 2.1.
Figure 2.1 Shorthand notation for common hematology values.
2.3.1 Hematopoiesis
Hematopoiesis is the production and differentiation of blood cells from hematopoietic stem cells. Stem cells reside in the bone marrow and have the ability to give rise to all types of blood cells (multipotency), and they also have the capacity to self-renew. Hematopoietic stem cells differentiate into two lineages of cells, myeloid and lymphoid progenitor cells. With the aid of growth factors, these cells proliferate and mature into their end product blood cells. Numerous growth factors stimulate and regulate the production of all types of leukocytes (white blood cells). Erythropoietin, a growth factor secreted into the bloodstream by renal tubular epithelium, is required for a myeloid progenitor cell to become an erythrocyte (red blood cell), and thrombopoietin is a growth factor produced by the liver and kidney that regulates production of thrombocytes (platelets).
2.3.2 Red blood cells
The main function of erythrocytes is to carry oxygen from the lungs to the body tissues and to transfer carbon dioxide from the tissues to the lungs. The average lifespan of the erythrocyte is 120 days. Hgb is the main component of the red blood cell (RBC) and serves to carry the oxygen and carbon dioxide. The RBC is shaped like a biconcave disk to provide more surface area for the Hgb to combine with oxygen.
Hgb is synthesized in erythroblasts (immature red blood cells) and requires folic acid and vitamin B12 for full maturation. The Hgb molecule is a complex structure that is comprised of a heme (porphyrin) ring with ferric ions and protein components. When erythrocytes are broken down, the heme ring of the Hgb is transformed to bilirubin and metabolized through the liver (therefore, increased bilirubin is an indicator of liver dysfunction; section 2.4.1), and the iron is recycled back into newly generated erythrocytes.
2.3.2.1 Basic tests of red blood cells
Anemia occurs when there is decreased Hgb, caused by a reduction in the number of circulating erythrocytes, the amount of Hgb (an indirect measure of cell mass), and/or the volume of packed cells (hematocrit [Hct]). Since the RBC, Hgb, and Hct counts are closely related, these values are typically evaluated together as part of the CBC, and reference values are pre/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses