7 Oral Infection
7.0 INTRODUCTION
Oral infections caused by bacteria, fungi, and viruses are commonly encountered in the general population, and the risk of infection increases dramatically in patients who are immunosuppressed or experiencing salivary gland hypofunction. In the majority of situations, an appropriate clinical diagnosis can be made without the need for laboratory investigation; however, diagnostic testing may be necessary in cases where the clinical presentation of oral infection is abnormal or subdued (which is common in severely immunocompromised patients), or when the diagnosis is known but the infection is non-responsive to standard empirical therapy. Consideration of a patient’s risk for infection, as discussed in chapter 4, is an essential component to preventing, diagnosing, and managing patients with oral infections.
7.1 Bacterial infection
Most oral bacterial infections are polymicrobial and of odontogenic etiology and can generally be attributed to an offending tooth and/or supporting structures following clinical and radiographic examination (see chapter 6). Salivary gland and bone infections are far less common but may have a bacterial etiology. Rarely, in the setting of profound and prolonged immunosuppression and/or immunocompromise, non-odontogenic mucosal bacterial infections (e.g., necrotizing stomatitis) may be encountered. In addition, although infrequent, oral bacteria can be isolated during episodes of bacteremia or at distant sites of infection (see chapter 4).
7.1.1 Tests of bacterial infection
Bacterial culturing can be a useful and in some cases critical laboratory test with which all dentists should be familiar (Table 7.1). In the absence of purulence there is no clinical indication for bacterial culturing; results will invariably demonstrate normal oral flora. As most abscesses of odontogenic etiology respond to standard narrow- (e.g., penicillin) or extended- (e.g., amoxicillin) spectrum antibiotics, culturing is generally reserved for cases that are non-responsive after at least 48 hours of empiric therapy, so that antibiotic susceptibility testing can be performed. Both aerobic and anaerobic cultures should be collected, and antibiotic susceptibility testing should be requested. For aerobic culture, purulence is sampled directly with a sterile swab and placed with the tip forward into the culture tube and sealed. Anaerobic culture samples for facultative anaerobes should be immediately transferred to transport vials, while strict anaerobe culturing may require a needle aspirate to minimize exposure to oxygen (Figure 7.1). Reporting of results will vary based upon standards at individual laboratories. Non-specific bacterial growth may simply be reported as “normal oral flora,” and if abnormal growth is noted, specific organisms are listed. The presence or absence of anaerobes is specified when an anaerobic sample is submitted. Despite optimal technique, it must be recognized that some species are more likely than others to be isolated and identified from clinical specimens; therefore, culture and antimicrobial susceptibility testing results must always be critically interpreted.
Table 7.1 Outline of oral infections, including etiology, clinical presentation, diagnosis, and management.
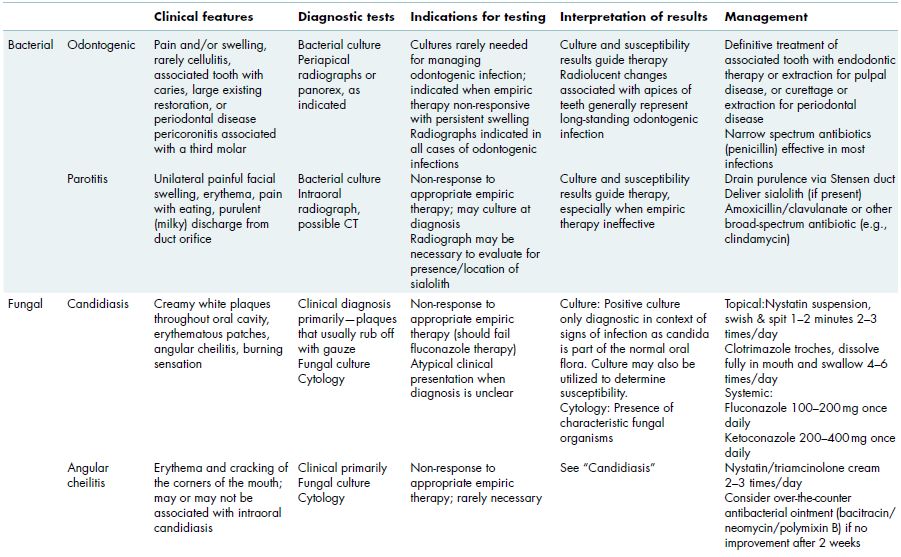
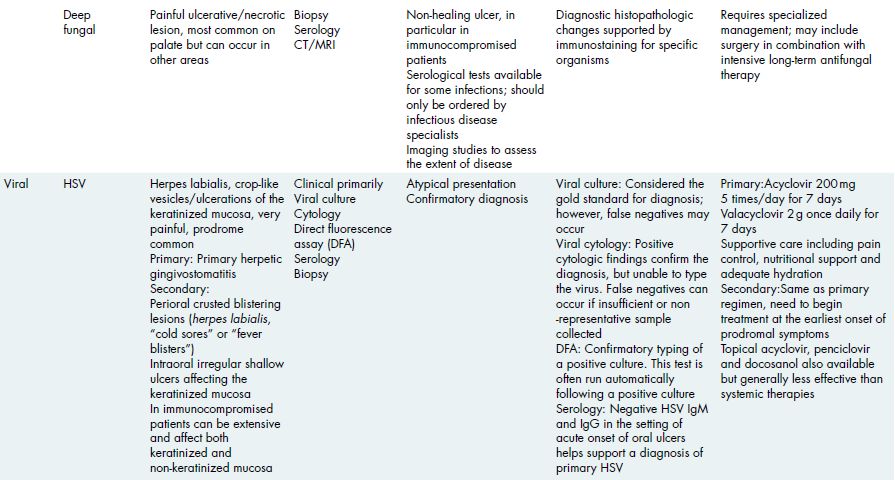
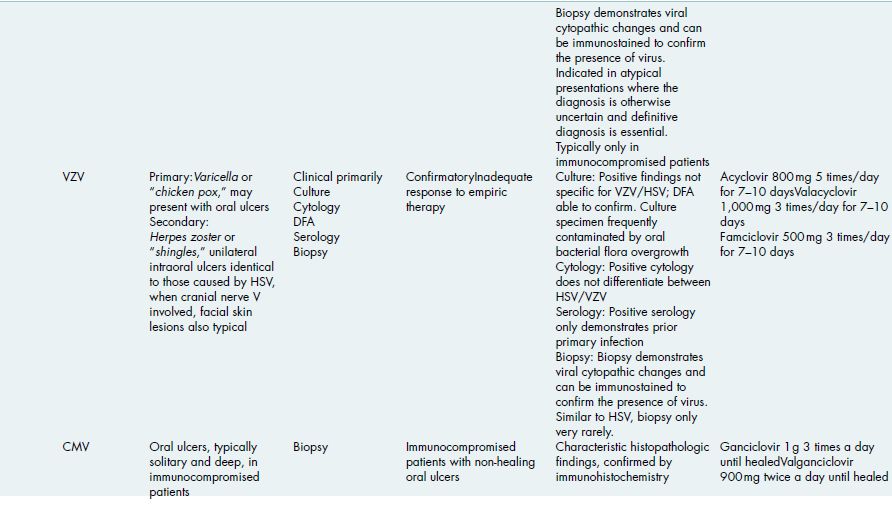
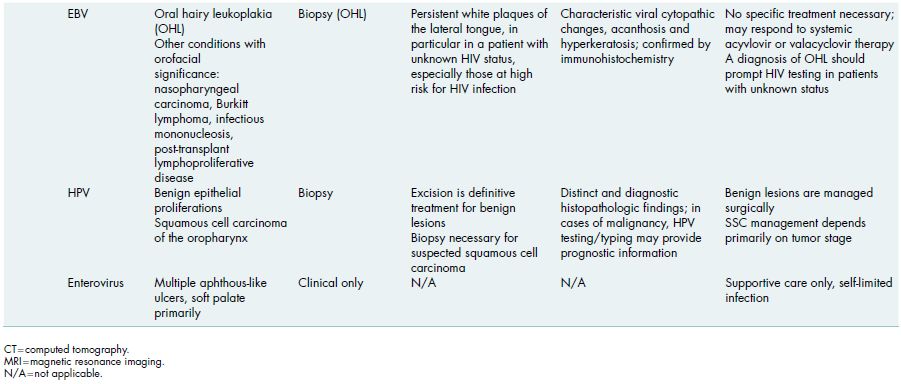
Figure 7.1 This patient with antiresorptive medication-associated jaw osteonecrosis developed a large abscess that was non-responsive to empiric antibiotic therapy. For aerobic culture, the purulent discharge is directly swabbed; however, for anaerobic culture, purulent material should be collected from within the abscess minimizing exposure to air.

Other oral infections that may result in purulence include bacterial parotitis, osteomyelitis, and secondary soft tissue infections associated with osteonecrosis (see chapters 5 and 10). While extremely rare, tuberculosis can manifest with secondary oral lesions that typically present as non-specific ulcerations of the tongue and require incisional biopsy for diagnosis.
7.1.2 Antimicrobials and spectrum
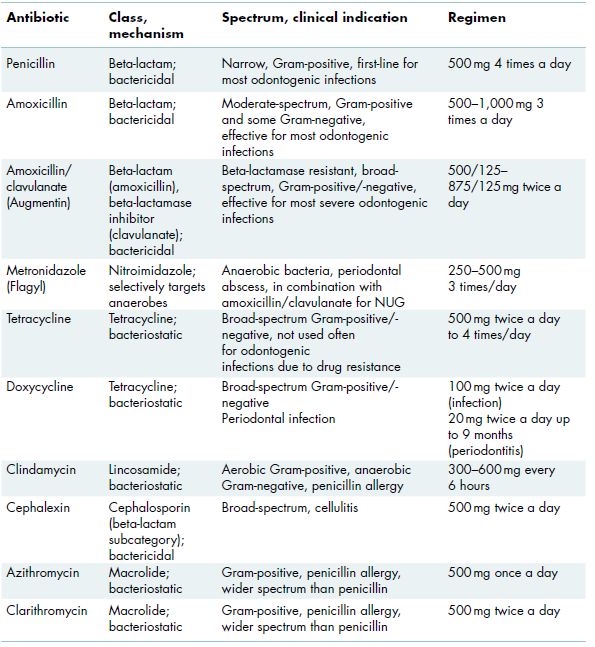
Antimicrobial therapy, whether empiric or based on laboratory results, should always be prescribed according to established or conventional regimens and taken compliantly by the patient for the prescribed duration (Table 7.2). Prescribing the correct antibiotic dose and for an adequate duration is as important as selecting an appropriate antibiotic. Narrow-spectrum antibiotics should be utilized as first-line empiric therapy since these agents are generally efficacious in treating the majority of odontogenic infections.
Table 7.2 Antibiotics commonly used in the management of odontogenic infections.
7.1.2.1 Topical therapy
Topical antimicrobial therapy can be an important adjunct for management of periodontal disease and secondary soft tissue infection, such as that commonly seen in cases of jaw osteonecrosis. Chlorhexidine gluconate used as a 0.12% topical solution is rinsed for up to 1 minute, twice daily. Chlorhexidine rinses have not been shown to reduce rates of caries or calculus formation, and abscesses require systemic antibiotics with or without surgical intervention.
7.1.2.2 Systemic therapy
In general, for any given infection, the most targeted antibiotic with the narrowest spectrum of activity should be utilized. Antibiotics can be bacteriostatic or bacteriocidal, and it is generally best to avoid using combinations of both types of agents concurrently due to potentially competitive mechanisms (Table 7.2). For most odontogenic infections, penicillin is effective, and in the case of a penicillin allergy, clindamycin can be used. For acute suppurative parotitis, a broader-spectrum antibiotic such as amoxicillin, amoxicillin/clavulanic acid, or clindamycin should be considered.
Figure 7.2 Pseudomembranous candidiasis of the buccal mucosa and soft palate in a patient on topical steroid therapy for management of oral lichen planus. Some of the white/yellow plaques are more confluent than others.

7.2 Fungal infection
Nearly all oral fungal infections are caused by Candida albicans or other Candida species, which are considered to be normal components of the oral microflora. When the highly balanced oral microbiologic ecosyst/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


