Chapter 12
Endodontic Management of the Aging Patient
Harold E. Goodis1 and Bassam M. Kinaia2
1 University of California School of Dentistry, San Francisco, CA, USA; Boston University Institute for Dental Research and Education, Dubai, UEA
2 Department of Periodontology and Dental Hygiene, University of Detroit-Mercy School of Dentistry, Detroit, MI, USA
Introduction
At the turn of the 19th into the 20th century, life expectancy was to the mid 50s. In the 21st century, men can live into their late 70s with women’s expectancy estimated to extend into the mid-80s. The aspect of living longer does not necessarily mean that people will live better. In dentistry, extension of life expectancy has led to the need for care of the oral cavity using new methods, materials, and technologies. In many instances, this presents clinicians with challenges of care modalities that were not expected (Centers for Disease Control and Prevention, 2012). The dental needs of the aging patient in the 21st century appear to be very different and more complex than those experienced by older patients in the mid to late 20th century (Chalmers, 2006a,b). As the population ages, people are taking more medications that may benefit their general health but not necessarily their dental or periodontal health (Ciancio, 1996). (See Chapter 11 for a discussion of periodontal disease.) Because we are living longer, more people suffer from chronic medical problems and diseases than those whose lives ended in earlier ages. As written in a newspaper opinion piece, treating today’s aging patients many times appears as if dentists are attempting to relate to very young children, but without the “giggles and glee” (Fieler, 2012). The writer remembers his father saying that there were parallels between “… caring upward and caring downward on the family tree.” Many middle-aged people are caring for their parents, in their own home or in a managed care facility. Emotionally, everything appears to be backward “… taking care of someone who once took care of you.” Mr. Fieler concluded with a profound statement, “… the lessons your children don’t want to hear from you today are the same ones you don’t want to hear from them later.” That sentiment causes patients who are aging of attempting to understand the need for procedures that they don’t expect nor understand. Therefore, the need for a root canal procedure can be daunting to them. Explaining not only the need for such a procedure but what it entails as far as what is done to a 70, 80, or even a 90-year-old patient may take up more time than one can imagine.
The need for dental care in aging patients is a multi-phase situation and those needs grow yearly. Many of these patients will receive necessary care but many won’t, primarily because of what occurs in teeth and oral soft tissues that many care providers have never treated. Therefore, this chapter will discuss the treatment regimens used in root canal therapy of older patients, compare, when applicable the form and function of the tooth, dental pulp, and dentin in young versus aging individuals, and the management of this treatment modality in an environment much different than that usually seen in private practice. The reader will find that, in many instances it is impossible to describe either clinical findings or step-by-step procedures. However, references to appropriate, published articles from refereed journals and textbooks will be suggested to supplement the information in this chapter. Thus, the following will be divided into a discussion of the structure of the inner and outer tissues of the tooth and the changes that occur over time, both physiologic and pathologic, that lead to a different way of treating a large group of patients who need what can be considered primary care.
The dental pulp
The developing soft tissue of an adult and aging individual’s tooth is a complex tissue surrounded by relatively hard tissues (Figs 12.1a,b & 12.2a,b). The dental pulp has several functions in a developing tooth, but in an adult tooth the pulp functions in a manner that is protective in nature. The protective mechanism, as in tissues throughout the body, warns us when something is wrong. In the pulp, the peripheral sensory nervous system composed of two types of pain fibers (neurons) and functions in a way that not only warns the individual that there is a problem but leads, in many instances, to proper diagnoses and treatment plans (Hargreaves et al., 2012). These neurons are called the A delta and C fibers and, because they are located in different areas of the pulp, respond to different stimuli. The response is usually one of pain that may differ in length, severity, location, and stimulus (Hargreaves et al., 2012).
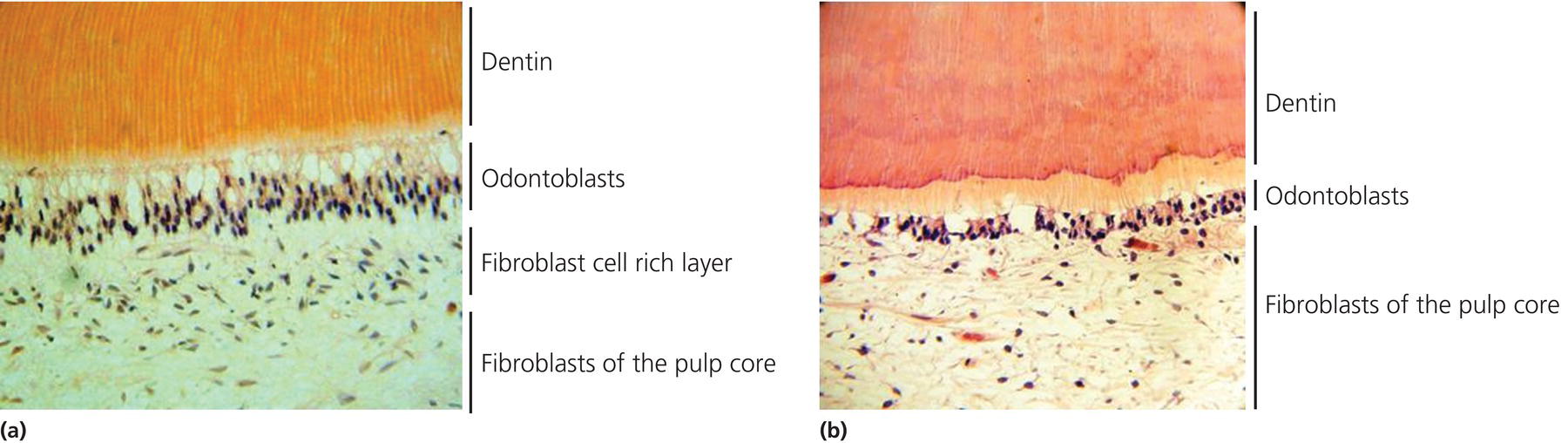
Figure 12.1 (a) Histologic section of the dental pulp complex of a young tooth (15 years old). Note the dense odontoblast and cell-rich zones. (b) Histologic section of the dental pulp complex of a 59-year-old patient. Note the lesser number of odontoblasts present.
Figures courtesy of Dr. Peter Murray, Nova Southeastern University.
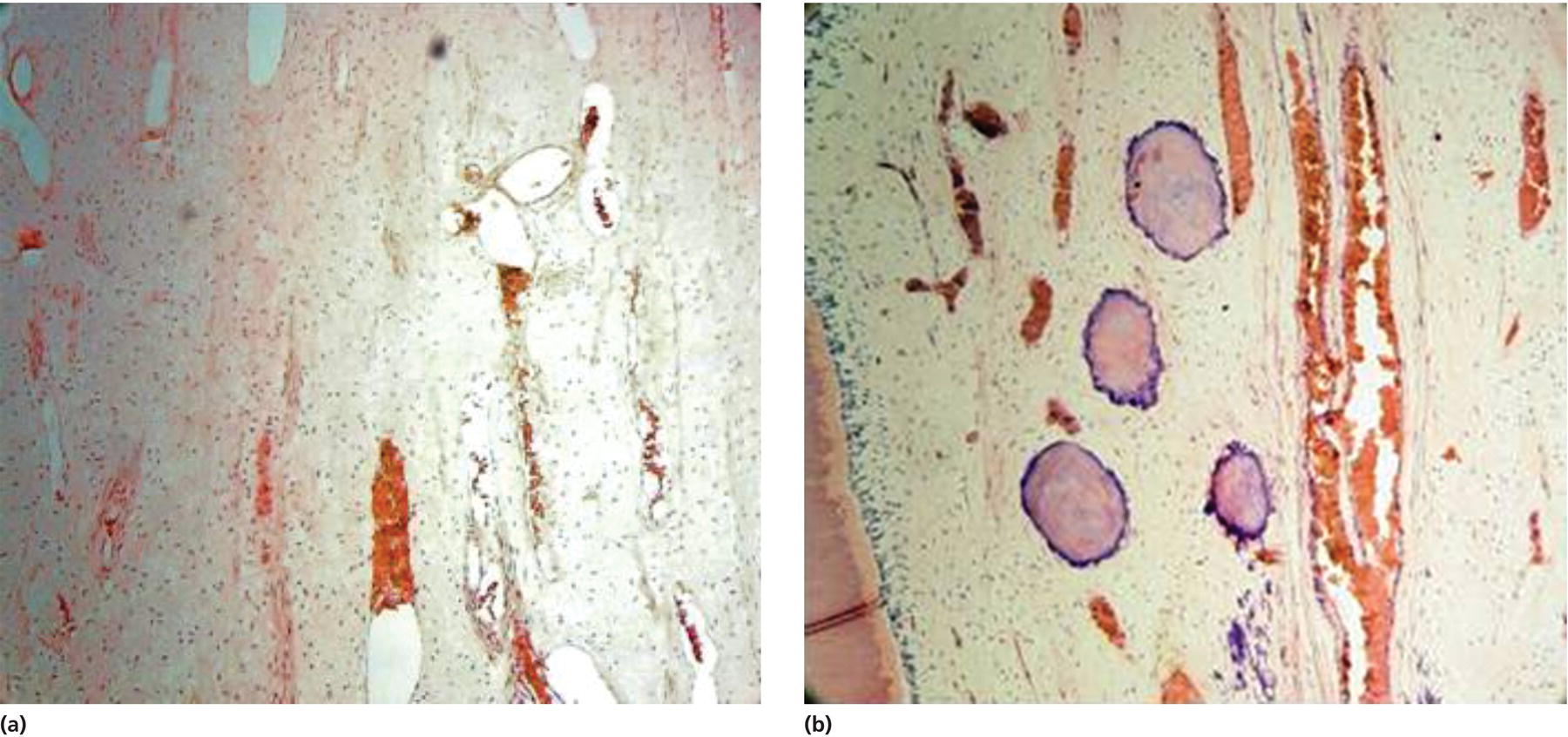
Figure 12.2 (a) Histologic section of the dental pulp complex of a young tooth (15 years old). Note the highly vascularized tissue. (b) Histologic section of the dental pulp complex of a second 59-year-old patient. Note the lesser number of odontoblasts present. Also note the calcifications found in the pulp tissue.
Figures courtesy of Dr. Peter Murray, Nova Southeastern University.
The dental pulp has an infinite capacity to heal itself, not an unusual event in the body as many tissues do the same when injured. Pulp tissue submitted for histologic examination demonstrated the effects of multiple challenges to the tooth, including caries (initial and recurrent), marginal bacterial micro-leakage of restorations, direct trauma, and iatrogenic procedures such as cavity preparation (Bernick & Nedelman, 1975; Hillmann & Geurtsen, 1997; Nielsen, 1983; Stanley, 1961). All affect the pulp, causing an inflammatory response, which will initially be pathologic, but can become physiologic, since the initial inflammatory response can lead to repair with possible regeneration of the pulpal tissue (Cooper et al., 2010).
The dental pulp tissue is considered a low compliance tissue due to its location and the types of tissues surrounding it (Kim, 1985a). First, the pulp is a relatively large volume of tissue with a relatively small vascular supply. The largest artery to enter the pulp is the arteriole and the largest vessel to exit the pulp is the venule; therefore, the vascular system is referred to as a microcirculation. Second, the pulp is a terminal circulation with few, if any, vessel anastomoses. Multi-rooted molars have demonstrated anastomoses in the root portion of the tooth. Therefore, the ability to shunt blood from and to an inflamed area is not possible and may compromise repair when injury occurs. Last, the pulp is surrounded by relatively hard, unyielding, dentin walls, which inhibits and, in many instances, completely suppresses the ability of the pulp to swell, as occurs in other soft tissues such as skin and muscle (Kim, 1985b). Taken together, the above mitigates toward an adverse ability to be protective in nature as it is designed to be. In sum, the potential for the dental pulp to repair itself is infinite. However, aging individuals have limitations for repair or regeneration of pulpal tissues due to limited blood supply, sensory deficits due to fewer neurons, and reduction of the pulp canal space resulting in less tissue available for repair to occur (Bernick & Nedelman, 1975). Therefore, the evidence points to the need for well-controlled root canal therapy to retain a tooth that may appear to be the easiest treatment rather than the best treatment (Trope, 2008). The potential of the dental pulp for healing is limitless. However, aging individuals have limitations for repair and regeneration. This is due to a limited blood supply, sensory deficits due to fewer neurons, and lesser amounts of pulp tissue due to continued mineralization of the tissue space (Trope, 2008).
Dentin and the odontoblasts
Normally the pulp of the developing and adult tooth, as described above, has the ability to form the matrix that becomes three types of dentin. Primary dentin is formed as the tooth develops with a structure that is tubular in nature. Secondary dentin begins to form as the tooth completes its form and erupts. It also contains a tubular structure with its tubules being continuous with those of primary dentin. The formation of secondary dentin continues throughout the life of the tooth and is physiologic in nature, unless there is an injury or challenge to the pulp (Smith et al., 1994, 1995) (Fig. 12.3a,b,c). Tertiary dentin generally occurs in teeth that have been injured in some manner (i.e., caries). It is not tubular in its formation but rather occurs as a solid kind of structure.
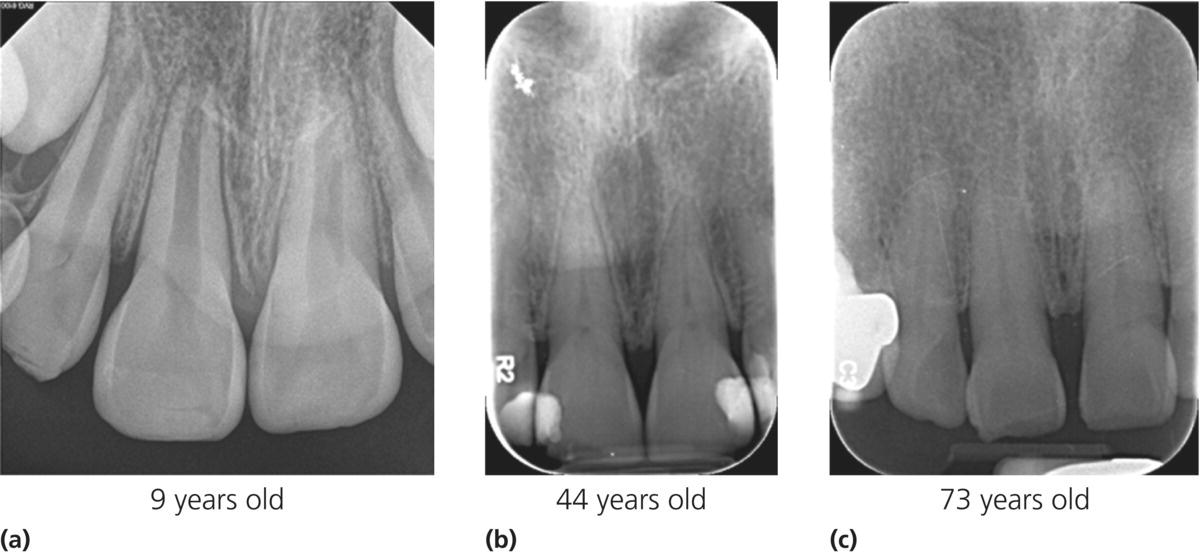
Figure 12.3 (a) A 9-year-old patient with typically young incisors. Note the size of the root canal systems and the incomplete root end development of the three teeth pictured. (b) A 44-year-old patient with restored maxillary central incisors. Note the great change in the size of the root canal spaces, partially attributed to the mesial and distal deposition of tertiary dentin due to composite placement. (c) Maxillary right lateral incisor and central incisor of a 73-year-old patient. Note the absence of restorations with no history of trauma. When compared to Fig. 12.9, the physiologic deposition of secondary dentin is evident.
Figures courtesy of Dr. Franklin Tay, Medical College of Georgia.
The importance of dentin cannot be overstressed. Therefore, it is the dentin that in fact may be considered as the partner to the pulp due to its location adjacent to the pulp (the pulp–dentin complex). Dentin’s tubular structure contains pulpal fluid and the projecting arm of the odontoblast, the odontoblast process. The odontoblast is responsible for the initiation of dentin matrix formation that becomes mineralized over time and again acts as a protective mechanism (Holland et al., 1985, 1994). The odontoblasts do not undergo mitosis nor they are replaced, unless the pulp is challenged, and continues to act as stated above. However, given the fact that humans are living longer, it is apparent that continued formation of secondary dentin may begin to narrow the root canal space as individuals age to a point that it may be difficult to perform a root canal procedure. Men will demonstrate narrowing of the root canal space in their 40s and it is not impossible that the entire upper and middle portions of the root canal system may be mineralized (Woo, 2001) (Fig. 12.4a,b,c). This event is a reminder that a completely physiologic process may become a pathologic process due to aging (Fig. 12.5a,b,c). Tertiary dentin is the last form of that hard tissue. It forms in response to an injury to the pulp caused by caries etc. Tertiary dentin is not physiologic but pathologic. Its matrix mineralizes as an atubular structure in response to placement of certain materials next to or over an exposed pulp. Tertiary dentin is of two types: reactionary where the dentin matrix is formed by surviving odontoblasts; and reparative dentin formed by a generation of new odontoblast-like cells, which are cells that may act differently than the original cells (Pääkkönen et al., 2009). The formation of tertiary dentin in response to a stimulating type material, such as calcium hydroxide (CaOH2), also narrows or closes the root canal space, but much more rapidly than secondary dentin. The new dentin formed also may lead to further closure of the root canal space and cause a nonresponse to temperature stimulation.
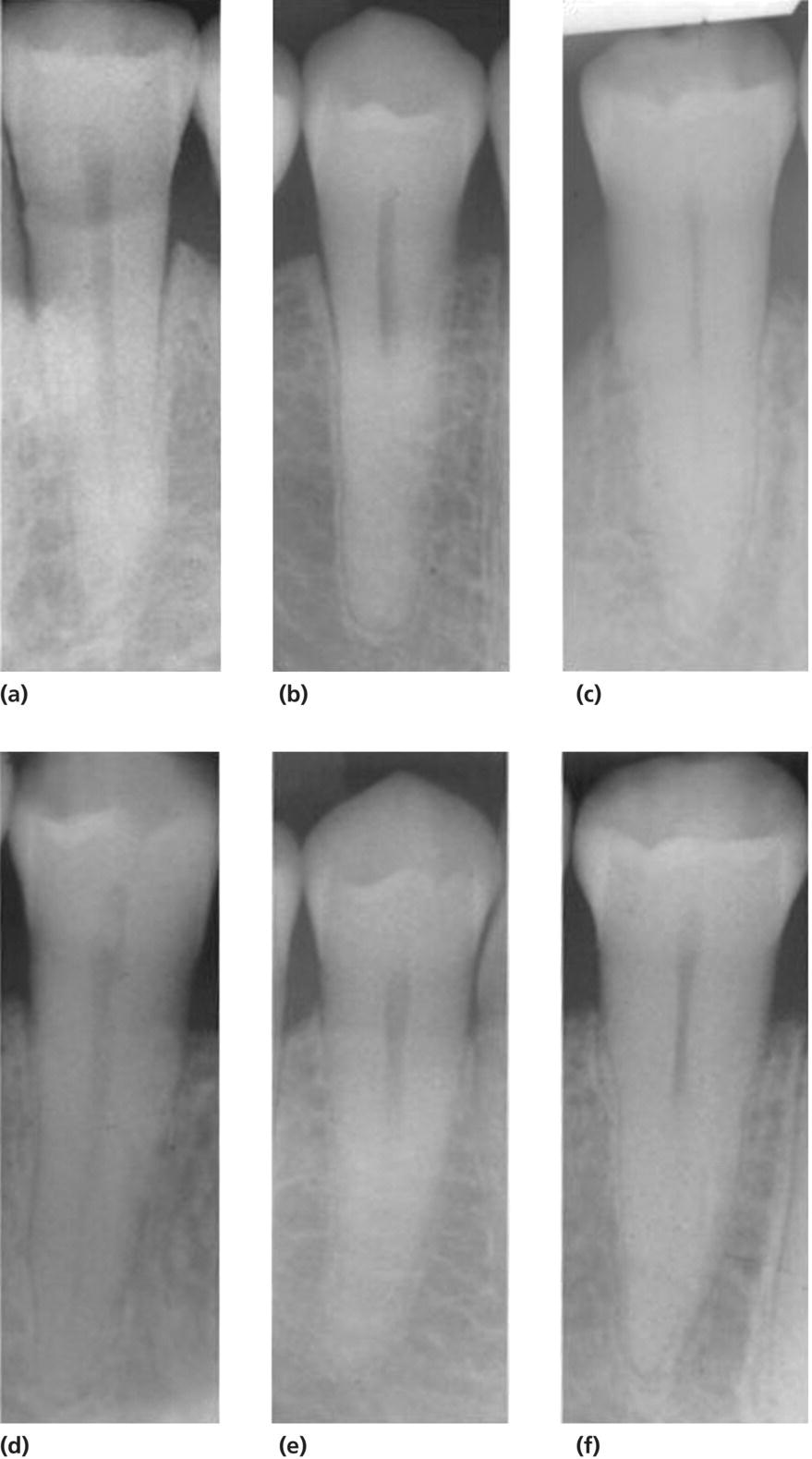
Figure 12.4 Periapical radiographs of a premolar taken of a male patient at three times over a 40-year period. (a) Mandibular first premolar at age 33. The root canal system can be seem to the apex of the tooth. (b) The same tooth at age 52. (c) The same tooth at age 73 years. The same pattern is seen in a second patient at the same time frames (d, e, f).
Courtesy of Woo, 2001.
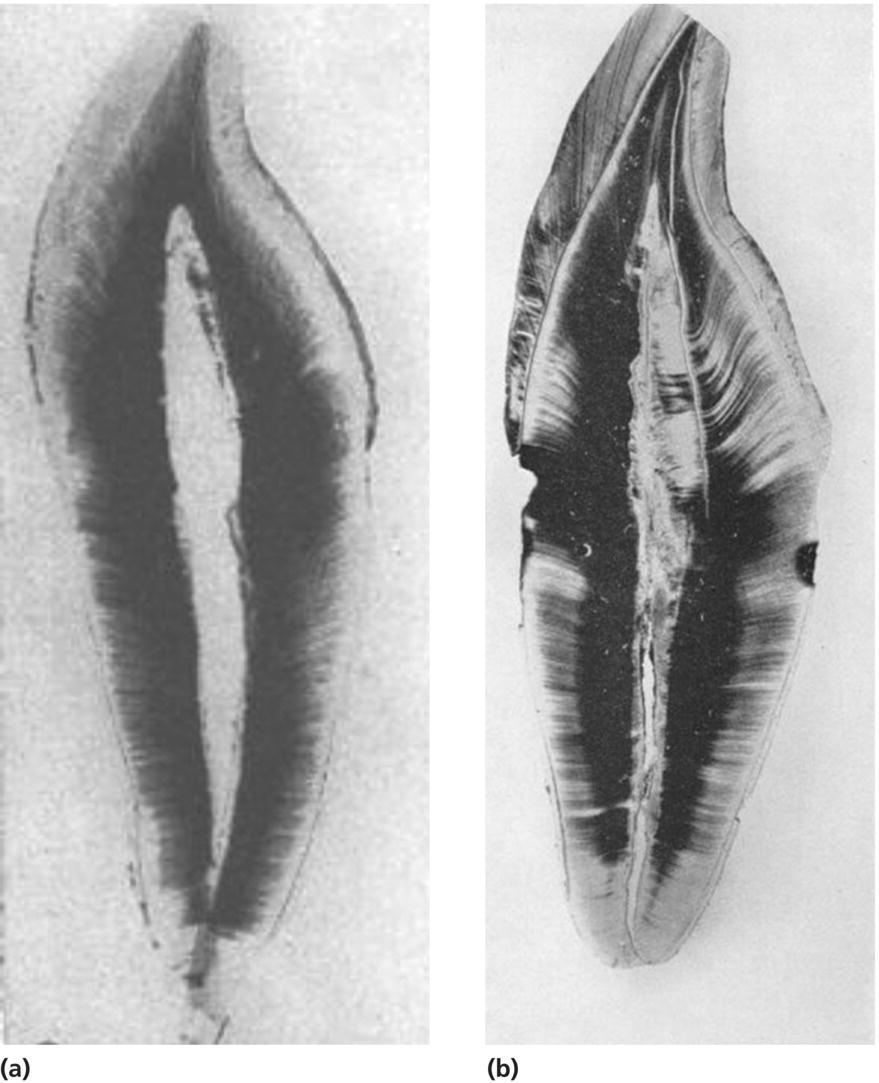
Figure 12.5 (a) Low power photomicrograph of an unstained root canal space (ground section) of an upper central incisor typical of a 26–30-year-old individual. Note the size of the root canal space (Original mag. ×20). (b) Low power photomicrograph of an unstained root canal space (ground section) of an upper central incisor typical of a over 71-year-old individual. Secondary dentin fills the entire pulp chamber of the root canal space. Note that the secondary dentin formation is tubular as opposed to atubular dentin. Its formation is due to age and not to caries or placement of restorations.
Courtesy of Philippas & Applebaum, 1966.
A normal dental pulp demonstrates its ability to survive throughout life. As mentioned above, the odontoblast, with its process extending into the dentinal tubules, is the cell responsible for formation of the dentin matrix. When caries are present (Stanley, 1977), and initially removed, the odontoblastic processes are cut, effectively causing the odontoblast to die. There are sufficient numbers of odontoblasts so that dentin continues to form. However, repeated placement or replacement of restorations, combined with marginal bacterial microleakage, may cause all odontoblasts in the area to die; therefore, the remainder of the tissue depends on formation of odontoblast-like cells to form a matrix that will result in tertiary dentin (About et al., 2001; Couve & Schmachtenberg, 2011; Couve et al., 2012; Murray et al., 2000). Eventually, the remaining pulp tissue becomes overwhelmed and the remaining tissue becomes necrotic. In these cases, depending on the age of the patient, the patient’s ability to sit for a period of time in the dental chair and the condition of the patient’s teeth (caries, fractured cusps, lost restorations, periodontal status, and restorability), treatment choices may become overwhelming.
Sensory mechanisms
As mentioned above, the adult dental pulp attempts to function as a protective mechanism. As people age, the root canal space contracts, limiting the number of cells remaining in the pulp to be able react positively to an adverse stimulus. Therefore, aging also leads to decreases in the number of sensory (pain) nerves present in the pulp (Bernick 1962a, 1967a; Fried, 1992; Fried & Hildebrand, 1981; Matysiak et al., 1986, 1988).
The presence of tertiary dentin may be capable of blocking peripheral pain fibers from being stimulated in a manner that will allow the patient to sense pain. Contracture of the pulp space limits the amount of pulp tissue present and can affect those remaining nerves in the body of the remaining pulp tissue, again limiting the ability to respond to an adverse stimulus. These events may compromise patient’s responses to tooth testing, especially to applications of testing with cold or heat. The responses occur through stimulation of sensory neurons located in and around odontoblasts and within the body of the pulp. More recent studies appear to indicate that odontoblasts also may have a sensory function (El Karim et al., 2011; Magloire et al., 2010; Okumura et al., 2005; Son et al., 2009). This is an important finding since aging individuals have fewer odontoblasts and, if the pulp has been injured, the odontoblast-like cells may not function as did the original odontoblasts functioned. These studies have expanded the sensory ability of the dental pulp to respond to injury, and indicates that the dental pulp sensory pain mechanisms are much more complex that originally believed.
Since the tissue responds to injury to protect the remaining pulp by formation of odontoblast-like cells, the neural response in these situations may or may not be diagnostic. The formation of tertiary dentin may prevent contracture of dentinal fluid and movement into the pulp through what now may be obliterated tubules; hence, no or weak responses to cold. On the other hand, the atubular dentin may block the ability of a heat stimulus from reaching the body of the pulp to allow increase in temperatures to a level that patients will respond to heat (Zach & Cohen, 1962, 1967). The pulp has a greater tolerance in young people to decreases in temperature, therefore indicating that a coolant must be cold enough to elicit responses. The tissue is less tolerant to increases in pulp temperatures as responses generally occur with temperatures rising 5–7 degrees (Zach & Cohen, 1962, 1967). Ultimately, the main factor continues to be limitation of root canal space and decreases in the numbers of sensory neurons, lessening the patient’s response being realistic.
Vascularity
The same limiting events occur with the vascular supply to the dental pulp. The microcirculation in normal pulp tissue maintains vitality. But as individuals age and the root canal system narrows due to continued secondary or tertiary dentin formation, fewer and smaller vessels are available to allow normal blood flow (Bernick, 1962b, 1967b, 1972). While the radicular vasculature is still effective, the gradual narrowing of the pulp volume indicates a diminished blood flow in the tissue (Domine & Holz, 1991). The metabolic ability of the dental pulp decreases gradually and the capillaries in the sub-odontoblasts become thinner with aging (Ma et al., 1997). Interestingly, one could say that, of everything being equal, an individual living well into his or her 90s, who presents with what appears to be a completely calcified root canal system, would have been thought to have had a perfect root canal therapy without treatment. However, a remnant of pulp tissue remains apically but has no blood supply, and a lesion will be seen apically on a radiograph. Such a case would eventually require treatment, most often surgery. Unlike an event due to trauma, a 90-year-old patient’s root canal closure would be due to a normal physiologic event of secondary dentin deposition throughout life. If that patient should require surgery, the situation and management changes and, depending on the health of the patient, treatment becomes more difficult (Eldarrat et al., 2010; Kvaal et al., 1994).
Management considerations
Diagnosis
Tooth testing
The need for a correct diagnosis in any treatment situation is a necessity. Tooth testing can be quite subtle or quite dramatic. The subtlety of endodontic diagnosis is being able to understand pain responses to temperature changes and other stimuli to understand whether the patient presents with a reversible or irreversible pulpitis. For example, a response to a cold stimulus that disappears as soon as the stimulus is removed from the tooth is generally a reversible pulpitis. This indicates that the problem is something other than an irreversible pulpitis, as seen in fractured cusps, caries, or recurrent caries. The key to the diagnosis is that the symptom occurs because underlying dentin has been exposed. Covering the dentin with a new restoration after caries removal or removal of a fractured cusp tip ends the pain. On the other hand, a response to a heat stimulus that lingers for some time or beginning many seconds to a minute or two after removal of the stimulus is indicative of an irreversible pulpitis. In older patients, these responses can be quiet dramatic, with loud and painful responses and a look that will say that the patient believes he or she is in the wrong office.
As stated above, tissues change in the aging patient. While dentists are capable of making a correct diagnosis in older patients, they must remember to be more “patient” with their “patients” who are older. An axiom of tooth testing for pulpal and periradicular diseases, whatever the age of the patient, is to listen to the patient! So often, especially in a busy practice, practitioners think that they can take a radiograph and immediately form a diagnosis and treatment plan without patient input. Believe it or not, patients do have a clue as to which tooth is causing the problem. However, with older patients, especially those experiencing pain and with a history of several medical conditions, the dentist must understand the possible difficulty of getting to the “root” of the problem.
First, aging patients tend to be more anxious, thinking that everything touching a particular tooth causes pain. They will try to help by responding immediately to a temperature test when a cotton swab without a stimulant touches their tooth. When asked what they felt, they can’t say. Therefore, each and every test used in the diagnostic process must be thoroughly explained to the patient. There have been many older patients who respond to a stimulant placed on the pontics of a fixed appliance. (A not uncommon event in the author’s office [H.E.G.].) Second, they ask many questions, sometimes asking the same question several times, either because they don’t understand or have a dementia and don’t remember the answers. Older patients also have the need to attempt to dictate what type of treatment they require. It is, therefore, necessary to schedule more time with aging patients than normally would be required for a younger patient. Remember again that an aging patient’s responses are not necessarily what a younger patient would report. With the root canal space compromised, either physiologically or pathologically, there may be no response to temperature-testing methods in what may ordinarily be a reversible pulpitis that turned into an irreversible pulpitis, because of recurrent caries or a fractured tooth structure present that can be treated without a root canal procedure. This may complicate the necessary treatment. A necrosis with a sinus tract and radiographic evidence of a lesion may be the easiest diagnosis to make and treat. The use of an electric vitalometer, especially after explaining how the device works, will sometimes frighten an older patient. Because of its limited ability, due to the need to be used only on tooth structure, in routine testing it should not be used for the aging patient. Older patients will always tell their friends how they were “electrocuted” in the dentist’s office. A good rule to follow is to never test the suspected tooth first. Test the adjacent, opposing or contra-lateral tooth first, then the suspected tooth last. This not only demonstrates to aging patients that they will not be hurt, it will also be a baseline for the patient’s responses.
Once the dental pulp becomes inflamed, the overriding symptom is the onset of pain. Since the volume of tissue in the root canal space of a young individual is relatively large, as opposed to older patients with much less tissue, diagnosis generally does not pose problems. Testing regimens are based on careful questioning of the patient to elicit as much history and information as possible. The input from the patient leads to the type of tooth testing that may be necessary to properly diagnose the problem. Since pain to temperature, either hot or cold, is a cardinal symptom of a pulpitis, this may be the best place to start. This, of course, occurs after a full intraoral and extraoral examination.
In many instances, symmetry of facial areas will have changed due to internal swelling in the mouth. Therefore, the testing begins with the easiest and most common tests prior to other, more complicated tests. When a necrosis is suspected and the pain complaint comes from chewing hard food or swallowing, with normal occlusion, the use of a mirror handle to gently percuss teeth is enough to cause a response. Differentiating between pain when percussing in a vertical direction, for periradicular pain, and in a bucco-lingual direction helps in understanding the possibility of a periodontal problem rather than an endodontic problem. (Don’t forget to take periodontal gingival sulcus readings.) Biting on a wet cotton roll, use of a Tooth Sleuth®, or percussing individual cusp tips may disclose the presence of a hard tooth structure fracture that certainly will change the diagnosis and may change the prognosis. The use of the ball of the index finger in the palpation test can pick up disease quickly and effortlessly; slight pressure in the cul-de-sac area is used to define sensitivity.
Since presence of vital tissue is necessary in the crown of the tooth for a response to temperature testing, a problem exists with a nonresponse in older patients. With gingival recession and closure of the root canal system, the remaining pulp tissue may be well below the cervical area of the tooth; hence, a possible nonresponse from an older patient. There is a possibility of periodontal recession that exposes dentinal tubules which curve down and then up to reach the pulp, the hot or cold stimulus may be placed somewhat lower towards the gingival crest of the tooth in an attempt to have a response. Care must be taken in these cases not to involve the soft tissue of the gingival crest which will result in a false positive. If radiographs disclose no periodontal ligament thickening or a radiolucent lesion and pain is the only symptom or sign, difficulties increase as to making a correct diagnosis. Keep in mind the difficulty of attempting to pulp test a child 3–5 years of age. That will make one understand the difficulty of testing that child’s aging grandparents, who are brought to the dentist by the child’s mother or father. A retrospective study concluded that general practitioners were able to detect radiographic changes when they are extensive, but they miss periodontal ligament widening and lamina dura changes (Sherwood, 2012). Remember that loss of restorations, secondary or recurrent caries, and fractured cusps, among other coronal conditions must be intercepted early enough to either prevent a pulpitis from occurring or from suffering the sequelae of a necrotic tooth.
Radiographs
The above is predicated on the fact that properly angled and exposed radiographs have been taken. This part of diagnosis is placed here as, while radiographs are incredibly important, too often dentists will take them first, glance at them when developed or if digital, and never look at them again. Hence, the placing of a radiographic discussion here after the discussion of tooth testing above is important. The dentist must return to view the radiograph after the information of listening to the patient, extraoral and intraoral examinations completed, with tooth testing having been generated. Ordinarily, the presence of a radiolucency at the apex of a tooth that doesn’t respond to testing indicates a necrotic pulp with extension to the periradicular area. That is particularly true in a younger patient but not necessarily true in an aging patient. Being able to diagnose between a lesion of endodontic origin (LEO) and other pathologic entities can be delicate. Obviously, younger patients may present with a greater ability to represent their symptoms and dental history than an aging patient. Simply put, more than one radiograph needs to be taken at a different angle (mesio-distal) after the fully parallel position of the first film. If the lesion moves in the angled film, it’s probably not a LEO. If the pulp tests are normal and there were no symptoms, the lesion will be a lesion other than a LEO; this is true in young and aging patients. Additionally, the angled film may better describe the number of roots present or dilacerations of roots not seen in the first film.
There is a very subtle situation that causes dentists to err in a diagnosis. It is referred to as a thickened periodontal ligament (PDL). Most dentists have never heard of or have forgotten that this entity exists. For example, a young patient will present with radiographic evidence of a thickened PDL. Confounding to the dentist – who believes that the symptoms indicate a pulpitis, which is confirmed by the tooth-testing results being positive to cold but with symptoms not lingering – an irreversible pulpitis is diagnosed and the dentist immediately begins a root canal procedure. As presented above, stimuli responses to cold are expressive of a reversible pulpitis, with exposure of dentin. To have this response in an older person with radiographic evidence of coronal closure of the root canal system may indicate that a deeper fracture is present that extends to the lower lever of the pulp tissue. The subtly of a thickened PDL comes from knowing that it generally indicates a reversible pulpitis (find the exposed dentin, treat it), not an irreversible pulpitis. Remember that conventional radiographs used for diagnosis and management of endodontic problems result in limited information because of the two-dimensional nature of the images produced or the geometric distortion produced by the angulation. (Patel et al., 2009) (The reader is referred to Berman & Hartwell, 2011, and other endodontic texts for a more detailed discussion of endodontic radiographs.)
Other methods of radiographic examination are presently being suggested to increase the ability of the dentist to make a correct diagnosis. Laser Doppler flowmetry (LDF) measures the presence or absence of blood flow in the pulp tissue. The device passes a laser beam through tooth structure that interacts with the red blood cells. The interaction causes a signal to bounce off of the blood cells, that are picked up by a receiver device. The resultant value is automatically converted to a number that indicates flow. The use of this device is limited as the laser beam will not go through metallic restorations and must be carried out in complete quiet with little or any type of airflow. In some instances, someone walking near the device will cause deviations in the values generated. The blood flow from gingival tissues also can cause marked deviations in the readings. However, when the environment is controlled, LDF can be used for research. One study tested 8–75-year-old participants’ pulpal blood flow (PBF) at different ages. Resting PBF decreased with increasing age, indicating a smaller mass of tissue with fewer vessels. When cold was applied to the crown, all blood flow decreased with significance in aging patients (Ikawa, 2003; Jafazadh, 2009). Laser wavelengths also may become the method of choice for cleaning and shaping root canal systems, but the science still in not quite there. Lasers are suggested for treating sensitive dentin and other clinical methodology (Stabholtz
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


