Complex Nonskeletal Problems in Preadolescent Children
Preventive and Interceptive Treatment
The problems discussed in this chapter are more challenging than those addressed in Chapter 11. Even though they are categorically similar, most require more skill to diagnose and treat—especially to carry out the mechanics to achieve proper tooth and root position while managing the reciprocal effects (anchorage) of forces aimed at more complicated tooth movement. General practitioners will need to be selective and match the treatment problems with their skills.
Eruption Problems
Transposition is a rare positional interchange of two adjacent teeth. It occurs with a prevalence of approximately 0.3% and equally affects males and females.1 There appears to be a genetic component to this problem.2
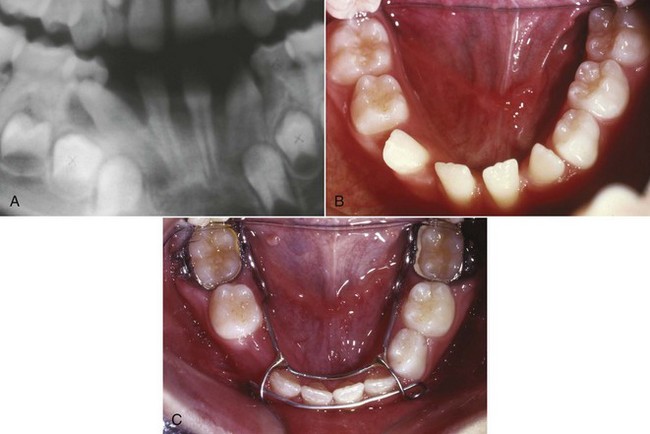
In the early mixed dentition years, transposition can develop when distally directed eruption of the permanent mandibular lateral incisor leads to loss of the primary mandibular canine and primary first molar (Figure 12-1). If left untreated, this can result in a true transposition of the permanent lateral incisor and canine.3 Interceptive treatment requires repositioning the lateral incisor mesially (Figure 12-1, C), which eliminates the possibility of the complete transposition with the canine. This means either bonding the tooth or gaining surgical access to the tooth and applying traction to tip the tooth back to its natural position. In addition to a labial fixed appliance, a lingual arch usually is required for supplemental anchorage. The benefit of this type of early intervention is that simple tipping movement usually can reposition the tooth. Left until later, bodily movement of the erupted teeth is required. One adverse consequence of this early repositioning is potential resorption of the lateral incisor root because it may be brought into contact with the unerupted canine. This is unlikely but should be discussed with the patient and parents prior to treatment. Beginning treatment before the canine is actively erupting is important.
Later in the mixed dentition, the more prevalent transposition is of the maxillary canine and first premolar or maxillary canine and lateral incisor.4 Treatment of transpositions involving the maxillary canine if not addressed early is quite challenging. Moving the teeth to their natural positions can be difficult because this requires bodily repositioning, translating the canine facially or lingually past the other tooth. Careful consideration of alveolar width and the integrity of the attached supporting tissue is required. Often, the best approach is to move a partially transposed tooth to a total transposed position or to leave fully transposed teeth in that position. This requires careful finishing with reshaping the transposed teeth to improve both their appearance and fit within the dental arch. Although this can be difficult, the time and difficulty in correcting the transposition is even more challenging.
Primary Failure of Eruption
Primary failure of eruption is characterized by failure of eruption of permanent posterior teeth when there is no overlying mechanical interference, and now is known to have a genetic etiology5 (see Chapter 5). This usually is noted in the late mixed dentition when some or all the permanent first molars still have not erupted and eruption of other posterior teeth in affected quadrants of the dental arch appears abnormal (Figure 12-2). The affected teeth are not ankylosed but do not erupt and do not respond normally to orthodontic force. If tooth movement is attempted, usually the teeth will ankylose after 1 to 1.5 mm of movement in any direction, so obtaining a genetic analysis and confirmation of the diagnosis can help guide treatment and circumvent unwanted reciprocal forces. In the long term, prosthetic replacement of the teeth that failed to erupt, acceptance of premolar occlusion in affected quadrants, or possibly segmental osteotomies (possibly even distraction osteogenesis) after growth is complete are almost the only treatment possibilities.
Impact of Radiation Therapy and Bisphosphonates
Due to the increased prevalence of successful stem cell transplantation (SCT) and total body irradiation (TBI) for treatment of childhood cancers, more patients with missing teeth and altered tooth morphology are being observed. The early age of SCT (less than 5 years old) is more of a risk factor than TBI.6 Shortened roots are the result of high-dose chemotherapy and TBI, especially when treatment is in the 3 to 5 years age group.7 Because these patients have high survival rates, they now seek orthodontic treatment. Some of the irradiated teeth fail to develop, others fail to erupt, and some may erupt even though they have extremely limited root development. Although the roots are short, light forces can be used to reposition these teeth and achieve better occlusion without fear of tooth loss (Figure 12-3).
Children are increasingly receiving bisphosphonates in conjunction with other aggressive and lifesaving therapies. This drug class has known implications for dentistry and orthodontic tooth movement in particular (see Chapter 8).8 Currently, as these patients reach the age when orthodontic tooth movement will be a possibility, it will be important to assess the impact of this therapy. Orthodontic treatment should not be attempted while bisphosphonates are being used.
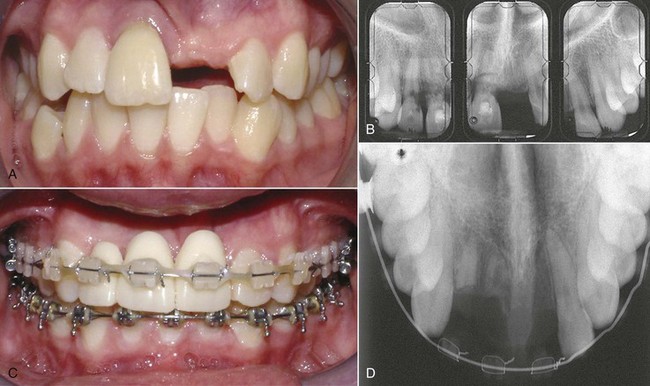
Traumatic Displacement of Teeth
Immediately following a traumatic injury, teeth that have not been irreparably damaged usually are repositioned with finger pressure to a near normal position and out of occlusal interference. They are then stabilized (with a light wire or nylon filament) for 7 to 10 days. At this point, the teeth usually exhibit physiologic mobility. If the alveolus has been fractured, then the teeth should be stabilized with a heavy wire for approximately 6 weeks. Following either of these initial treatments, if the teeth are not in ideal positions or have consolidated in a facial or lingual position that causes an esthetic problem or occlusal interference, orthodontic treatment to reposition them is indicated, and it can begin at that time, using light force. But even tipping forces can lead to loss of vitality and root resorption for previously traumatized teeth.9 This increased risk also applies to patients who have trauma (more extensive than crown fracture and especially luxation, intrusion, and extrusion injuries) during active orthodontic treatment.10 Prior to moving traumatized teeth, multiple radiographs at numerous vertical and horizontal angulations (or cone-beam CT [CBCT]) with a small field of view should be obtained to rule out vertical and horizontal root fractures that may make it impossible to save the tooth or teeth (Figure 12-4). During orthodontic treatment, it is reasonable to follow the teeth clinically by observing clinical mobility, sensitivity to percussion and cold, and electric pulp testing. The patients should report tooth discoloration, pain, swelling, and any discharge from the surrounding tissues. Radiographically, observation is sensible to determine periapical pathology at 2 to 3 weeks, 6 to 8 weeks, and 1 year. If the apex is complete at the time of the injury, it is more likely that the tooth will become nonvital from luxation injuries. If that happens, pulpal extirpation and treatment is recommended. External root resorption can jeopardize the tooth quite rapidly. Again, pulpal extirpation and treatment is recommended.
Vertical displacement of teeth presents an orthodontic treatment dilemma. If the patient is under 12 years old and if the apex is open, the best option in terms of pulpal necrosis, root resorption, and marginal bone healing is to allow the tooth to re-erupt.11,12 Re-eruption may take several months. In the meantime, the teeth should be monitored as described above. Any signs of nonvitality should be addressed with endodontic treatment. Even with severe intrusion, in the 12 to 17 years age group and with a closed apex, teeth that are allowed to re-erupt have better marginal bone healing, but nearly all of this group will have pulpal necrosis that requires endodontics.11 Based on this background, when the apex is open, it is best to allow re-eruption, regardless of the extent of the injury in a child. If the apex is closed and the intrusion is less than 6 mm, then re-eruption or orthodontic treatment (Figure 12-5) is probably indicated. Intrusions beyond this amount are best addressed by surgery due to the time involved. The goal is to preserve pulpal vitality, but with intruded teeth and the poor pulpal prognosis, repositioning is critical to improve access for endodontics and complete the diagnosis; crown and root fractures can remain undiagnosed even following extensive radiographs. Within 2 weeks of the injury, the intruded tooth should have been moved enough to allow endodontic access to reduce the possibility and extent of resorption. At that point, the tooth should be at or near its pretrauma position; if not, gingivectomy should be used to facilitate access.
When tooth movement during the course of routine orthodontic treatment is indicated for teeth that have had previous intrusion injuries, they are at increased risk for pulp nonvitality.13 Teeth that were extruded at the time of injury and not immediately reduced pose a difficult problem. These teeth have reduced bony support and a poor crown–root ratio. Attempts to intrude them result in bony defects between the teeth, and loss of pulp vitality is a real risk (especially for lateral incisors), so orthodontic intrusion is not a good plan.14 When the discrepancy is minor to moderate, reshaping the elongated tooth by crown reduction may be the best plan (Figure 12-6). This risk also applies to previously traumatized teeth with some obliteration of the pulp. The greater the obliteration, the greater the risk of loss of pulpal vitality during orthodontic treatment.15 An endodontically treated tooth that will need orthodontics can be successfully moved without much fear of resorption either before or after the final fill.16
Another consideration for patients with traumatically injured anterior teeth that cannot be restored is to retain the root of the compromised tooth until vertical growth is largely completed and an implant can be placed into the area.17 This adjunctive procedure reduces the chance of ridge resorption and the need for later bone grafting. If the tooth is compromised and can still be moved orthodontically, it can be repositioned and the root buried. Root burial entails decorination (removal of the clinical crown and root structure to below the soft tissue level) and closure of the soft tissue. The root can subsequently be removed or the implant placed through it (Figure 12-7).
Space-Related Problems
A major goal of early treatment is to prevent molars or incisors from drifting after premature loss of primary teeth, reducing the space available for unerupted teeth. Early treatment to align crowded incisors when space ultimately would be adequate or to create some additional space when a space deficiency exists may or may not be indicated. The decision as to whether this should be done in the mixed dentition and how it will be accomplished depends on the impact on esthetics as judged by the child and parents, as well as the location and magnitude of the problem. The goal should be to keep as many sensible options open as possible but to refrain from treatment when either the problem is too minor or later treatment obviously will be needed. Intervention for crossbites, habits, eruption problems, and simpler space problems has been described in Chapter 11. The section below focuses on more complex space problems that require more expertise in diagnosis, treatment planning, and biomechanics in order to achieve a useful and timely treatment. These treatments must be truly beneficial to the patient in the long run to be justified.
Excess Space
Generalized Spacing of Permanent Teeth
In the absence of incisor protrusion, excess space is not a frequent finding in the mixed dentition. It can result from either small teeth in normal-sized arches or normal-sized teeth in large arches. Unless the space presents an esthetic problem, it is reasonable to allow eruption of the remaining permanent teeth before closing the space with fixed appliances as part of comprehensive treatment (see Chapter 15). There is little or no advantage to early treatment unless it is for compelling esthetic reasons.18
A midline diastema often is a localized excess space problem (if not complicated by pathology, supernumerary teeth, or missing adjacent teeth). Tipping anterior teeth to close a small diastema was addressed in Chapter 11, but closing a large unesthetic diastema that may also be inhibiting eruption of adjacent teeth requires bodily repositioning of the central incisors to maintain proper inclinations of the teeth. Mesial crown and root movement provides more space for the eruption of the lateral incisors and canines. When the situation demands bodily mesiodistal movement and no retraction of the teeth, an anterior segmental archwire from central to central incisor or a segmental archwire including more anterior teeth is needed. Initial alignment of the incisors with a flexible wire is required. Then a stiffer archwire can be employed as the teeth slide together (with 22-slot brackets, 18 mil round or 16 × 22 mil rectangular steel are good choices; Figure 12-8). The force to move the incisors together can be provided by an elastomeric chain. Diastema closure is more predictable if only mesiodistal movement is required. If protruding incisors are part of the problem and need to be retracted to close the space, then careful attention to the posterior anchorage, overbite, and type of needed incisor tooth movement (tipping versus bodily retraction) is required (see below).
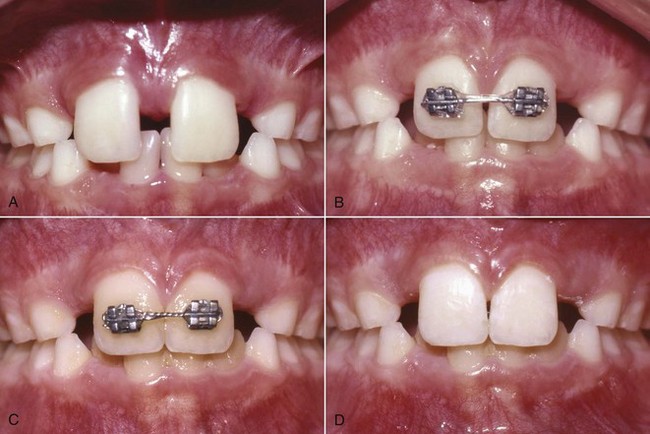
FIGURE 12-8 Closure of a diastema with a fixed appliance. A, This diastema requires closure by moving the crowns and roots of the central incisors. B, The bonded attachments and rectangular wire control the teeth in three planes of space while the elastomeric chain provides the force to slide the teeth along the wire. C, Immediately after space closure, the teeth are retained, preferably with (D) a fixed lingual retainer (see Figures 12-9 and 17-12), at least until the permanent canines erupt.
The experienced clinician’s desire to close diastemas at an early age is tempered by knowledge of how difficult it can be to keep the space closed as the other permanent teeth erupt. If the lateral incisors and canines have not erupted when the diastema is closed, a removable retainer will require constant modification. If the overbite is not prohibitively deep, a better alternative approach for retention is to bond a 17.5 mil multistrand archwire to the linguocervical portion of the incisors (Figure 12-9). This provides excellent retention with less maintenance.
Maxillary Dental Protrusion and Spacing
Treatment for maxillary dental protrusion during the early mixed dentition is indicated only when the maxillary incisors protrude with spaces between them and are esthetically objectionable or in danger of traumatic injury. When this occurs in a child who has no skeletal discrepancies, it is often a sequel to a prolonged finger-sucking habit. Eliminating the finger habit prior to tooth movement is necessary (see Chapter 11). The more common cause for maxillary incisor protrusion is a Class II malocclusion that often has a skeletal component, and, in that case, treatment must address the larger problem (see Chapter 13).
If there is adequate vertical clearance (not a deep bite) and space within the arch, maxillary incisors that are proclined or have been tipped facially by a sucking habit can be tipped lingually with a removable appliance as described in Chapter 11. When the teeth require bodily movement or correction of rotations, a fixed appliance is required (Figure 12-10). In these cases, an archwire should be used with bands on posterior teeth and bonded brackets on anterior teeth. This appliance must provide a retracting and space-closing force, which can be obtained from closing loops incorporated into the archwire or from a section of elastomeric chain. To ensure bodily movement, a rectangular archwire must be used so that the crown and root movement are controlled (as described in Chapter 9), and undue tipping does not occur and leave the patient with upright or “rabbited” teeth. Bodily incisor retraction places a large strain on the posterior teeth, which tends to pull them forward. Depending on the amount of incisor retraction and space closure, a headgear, chosen with consideration for vertical facial and dental characteristics, may be necessary for supplemental anchorage support.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses