12
A Systematic Approach to the Orthodontic Treatment of Periodontally Involved Anterior Teeth
Single tooth gingival recession
Etiology and prevalence
Amount of keratinized gingiva
Gingival recession and proclination of lower incisors
Clinical guidelines
Progressive spacing of incisors
Etiology, prevalence and differential diagnosis
Management
Case reports
Case 1
Case 2
Case 3
Management of periodontally involved teeth
Preliminary considerations
Esthetic considerations
Clinical examination
Management
References
Single Tooth Gingival Recession
This section focuses on isolated labial gingival recession in relation to the anterior teeth, either present or likely to occur, in patients who are going to receive orthodontic treatment. It does not cover the hard toothbrushing-related recession, which is primarily seen in canines, or multiple tooth recession affecting individual patients with thin-type gingiva.
Etiology and Prevalence
A tooth has gingival recession when its gingival margin is located apical to the cementoenamel junction (CEJ). There is scant information about the prevalence of solitary gingival recession in children and adults. After examining the lower incisor region in 15-year-old children, Stoner and Mazdyasna (1980) reported a prevalence of 17% for pseudo-gingival recession, that is, a longer clinical crown without root exposure, and 1% for gingival recession. Ainamo et al. (1986), in a sample of 7-, 12- and 17-year-old children, found the prevalence of gingival recession to be 5%, 39% and 74%, respectively. Evaluating the periodontal status among American children older than 13 years, Brown et al. (1996) found that gingival recession and loss of attachment increased with age, although the extent or number of affected sites with advanced conditions was not large in any age group; these findings were in agreement with Gorman (1967), Löe et al. (1992) and Khocht et al. (1993). Gingival recession is present in populations with both good and poor dental hygiene, although in the former it affects the buccal surfaces more (Löe et al. 1992). The teeth most frequently affected by isolated gingival recession are the lower central incisors, followed, but to a much smaller extent, by the upper and lower canines.
It has been suggested but not proved that gingival recession follows alveolar bone dehiscence. Bone dehiscence is a common finding when examining human dry skulls (Elliot and Bowers 1963; Rupprecht et al. 2001) and is positively correlated with thin alveolar bone. One should bear in mind that before computed topography was introduced, there were no reliable indirect means (conventional radiographs) for measuring the thickness of the alveolar bone of the teeth. During the surgical treatment of 113 teeth with gingival recession Löst (1984) found that the average distance between the lowest point of recession and alveolar dehiscence was 2.8 mm, with considerable individual variation. With computed tomography, it has been demonstrated that the thickness of both the labial and lingual plates of the alveolar bone of the lower incisors decreases when these teeth are orthodontically retracted, developing in some instances bony dehiscences that do not cause gingival recession (Sarikaya et al. 2002). This study only lasted 3 months so the formation of new alveolar bone afterwards cannot be ruled out. Nonetheless, it showed that dehiscence does not always lead to gingival recession.
Various factors have been implicated in the development of gingival recession: plaque-induced inflammation, malalignment of teeth, toothbrushing, orthodontic movement, high muscle/frenal attachment, caries and subgingival restorations, and a combination of these factors (Snyder 1982; Khocht et al. 1993). With regard to single tooth recession, especially in labially displaced lower central incisors or in canines blocked out of the arch, the insufficient amount of hard and/or soft tissue covering the labial side of these teeth seems to be the major factor in the presence or the potential for developing gingival recession with or without orthodontics.
Amount of Keratinized Gingiva
A number of studies aimed to determine the minimal amount of keratinized gingiva necessary to prevent gingival recession. There is a general agreement that teeth with minimal or no keratinized gingiva will not necessarily be associated with gingival recession (Bowers 1963; Lang and Loe 1972; Kennedy et al. 1985; Wennström et al. 1987; Freedman et al. 1992, 1999). In healthy periodontal patients with no gingival recession who underwent orthodontic treatment, Coatoam et al. (1981) reported that teeth with less than 2 mm of keratinized gingiva were capable of tolerating the treatment.
In children, gingival recession around the lower central incisors may improve when gingival inflammation is reduced (Powell and McEniery 1982) and self-correction of labially displaced incisors has occurred (Andlin-Sobocki et al. 1991; Andlin-Sobocki and Persson 1994). The more prominent a lower incisor is in the arch, the less keratinized gingiva it will have (Bowers 1963; Rose and App 1973), and when a labially proclined incisor is moved lingually, the width of its keratinized gingiva increases (Dorfman 1978; Nygan et al. 1991). The thickness of the labial marginal soft tissue appears to be more relevant than the width when considering its resistance to the proclination of the teeth, especially in the presence of plaque-induced inflammation of the gingiva (Steiner et al. 1981; Wennström et al. 1993).
Gingival Recession and Proclination of Lower Incisors
In contemporary orthodontics, crowding of the lower incisors is largely resolved through the expansion of the dental arch and the proclination of the incisors, and more seldom by extraction of one central incisor or two lower premolars.
Various studies have been performed in humans and animals to ascertain the influence of tooth position on gingival recession. It has been demonstrated that orthodontic proclination of the lower incisors in youngsters and adults does not cause gingival recession (Ruf et al. 1998; Artun and Grobety 2001; Djeu et al. 2002; Allais and Melsen 2003), but there are no data on long-term effects. Artun and Krogstad (1987), in a study of surgically treated patients with Class III malocclusions, reported a mild increase in the clinical crown height following proclination, greater than 10°, of the lower incisors. When reviewing animal studies, one should keep in mind that:
- The experiments were carried out in healthy animals, mainly monkeys and dogs
- Maxillary instead of the mandibular incisors were used in some instances (Karring et al. 1982; Wennström et al. 1987)
- Mechanotherapy and appliance design varied among the studies and differed from those used in regular human orthodontics.
a. In sum, proclination of the lower incisors in animals may result in
i. minimal increase of crown length
ii. bone dehiscence
iii. no loss of connective tissue attachment or only in a few teeth when the measurements were done on histological sections analyzed in the microscope, or when the assessment was done clinically following an elevation of a mucoperiosteal flap
b. Moreover, if the tooth was moved back to the original position the bone loss – dehiscence – was reverted, possibly owing to a healthy supracrestal soft tissue with the capacity to form bone after its resorption caused by traumatic forces (Batenhorst et al. 1974, Steiner et al. 1981, Engelking & Zachrisson 1982; Karring et al. 1982; Nyman et al. 1982; Wennström et al. 1987).
Based on the studies cited above it is likely that when lower incisors with a thin band of keratinized gingiva are proclined to resolve severe crowding, bone dehiscence, a thinning of the gingiva and an apical shift of the gingival margin may occur. This, in turn, may serve as a locus minoris resistentia to the development of gingival recession if bacterial plaque is present (Steiner et al. 1981; Wennstrom 1996).
Clinical Guidelines
When deciding to increase the band of keratinized gingiva around a tooth, it makes sense to distinguish between (1) lower and upper anterior teeth, (2) adults and children, (3) orthodontic and non-orthodontic patients, as well as (4) presence of, or potential for, gingival recession. In the presence of a minimal band of keratinized gingiva, if no orthodontic treatment is implemented, surgically increasing the width of the band of gingiva to improve the periodontal health is not indicated, regardless of age (Hangorsky and Bissada 1980; Wennstrom and Lindhe 1983; Persson and Lennartsson 1986). However, when adults with gingival recession affecting the upper anterior teeth and with a high smile line request treatment for esthetic reasons, surgical correction of the recession is indicated.
Periodontal plastic surgery for root covering or gingival augmentation is effective in reducing gingival recession but the proportion of partial and complete root coverage shows marked variability both between and within surgical techniques (Roccuzzo et al. 2002). In orthodontic patients with or the risk of gingival recession, free, epithelialized or connective, rather than pedicle, grafts are recommended, as the resulting gain in gingival thickness is larger. According to the few articles published on the subject, the type of gingival attachment that develops on the grafted site is, to a limited extent, the connective tissue type in the most apical and lateral parts of the recession and the epithelial type on the major portion of the covered root (Wennstrom and Pini Prato 2003). Free epithelialized gingival grafts should be reserved for the lower anterior teeth, where the color match is not an issue while the connective tissue type can be used in both arches. Coronal migration of the gingival margin of the graft, known as creeping effect, is sometimes observed during the maturation period in young patients who have received the free epithelialized graft long before the initiation of the orthodontic treatment.
It is worth emphasizing that with the use of superelastic archwires and self-ligating low-friction brackets, teeth can be moved orthodontically with truly light forces which are much more gentle on the periodontal support. This, in turn, may allow expansion and proclination of teeth without causing bone resorption (Handelman 1996) but with bone remodeling. Although there is no scientific evidence to support this claim, clinical experience indicates that larger dental movements can be implemented without risking the periodontal tissues.
In adults the most commonly affected teeth are the upper and lower canines which are partially or completely blocked out of the dental arch, and crowded and labially positioned lower central incisors. In adults with recession, a gingival graft is most times placed before the orthodontic treatment is initiated (Figs. 12.1 and 12.2).
Fig. 12.1 A 36-year-old woman with crowding of the lower incisors and gingival recession on tooth 31. A free epithelialized gingival graft was placed before non-extraction orthodontic treatment. (1–4) Tooth 31 before treatment after the gingival graft and during and after the orthodontic treatment. (5–6) Occlusal view before and after the treatment. (7–8) Frontal view before and after the treatment.
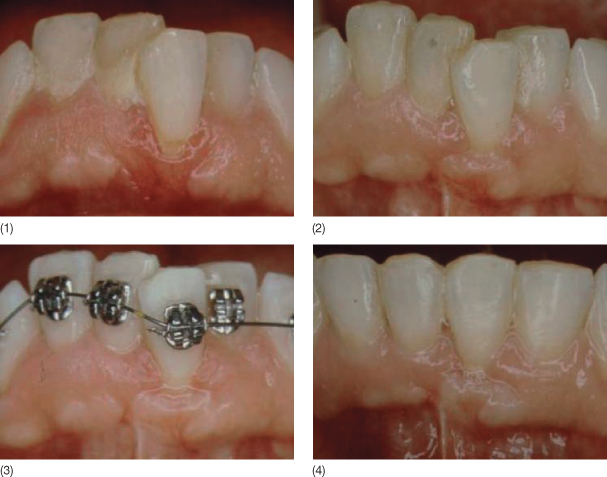
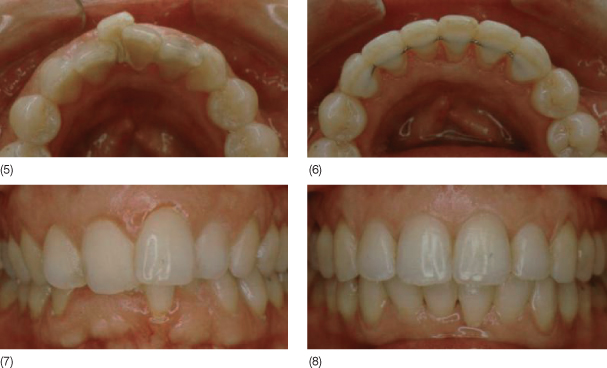
Fig. 12.2 A 37-year-old woman with a very narrow maxillary arch showing a blocked out maxillary left canine with severe gingival recession. Tooth 23 received a free subepithelial connective tissue graft before the orthodontic treatment. Before and after the interdisciplinary treatment: (1–4) upper front teeth, (5–6) frontal view, (7–8) oclusal view, and (9–10) smile.


When aligning a blocked-out lower central incisor with an appropriate band of keratinized gingiva by marked proclination of the tooth, a gingival graft may or may not be indicated to prevent thinning out of the gingiva and thereafter gingival recession during or long after the orthodontic treatment (Figs. 12.3 and 12.4).
Fig. 12.3 A 22-year-old woman with a concave facial profile and a blocked-out lower central incisor with an appropriate band of keratinized gingiva. The incisor received a free epithelialized gingival graft before non-extraction orthodontic treatment to increase the thickness of the gingival margin and thus prevent the risk of gingival recession after dental alignment. (1,2) Before, (3) during, and (4,5) after the orthodontic treatment. (6–9) Facial profile and cephalometric radiograph before and after the orthodontic treatment.
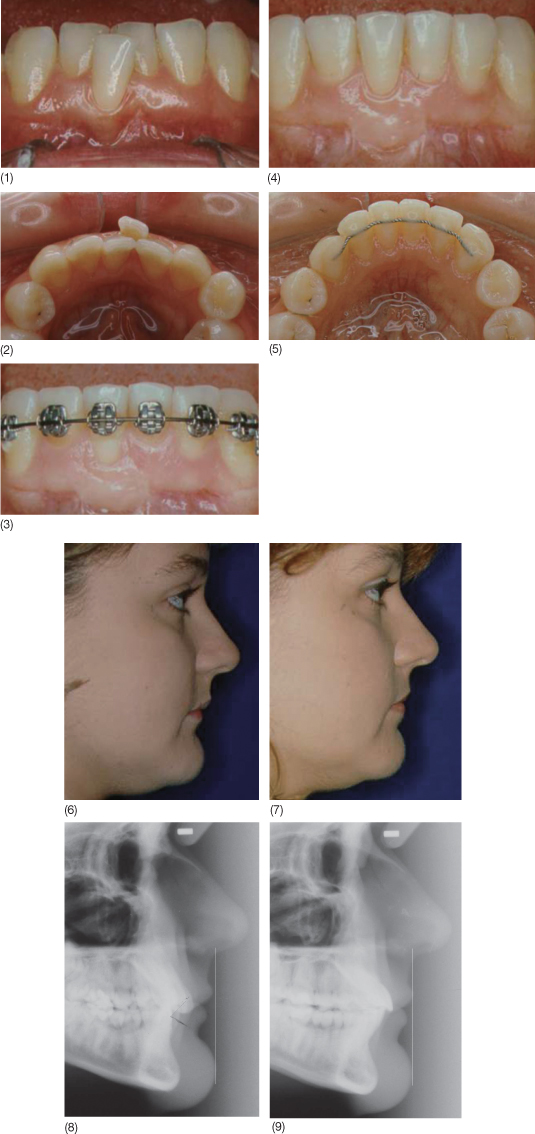
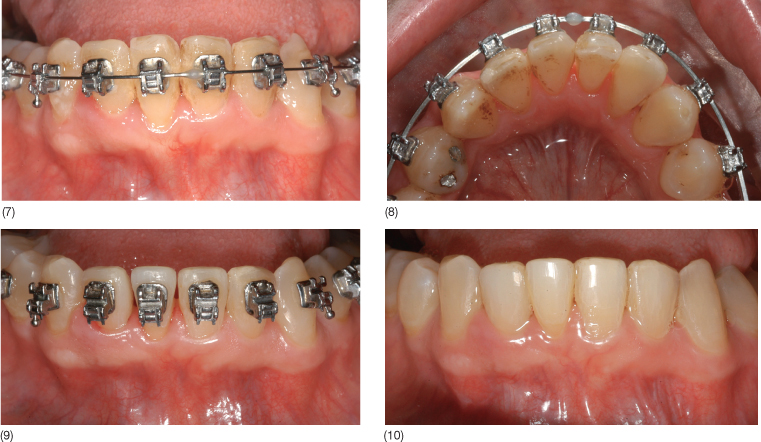
Fig. 12.4 A 42-year-old patient with crowding of the lower incisors and a narrow and thin band of keratinized gingiva in relation to 41. It was decided to check the soft tissue response to orthodontic treatment with expansion of the dental arch and proclination of the incisors. Non-extraction treatment, using low-friction self-ligating brackets and superelastic archwires, was initiated; no augmentation of the gingival band was needed. (1,2) Before treatment, (3,4) patient’s casts with bonded bracket, (5–6) at bonding appointment, (7, 8) 5 months into treatment, (9) after three-dimensional tooth remodeling of the lower anterior teeth, and (10) after the orthodontic treatment.
Progressive Spacing of Incisors
Etiology, Prevalence and Differential Diagnosis
In the periodontal literature, progressive spacing of the incisors is known as pathological tooth migration and defined as a change in tooth position resulting from disruption of the forces that maintain teeth in a normal position with reference to the skull (Chasens 1979).
Progressive spacing of incisors (PSI) is the most evident sign of the pathological change in the position of the teeth, in opposition to the ‘physiological’ dental crowding that usually occurs with aging; the affected teeth are the incisors, especially the upper ones; and spacing, at least initially, is progressive. However, some forms of spacing should not be termed as PSI although they increase with time. These are:
- Dentitions which have always had spacing, e.g. due to Bolton discrepancies, some dental Class III malocclusions, alteration of the function or form of the tongue (very seldom)
- Dentitions with missing anterior teeth where neighboring teeth may have migrated into the edentulous space created by extraction or agenesis
- Dentitions with gingival hyperplasia.
The causes of PSI have not yet been established but we know from Towfighi et al. (1997) and Martínez-Canut et al. (1997) that the prevalence of PSI in patients with moderate and severe periodontitis ranges from 30% to 56%, respectively. Moreover, the loss of more than three posterior teeth raises the odds of developing PSI (Martínez-Canut et al. 1997). It is likely that the periodontal bone loss could by itself explain the developing of PSI. Based on the equilibrium theory of tooth position the periodontium together with the cheeks and lips counteract the pressure exerted by the tongue at rest (Proffit 1978). When bone loss occurs the centre of resistance of the teeth changes and the tongue pressure on the incisors results in tooth migration leading to spacing.
The minor spacing in the anterior teeth that sometimes occurs in the acute periodontal phases and that partially or completely reverses after conventional or surgical periodontal treatment may be considered as an initial stage of PSI (Hirschfeld 1933; Manor et al. 1984; Brunsvold et al. 1997; Gaumet et al. 1999; Singh and Deshpande 2002). The evolution of bone loss with or without presence of deep overbite and/or tooth loss will determine whether the condition will progress to true PSI.
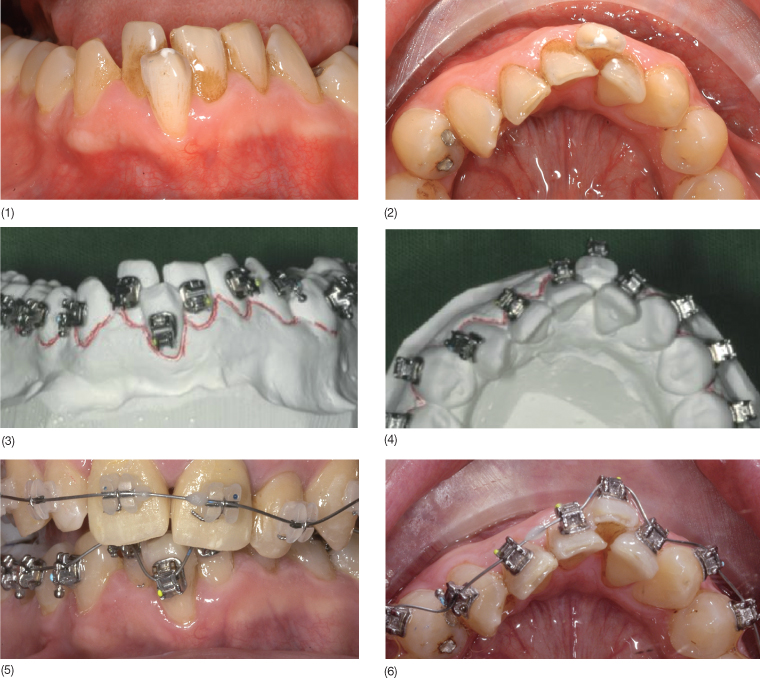
In summary, the term PSI should be restricted to those individuals with chronic periodontitis who, in any given time of their lives, develop spacing between the anterior teeth as a result of their proclination, with or without the presence of mutilated dentitions and/or deep overbites (Fig. 12.5).
Fig. 12.5 Evolution of PSI in a 35-year-old female patient with chronic periodontitis (1–4) and clinical situation at the initial orthodontic records (5–9).

Management
It should be emphasized that in patients with established PSI, periodontal treatment only will not close the interdental spaces or prevent its progression. Therefore, a combined interdisciplinary periodontal and orthodontic approach along with restorative prosthetic treatment if tooth loss is present is the appropriate way of managing these patients. The clinician should not underestimate the devastating effect that PSI has on the patient’s smile. Patients often seek a solution for their unsatisfactory smiles on their own and are therefore highly motivated to undergo interdisciplinary treatment which would include orthodontics (Fig. 12.6).
Fig. 12.6 (1–5) Handicapped smiles of patients with PSI and chronic periodontitis.

Closing spaces between anterior upper teeth with orthodontics is easy and predictable provided there is enough overjet between the upper and the lower incisors to retract the former. In the presence of a reduced vertical dimension with a deep overbite, the treatment of PSI is more challenging. In the patients, opening the bite will be the first treatment objective, which in turn will create an overjet into which the fanned out upper incisors can be retracted. There are various possibilities for opening the bite including: the use of a modified Hawley (see Box 12.1) with an anterior bite plane; uprighting the inclined posterior teeth; and placement of temporary prosthesis before the orthodontic treatment is initiated in patients with posterior mutilated dentitions. Three patients with PSI, deep bite of dental origin and insufficient overjet are presented below showing different ways of opening the bite. For the figures illustrating these cases, please visit the book’s companion website at www.wiley.com/go/melsen.
Box 12.1 Modified Hawley’s bite plane
- Description: A removable acrylic palatal plate supported by Adams’ claps or similar on the molars, with or without a labial bow, which carries an anterior bite plane immediately behind the upper incisors and canines onto which the lower anterior teeth, incisors and canines, have contact leaving at the same time the posterior teeth slightly out of contact. In order to avoid an overloading, the lower incisors should contact the bite plane.
- Effect: It temporarily opens the dental bite via passive eruption of the posterior lower teeth left out of contact which, in turn, as the mandible rotates clockwise, will develop or increase the overjet. The overjet so created will permit the closing of the spaced upper incisors without interference from the lower anterior teeth (Fig. 12.7).
- Usage: In the active part of the orthodontic treatment, Hawley’s bite plane is worn 24 hours per day except during the meals. In chronic periodontal patients, the bite opening required for the treatment of PSI is usually achieved in 3–4 months. The standard sequence consists of: (1) bite opening with Hawley’s bite plane, (2) bonding of the fixed appliances in the lower arch while maintaining Hawley’s bite plane until the lower teeth are aligned, (3) ceasing wear of Hawley’s bite plane with bonding of the fixed appliances in the upper arch to close the spaces and, (4) at end of orthodontic treatment, placement of fixed lingual retainers in both arches and a new Hawley’s bite plane for night use.
Case Reports
Case 1
A 47-year-old woman was referred by her general dentist for chronic periodontitis, PSI, impacted upper canines and mutilated dentition (see Box 12.2 for details). Bite opening was achieved with a combination of (1) prosthetic design, (2) proclination of the incisors and (3) reduction of the crown-to-root ratio. For the photographs for this case, visit www.wiley.com/go/melsen.
Box 12.2 Patient 1: diagnosis, treatment plan and sequence
Diagnosis: Brachyfacial (3)a · PSI (3) · Missing teeth 17, 27, 36, 37, 47 · Upper canines impacted in the palate · Angle Class I dental and skeletal · Retroclined upper and lower incisors (3) · Dental and skeletal deep bite (3/2) · Posterior bite collapse · Chronic periodontitis (3) · Primary and secondary occlusal trauma
Treatment plan: orthodontics, periodontics and prosthetics
- Objectives: pleasing smile + closing the interdental spaces of the anterior segment + opening the bite + coordination of the dental arches to allow the aesthetic prosthetic rehabilitation of the dentition
- Appliances: multibracket + elastics + modified provisional prosthesis
- Retention: indefinitely, with a fixed lingual arch in the lower anterior segment
- Possible limitations: degree of overbite and periodontal bone loss extension. Retention
- The upper incisors were orthodontically tested during a short period of time before any irreversible treatment was implemented
- Financial limitations: only certain aspects of dental treatment could be carried out
Sequence:
- Periodontal treatment and monitoring periodontal status throughout the orthodontic phase
- Orthodontics – start
- Implants: tooth 36
- Dental extractions: teeth 13 and 23, upper canines, and tooth 26b
- Modified provisional prosthesis in the upper posterior segments, markedly increasing the dental vertical dimension
- Orthodontics – end + retention
- Provisional prosthesis: from tooth 16 to 25
- Final prosthesis: Tooth-borne from tooth 16 to 25, in one piece; Implant-borne for tooth 36 and 26
a (1) mild, (2) moderate, (3) severe.
b Tooth 26 was extracted due to an endodontic accident.
- Prosthetic design: The bite opening was mainly achieved by increasing the height of the clinical crowns of the posterior teeth. Since full-arch prosthetic rehabilitation of the upper arch to replace both canines and stabilize the anterior segment was planned for the patient, the logical interdisciplinary treatment sequence was altered. Before the start of the orthodontic treatment, the patient received two vertically over-elongated provisional prosthesis in the posterior segments to establish a working vertical dimension to which the position of the upper and lower incisors was orthodontically adjusted.
- Proclination of the incisors: The overjet produced by the opening of the bite was utilized to procline the lower incisors, creating a new incisal relationship compatible with the new occlusal vertical dimens/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


