Restorative Materials—Ceramics
The term ceramic refers to any product made from a nonmetallic inorganic material usually processed by firing at a high temperature to achieve desirable properties. The more restrictive term porcelain refers to a specific compositional range of ceramic materials originally made by mixing kaolin (hydrated aluminosilicate), quartz (silica), and feldspars (potassium and sodium aluminosilicates), and firing at high temperature. Dental ceramics for metal-ceramic restorations belong to this compositional range and are commonly referred to as dental porcelains.
The laboratory portion of ceramic restorations is usually made in a commercial dental laboratory by skilled technicians working with specialized equipment to shape and tint the restoration to the specifications provided by the dentist. Skilled technicians and artisans are also employed by the manufacturers of artificial denture teeth to produce the many forms, types, and shades necessary in this application of porcelain. However, a variety of machinable ceramics are also available for chair-side fabrication of all-ceramic restorations by computer-aided design/computer-aided manufacturing (CAD/CAM). A discussion of CAD/CAM systems is presented in Chapter 14.
Classification of Dental Ceramics
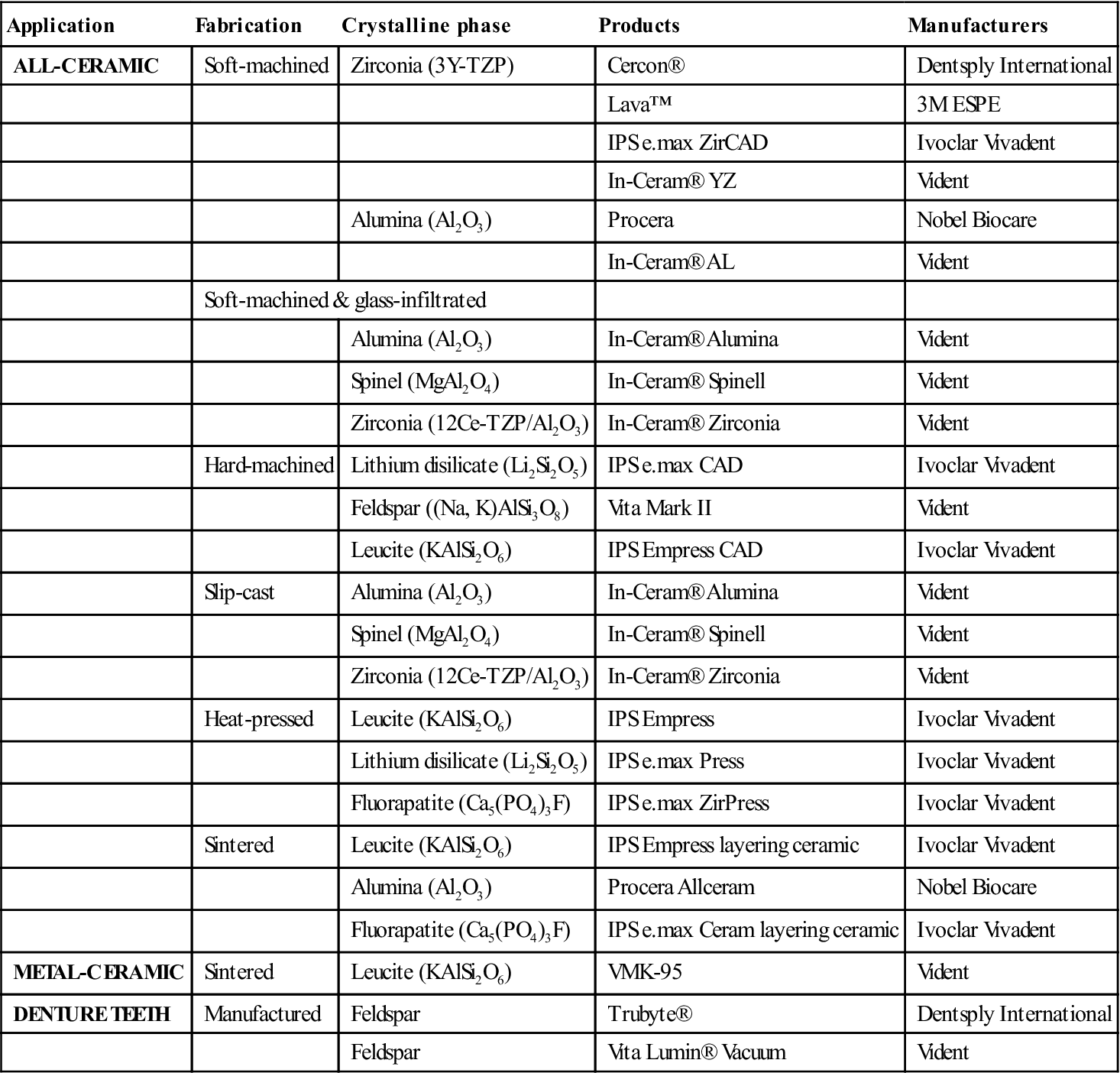
Dental ceramics can be classified according to their applications, fabrication method, or crystalline phase (Table 11-1).
TABLE 11.1
Classification of Dental Ceramic Materials with Examples of Products and Their Manufacturers
< ?comst?>
| Application | Fabrication | Crystalline phase | Products | Manufacturers |
| ALL-CERAMIC | Soft-machined | Zirconia (3Y-TZP) | Cercon® | Dentsply International |
| Lava™ | 3M ESPE | |||
| IPS e.max ZirCAD | Ivoclar Vivadent | |||
| In-Ceram® YZ | Vident | |||
| Alumina (Al2O3) | Procera | Nobel Biocare | ||
| In-Ceram® AL | Vident | |||
| Soft-machined & glass-infiltrated | ||||
| Alumina (Al2O3) | In-Ceram® Alumina | Vident | ||
| Spinel (MgAl2O4) | In-Ceram® Spinell | Vident | ||
| Zirconia (12Ce-TZP/Al2O3) | In-Ceram® Zirconia | Vident | ||
| Hard-machined | Lithium disilicate (Li2Si2O5) | IPS e.max CAD | Ivoclar Vivadent | |
| Feldspar ((Na, K)AlSi3O8) | Vita Mark II | Vident | ||
| Leucite (KAlSi2O6) | IPS Empress CAD | Ivoclar Vivadent | ||
| Slip-cast | Alumina (Al2O3) | In-Ceram® Alumina | Vident | |
| Spinel (MgAl2O4) | In-Ceram® Spinell | Vident | ||
| Zirconia (12Ce-TZP/Al2O3) | In-Ceram® Zirconia | Vident | ||
| Heat-pressed | Leucite (KAlSi2O6) | IPS Empress | Ivoclar Vivadent | |
| Lithium disilicate (Li2Si2O5) | IPS e.max Press | Ivoclar Vivadent | ||
| Fluorapatite (Ca5(PO4)3F) | IPS e.max ZirPress | Ivoclar Vivadent | ||
| Sintered | Leucite (KAlSi2O6) | IPS Empress layering ceramic | Ivoclar Vivadent | |
| Alumina (Al2O3) | Procera Allceram | Nobel Biocare | ||
| Fluorapatite (Ca5(PO4)3F) | IPS e.max Ceram layering ceramic | Ivoclar Vivadent | ||
| METAL-CERAMIC | Sintered | Leucite (KAlSi2O6) | VMK-95 | Vident |
| DENTURE TEETH | Manufactured | Feldspar | Trubyte® | Dentsply International |
| Feldspar | Vita Lumin® Vacuum | Vident | ||
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Classification by Application
Ceramics have two major applications in dentistry: (1) ceramics for metal-ceramic crowns (Figure 11-1, right) and fixed partial prostheses, (2) all-ceramic crowns (Figure 11-1, left), inlays, onlays, veneers, and fixed partial prostheses. Additionally, ceramic orthodontic brackets, dental implant abutments, and ceramic denture teeth are available.
Classification by Fabrication Method
The classification by fabrication method is summarized in Table 11-1, which also includes examples of commercial ceramics and their manufacturers. The most common fabrication technique for metal-ceramic restorations is called sintering. Sintering is the process of firing the compacted ceramic powder at high temperature to ensure optimal densification. This occurs by pore elimination and viscous flow when the firing temperature is reached. All-ceramic restorations can also be produced by sintering, but they encompass a wider range of processing techniques, including slip-casting, heat-pressing, and CAD/CAM machining. Some of these techniques, such as machining and heat-pressing, can also be combined to produce the final restoration.
Classification by Crystalline Phase
Regardless of their applications or fabrication technique, after firing, dental ceramics are composed of a glassy (or vitreous) phase and one or more crystalline phases, together with various amounts of porosity. Depending on the nature and amount of crystalline phase and porosity present, the mechanical and optical properties of dental ceramics vary widely. Increasing the amount of crystalline phase may lead to crystalline reinforcement and increase the resistance to crack propagation but also can decrease translucency. Materials for all-ceramic restorations have increased amounts of crystalline phase (between 35% for leucite-reinforced ceramics and up to 99% for polycrystalline zirconia ceramics such as 3Y-TZP) for better mechanical properties, but they are usually more opaque than dental porcelains for metal-ceramic restorations with low crystallinity. Table 11-1 lists the various combinations of fabrication techniques and crystalline phases found in dental ceramics.
General Applications of Ceramics in Prosthetic Dentistry
Ceramics remain the best material available for matching the esthetics of a complex human tooth. Their applications in dentistry are steadily expanding as new materials and manufacturing techniques are being introduced. They are used in single and multiunit metal-ceramic restorations. With all-ceramic systems, their applications include inlays, onlays, veneers, and crowns. The development of high-strength zirconia-based systems has made possible the fabrication of dental implant abutments and fixed partial prostheses. In addition, ceramics are still used to fabricate denture teeth. However, ceramics are generally brittle, weak in tension, and their performance is highly dependent on both their microstructure and the quality of the processing from the raw components to the final staining or glazing step.
Metal-Ceramic Crowns and Fixed Partial Prostheses
Ceramic is widely used as the veneering material in metal-ceramic crowns and fixed partial prostheses. This development was the result of successfully matching the coefficients of thermal expansion of porcelain with metal alloys and achieving a proper metal-ceramic bond. The finished glazed restoration is color-stable, tissue-friendly, biologically inert, and chemically durable. Metal-ceramic restorations are still widely used. However, while the survival rate of most all-ceramic crown systems compares favorably to that of metal-ceramic crowns for single restorations, the survival rate of multiunit all-ceramic fixed dental prostheses at 10 years is considerably lower. Meanwhile, survival rates at 5 years for zirconia-based all-ceramic systems appear promising.
All-Ceramic Crowns, Inlays, Onlays, and Veneers
Ceramics have been used to fabricate jacket crowns since the early 1900s. At that time feldspathic porcelain was used in the fabrication. Alumina-reinforced ceramics with improved mechanical properties were developed in the early 1960s. During the past 30 years, numerous novel materials and techniques for fabricating all-ceramic restorations have been introduced. As mentioned earlier in this chapter, they include heat-pressed, slip-cast, and machined all-ceramic materials. These new materials and techniques have widened the range of applications of ceramics, and in some cases made their processing easier.
Ceramic inlays and onlays are becoming increasingly popular as an alternative to posterior resin composites. They have better abrasion resistance than posterior composite resins and therefore are more durable. However, occlusal adjustments are more difficult and can lead to subsequent wear of the opposing tooth if not properly adjusted and polished. The marginal gap is clinically acceptable, yet greater than with gold inlays or onlays.
A ceramic esthetic veneer (laminate veneer) is a layer of ceramic bonded to the facial surface of a prepared tooth to cover an unsightly area. Ceramic veneers are custom made and are fabricated in a dental laboratory. Initially, ceramic veneers were made of feldspathic porcelain and sintered. Currently, most ceramic veneers are fabricated by heat-pressing or machining, using either a leucite-reinforced or lithium disilicate ceramic. To obtain sufficient adhesion, the tooth enamel is etched with phosphoric acid and the bonding surface of the ceramic is etched with 5% to 9% hydrofluoric acid gel and treated with a silane coupling agent. Resin composites specifically formulated for bonding to ceramic are used as the adhesive.
Mechanical and Thermal Properties of Dental Ceramics
Toughening Methods
Toughening methods for glasses and ceramics can be “built-in” or intrinsic to the material composition or crystalline phase. Crystalline reinforcement and transformation toughening are examples of built-in toughening mechanisms. Specific processing steps, such as tempering, chemical strengthening, or glaze application can also be involved to obtain strengthening.
The principle of toughening by crystalline reinforcement is to increase the resistance of the ceramic to crack propagation by introducing a dispersed crystalline phase with high toughness. Crystals can also act as crack deflectors when their coefficient of thermal expansion is greater than that of the surrounding glassy matrix, placing them under tangential compressive stresses after the ceramic has been cooled to room temperature.
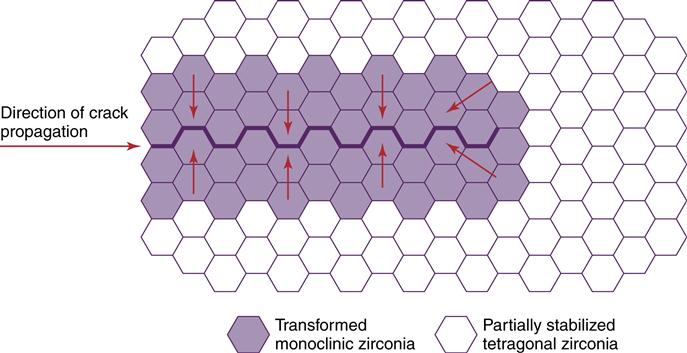
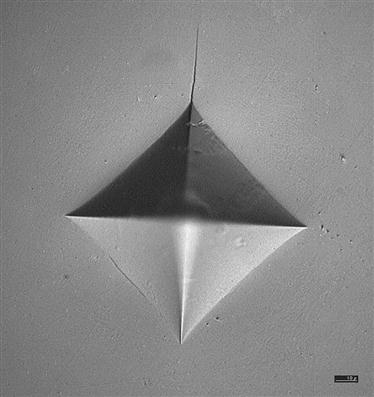
Transformation toughening is obtained, for example, in ceramics containing partially stabilized tetragonal zirconia. Zirconia (ZrO2) exists under several crystallographic forms. The monoclinic form is stable at all temperatures below 1170° C. The tetragonal form is stable between 1170° and up to 2370° C. The transformation from the tetragonal to the monoclinic form upon cooling is associated with a volume increase of the unit cell. This is the reason compacts of pure unalloyed zirconia cannot be obtained at room temperature; the compact would spontaneously crack upon cooling due to the transformation. The tetragonal form can be partially stabilized to room temperature by doping with various oxides, such as yttria oxide (Y2O3) or cerium oxide (CeO2). Zirconia-based dental ceramics produced by machining followed by sintering at high temperature contain tetragonal zirconia polycrystals, partially stabilized with 3 mole percent yttrium (3Y-TZP). This partial stabilization or metastability of the tetragonal phase allows the transformation from tetragonal to monoclinic to occur under external applied stresses. The transformation is also called stress-induced and is accompanied by a volume increase with associated compressive stresses in the vicinity of the crack tip, eventually leading to a closing of the crack in the transformed zone (Figure 11-2). Transformation toughening is responsible for the excellent mechanical properties of 3Y-TZP. Figure 11-3 shows a Vickers indentation in a 3Y-TZP dental ceramic under a 98.1-N load. Only one short crack can be seen emanating from one corner of the indentation.
Tempering and chemical strengthening are extrinsic strengthening techniques based on the creation of a compressive stress layer at the surface of a glass or a ceramic. Tempering is obtained by using rapid but controlled cooling rates whereas chemical strengthening relies on the replacement of small ions with larger ions by diffusion from a molten salt bath in which the ceramic or glass is immersed. Although widely used in the glass industry, neither of these two techniques is used for dental ceramics.
Glazing is the final step in the fabrication of metal-ceramic restorations. This standard technique, also called self-glazing, does not significantly improve the flexural strength of feldspathic dental porcelains. However, a low-expansion glass called glaze can also be applied at the surface of the ceramic, then fired to high temperature. Upon cooling, this glaze layer is placed under compression from the greater contraction of the underlying ceramic. This layer is also known to reduce depth and width of the surface flaws, thereby improving the overall resistance of the ceramic to crack propagation.
Test Methods
Numerous test methods are available to evaluate the mechanical properties of ceramics. Studies of the influence of test method on the failure stress of brittle dental materials have shown that important test parameters are the specimen thickness, contact zone at loading, homogeneity and porosity of the material, and loading rate. For this reason, discrepancies exist among the published values of mechanical properties for a given material. Manufacturers evaluate dental ceramics using a standard (ISO 6872) published and regularly revised by the International Organization for Standardization. Set protocols are proposed to evaluate radioactivity, flexural strength, linear coefficient of thermal expansion, glass transition temperature, and chemical solubility.
Sometimes, researchers use devices that try to simulate dental morphology. However, the experimental variables can become extremely complex and difficult to reproduce in this type of testing. Finite element analysis (FEA) constitutes another approach to the simulation of clinical conditions. Failure predictions of ceramic inlays by the FEA technique have successfully matched fractographic analyses of clinically failed restorations. Fractography is well established as a failure-analysis technique for glasses and ceramics. It has been recognized as a powerful analytical tool in dentistry. The in vivo failure stress of clinically failed all-ceramic crowns can be determined using fractography (see more discussion in Chapter 5.
Comparative Data
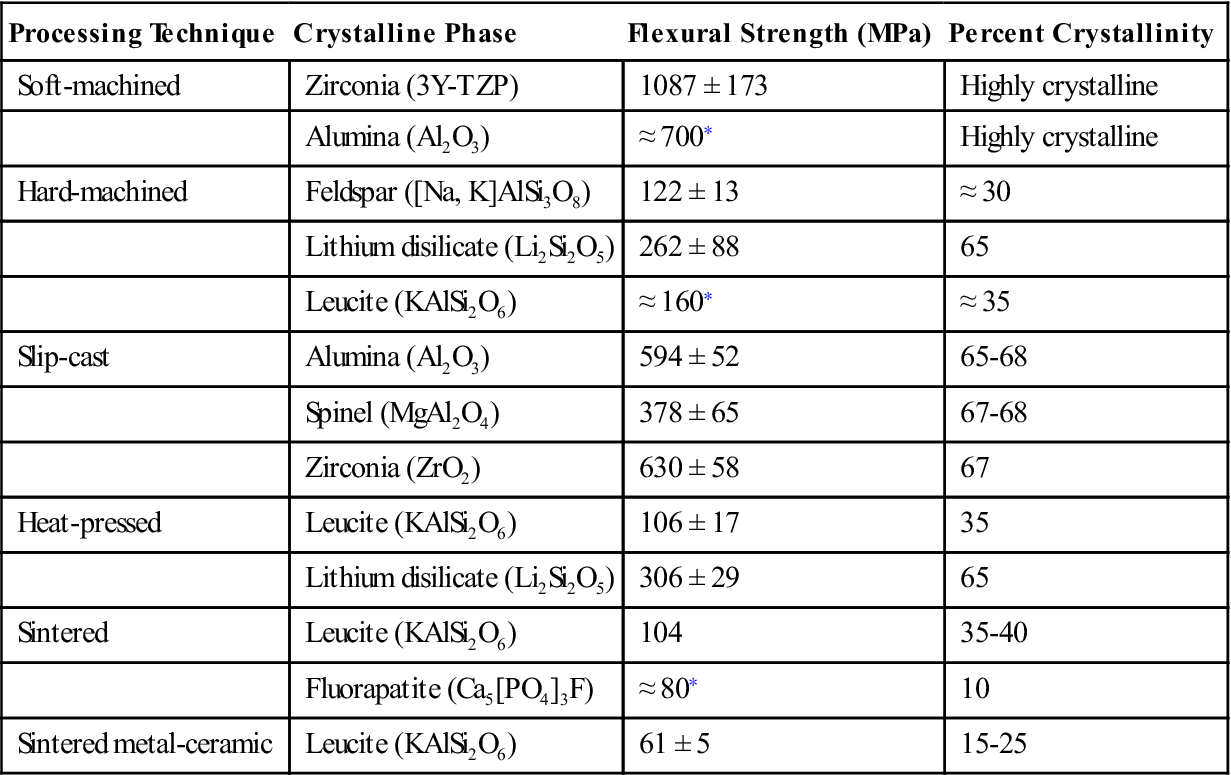
Flexural strength data for dental ceramics are summarized in Table 11-2. Feldspathic porcelains for metal-ceramic restorations have a mean flexural strength between 60 and 80 MPa. This value is lower than those listed for all-ceramic materials; however, because metal-ceramic restorations are supported by a metallic framework, their long-term probability of survival is usually higher.
TABLE 11.2
Flexural Strength of Selected Dental Ceramics
< ?comst?>
| Processing Technique | Crystalline Phase | Flexural Strength (MPa) | Percent Crystallinity |
| Soft-machined | Zirconia (3Y-TZP) | 1087 ± 173 | Highly crystalline |
| Alumina (Al2O3) | ≈ 700∗ | Highly crystalline | |
| Hard-machined | Feldspar ([Na, K]AlSi3O8) | 122 ± 13 | ≈ 30 |
| Lithium disilicate (Li2Si2O5) | 262 ± 88 | 65 | |
| Leucite (KAlSi2O6) | ≈ 160∗ | ≈ 35 | |
| Slip-cast | Alumina (Al2O3) | 594 ± 52 | 65-68 |
| Spinel (MgAl2O4) | 378 ± 65 | 67-68 | |
| Zirconia (ZrO2) | 630 ± 58 | 67 | |
| Heat-pressed | Leucite (KAlSi2O6) | 106 ± 17 | 35 |
| Lithium disilicate (Li2Si2O5) | 306 ± 29 | 65 | |
| Sintered | Leucite (KAlSi2O6) | 104 | 35-40 |
| Fluorapatite (Ca5[PO4]3F) | ≈ 80∗ | 10 | |
| Sintered metal-ceramic | Leucite (KAlSi2O6) | 61 ± 5 | 15-25 |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
< ?comst1?>< ?comen1?>∗< ?comst1?>< ?comen1?>Data from manufacturer.
Data from: Guazzato M, Albakry M, Ringer SP, et al: Dent. Mater. 20, 441-448, 2004; Guazzato M, Albakry M, Ringer SP, et al: Dent. Mater. 20, 449-456, 2004; Denry IL, Holloway JA, Tarr LA: J. Biomed. Mater. Res. (Appl. Biomater.), 48, 791-796, 1999; Della Bona A, Mecholsky Jr. JJ, Anusavice KJ: Dent. Mater. 20, 956-962, 2004; Höland W, Beall G: Glass-ceramic technology. The American Ceramic Society, Westerville, OH, 2002.
Among the currently available all-ceramic materials, zirconia (3Y-TZP) ceramics exhibit the highest values (800-1300 MPa), followed by slip-cast ceramics (378 to 630 MPa), and lithium disilicate–reinforced ceramics (262 to 306 MPa). The flexural strength of leucite-reinforced ceramics is around 100 MPa. As mentioned previously, the nature and amount of the crystalline phase present in the ceramic material strongly influences the mechanical properties of the final product. The shear strength of feldspathic porcelain is 110 MPa, and the diametral tensile strength is lower at 34 MPa. The compressive strength is about 172 MPa, and the Knoop hardness is 460 kg/mm2.
Fracture toughness is also an important property of ceramics; it measures the resistance to brittle fracture when a crack is present. The fracture toughness of conventional feldspathic porcelains is very similar to that of soda lime glass (0.78 MPa • m0.5). Leucite-reinforced ceramics exhibit slightly higher fracture toughness values (1.2 MPa • m0.5), followed by lithium disilicate–reinforced ceramics (3.0 MPa • m0.5). 3Y-TZP ceramics have the highest fracture toughness of all-ceramic materials (greater than 5.0 MPa • m0.5).
The elastic constants of dental ceramics are needed in the calculations of both flexural strength and fracture toughness. Poisson’s ratio lies between 0.21 and 0.26 for dental ceramics. The modulus of elasticity is about 70 GPa for feldspathic porcelain, 110 GPa for lithium disilicate heat-pressed ceramics, and 210 GPa for 3Y-TZP ceramics and reaches 350 GPa for alumina-based ceramics.
Shrinkage remains an issue for all-ceramic materials with the exception of machined ceramics from fully sintered ceramic blocks and heat-pressed ceramics. Shrinkage of the veneering ceramics applied on all-ceramic cores has to be carefully compensated for during porcelain buildup. The large shrinkage of machined zirconia restorations during the subsequent sintering at very high temperature (about 25%) is compensated for at the design-stage by computerized enlargement of the restorations.
The density of fully sintered feldspathic porcelain is around 2.45 g/cm3 and will vary with the porosity of the material. The density of ceramic materials also depends on the amount and nature of crystalline phase present. The theoretical density of 3Y-TZP dental ceramics is 6.08 g/cm3, assuming that the material is pore free. A density greater than 98.7% of the theoretical density is required for medical grade 3Y-TZP ceramics.
The thermal properties of feldspathic porcelain include a conductivity of 0.0030 cal/sec/cm2 (° C/cm), a diffusivity of 0.64 mm2/sec, and a linear coefficient of thermal expansion (CTE) of about 12.0 × 10−6/° C between 25° and 500° C. The CTE is about 10 × 10−6/° C for aluminous ceramics and lithium disilicate ceramics, 10.5 × 10−6/° C for zirconia-based ceramics (3Y-TZP), and 14 to 18 × 10−6/° C for leucite-reinforced ceramics.
Optical Properties of Dental Ceramics
Shade matching is a critical problem in replacing natural teeth. In addition, porcelain, being mostly amorphous in structure, cannot match the optical properties of crystalline enamel completely. As a result, ultraviolet (UV) and visible light rays are reflected and absorbed in different manners by the combination dentin/enamel, compared to porcelain, and restorations viewed from one incidence angle may not appear the same as they do when viewed from a different incidence angle. The cementing medium is an important factor in the final appearance of an all-ceramic restoration. Because of its opacity, an aluminous all-ceramic restoration may be cemented with a wide range of luting agents. However, more translucent all-ceramic restorations such as leucite-reinforced heat-pressed or machined inlays, crowns, or veneers, or a machined inlay or veneer, usually require the use of translucent resin luting agents that are available in different shades.
The shades of commercial premixed dental porcelain powders are in the yellow to yellow-red range. Because the range of shades of natural teeth is much greater than the range available in a kit of premixed porcelains, modifier porcelains are also supplied for adjustments. These modifiers are strongly pigmented porcelains usually supplied in blue, yellow, pink, orange, brown, and gray. The dental technician may add the modifier porcelain to the opaque and body porcelains during the building of the crown. Extrinsic surface staining, another way of changing the appearance of a ceramic crown, involves the application of highly pigmented glazes. The main disadvantages of surface staining are a lowered durability (a result of solubility) and the reduction of translucency.
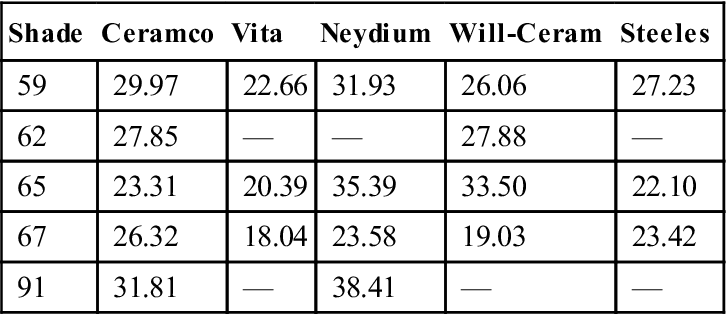
Translucency is another critical property of dental ceramics. The translucency of opaque, dentin (body), and enamel (incisal) porcelains differs considerably. Opaque porcelains have very low translucency, allowing them to mask metal substructure surfaces. Tin oxide (SnO2) and titanium oxide (TiO2) are important opacifying oxides for dental ceramics. Dentin porcelain translucency values range between 18% and 38%, as seen in Table 11-3. Enamel porcelains have the highest values of translucency, ranging between 45% and 50%. The translucency of materials for all-ceramic restorations varies with the nature of the reinforcing crystalline phase. Alumina- and some zirconia-based systems are opaque, whereas leucite-reinforced systems are more translucent. Recently, translucent zirconia systems have become available. The translucency of spinel-based systems is comparable to that of lithium disilicate–based systems and intermediate between alumina-based and leucite-reinforced systems. In order to mimic the optical properties of human enamel, opalescence is often desirable. Opalescence is a form of scattering and occurs when the crystal size is equal or smaller than the wavelength of light. In reflected light, the shorter blue-violet wavelengths are transmitted, whereas in transmitted light, the longer red-orange wavelengths are transmitted through the porcelain.
TABLE 11.3
Percent Light Transmission of 1-mm Thick Dentin Porcelains
< ?comst?>
| Shade | Ceramco | Vita | Neydium | Will-Ceram | Steeles |
| 59 | 29.97 | 22.66 | 31.93 | 26.06 | 27.23 |
| 62 | 27.85 | — | — | 27.88 | — |
| 65 | 23.31 | 20.39 | 35.39 | 33.50 | 22.10 |
| 67 | 26.32 | 18.04 | 23.58 | 19.03 | 23.42 |
| 91 | 31.81 | — | 38.41 | — | — |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Adapted from Brodbelt RHW, O’Brien WJ, Fan PL: J. Dent. Res. 59, 70, 1980.
Dental enamel also exhibits fluorescence. This characteristic is achieved in dental porcelains by adding rare earth oxides (such as cerium oxide). Because the outer layers of a ceramic crown are translucent, the apparent color is affected by reflectance from the inner opaque or core ceramic. For metal-ceramic restorations, shade mixing results from combining the light reflected from the inner, opaque porcelain surface and the light transmitted through the body porcelain. The thickness of the body porcelain layer determines the shade obtained with an opaque porcelain. This thickness effect may be minimized if the body porcelain and the opaque porcelain are the same color as that of some commercial systems.
All-Ceramic Restorations
Materials for all-ceramic restorations use a wide variety of crystalline phases as reinforcing agents and contain up to 99% by volume of crystalline phase. The nature, amount, and particle size distribution of the crystalline phase directly influence the mechanical and optical properties of the material. The match between the refractive indexes of the crystalline phase and glassy matrix is an important factor for controlling the translucency of the porcelain.
As mentioned earlier, several processing techniques are available for fabricating all-ceramic restorations: sintering, heat-pressing, slip-casting, and CAD/CAM. Figure 11-1, left, illustrates the cross section of an all-ceramic crown.
Sintered All-Ceramic Materials
Two main types of all-ceramic materials are available for the sintering technique: alumina-based ceramic and leucite-reinforced ceramic.
Alumina-Based Ceramic
The aluminous core ceramic used in the aluminous porcelain crown developed by McLean in 1965 is a typical example of strengthening by dispersion of a crystalline phase. Alumina has a high modulus of elasticity (350 GPa) and relatively high fracture toughness (3.5 to 4 MPa • m0.5), compared to feldspathic porcelains. Its dispersion in a glassy matrix of similar thermal expansion coefficient leads to a significant strengthening effect. It has been proposed that the excellent bond between the alumina and the glass phase is responsible for this increase in strength compared with leucite-containing ceramics. The first aluminous core porcelains contained 40% to 50% alumina by weight, dispersed in a low-fusing glassy matrix. The core was baked on a platinum foil and later veneered with matched-expansion porcelain. Aluminous core ceramic is now baked directly on a refractory die. Aluminous core porcelains have flexural strengths approximately twice that of feldspathic porcelains (139 to 145 MPa).
Densely sintered alumina-based ceramics can also be produced by dry pressing, followed by sintering. In order to compensate for sintering shrinkage (12% to 20% linear), an enlarged die is generated by computer-aided design. A high purity alumina-based ceramic is then fabricated by dry pressing and sintering at high temperature (1550° C). The final product is a highly crystalline ceramic with a mean grain size of about 4 μm and a flexural strength of about 600 MPa. The entire process has to be carefully controlled by the manufacturer. The last steps consist of veneering with translucent porcelain, staining, and glazing. The clinical performance of this ceramic in vivo at 15 years is considered excellent. The same technology is also available for zirconia-based core ceramics.
Leucite-Reinforced Ceramic
Leucite-reinforced ceramics containing up to 45% by volume tetragonal leucite are available for fabricating all-ceramic sintered restorations. Leucite acts as a reinforcing phase; the greater leucite content (compared with conventional feldspathic porcelain for metal-ceramic restorations) leads to higher flexural strength (104 MPa) and compressive strength. The large amount of leucite in the material also contributes to a high thermal contraction coefficient. In addition, the large mismatch in thermal contraction between leucite (20 to 25 × 10−6/° C) and the glassy matrix (8 × 10−6/° C) results in the development of tangential compressive stresses in the glass around the leucite crystals upon cooling, because the crystals contract more than the surrounding glassy matrix. These stresses can act as crack deflectors and contribute to increased resistance of the ceramic to crack propagation.
Sintered all-ceramic restorations are now being replaced by heat-pressed or machined all-ceramic restorations with better-controlled processing steps.
Heat-Pressed All-Ceramic Materials
Heat-pressing relies on the application of external pressure at high temperature to sinter and shape the ceramic. Heat-pressing is used in dentistry to produce all-ceramic crowns, inlays, onlays, veneers, and more recently, fixed partial prostheses. During heat-pressing, ceramic ingots are brought to high temperature in a phosphate-bonded investment mold produced by the lost wax technique. The heat-pressing temperature is chosen near the softening point of the ceramic. A pressure of 0.3 to 0.4 MPa is then applied through a refractory plunger. This allows filling of the mold with the softened ceramic. T/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses