11
Rescuing Teeth Impacted in Dentigerous Cysts
Dentigerous cysts
Radicular cysts
Treatment principles
The prognosis of teeth which have been severely displaced by cysts
Integrating spontaneous resolution into a combined treatment regimen
Eyelets and brackets
Cysts are found in a variety of tissues and in many sites in the human body. They are fluid-filled, epithelium-lined, balloon-like lesions, which generally enlarge progressively and painlessly due to hydrostatic pressure from within. If they are developing in a homogeneous medium, then the laws of physics determine that they will be spherical in shape. If the medium is bone, then this will resorb in response to pressure from within, thereby progressively permitting the enlargement. Simultaneously, there is a reactive bone apposition process on the outer side, which causes the bone to become expanded. This apposition is slower than the resorption from within, and so the bony expansion is accompanied by a thinning of the bony walls of the cyst, which may eventually become paper-thin. In the final instance, the cyst will resorb the last remnant of the hard tissue to become fluctuant beneath the skin or, in the context of this book, the oral mucosa.
Dentigerous Cysts
A dentigerous cyst is a specialized type of cyst insofar as it is located around the crown of an unerupted tooth and arises as an expansion of what is normally the very narrow space between the inner and outer enamel epithelia of the dental follicle, in which the completed crown of the tooth has developed. These two layers meet at the cemento-enamel junction (CEJ) at the neck of the developing tooth [1]. The cystic area enlarges due to the production of fluid by the epithelium, forcing the layers apart into its typical spherical shape, except where the crown of the tooth protrudes into the cyst, with its long axis traversing the centre of the lesion. In its early stages, therefore, it is difficult to distinguish a dentigerous cyst from a benign enlargement of the dental follicle, and between that and the normal follicle of the tooth. Furthermore, when eruptive movements of the tooth bring it through the bone and in close proximity with the oral mucosa the early dentigerous cyst may be fluctuant to palpation, is termed an eruption cyst and usually resolves spontaneously by rupture into the oral cavity. The tooth then erupts normally, its gingival attachment becomes normal and no subsequent signs of the earlier pathology remain.
However, when the cyst becomes larger, the pressure from within overcomes the tooth’s inherent eruptive force potential to stop its normal eruption, and it may even cause the tooth to ‘back up’ along its former eruption path, displacing it apically, while still remaining in the middle of the cyst (Figure 11.1). It seems, therefore, that the term ‘eruption cyst’ may represent a state of pressure equilibrium between the forces of eruption and the opposing force of intra-cystic pressure. With a smaller eruption cyst, the forces of eruption might prevail, as we have pointed out above. However, a larger eruption cyst may require surgical incision to bring about decompression, which will then permit the tooth to erupt spontaneously and quite quickly in the younger patient.
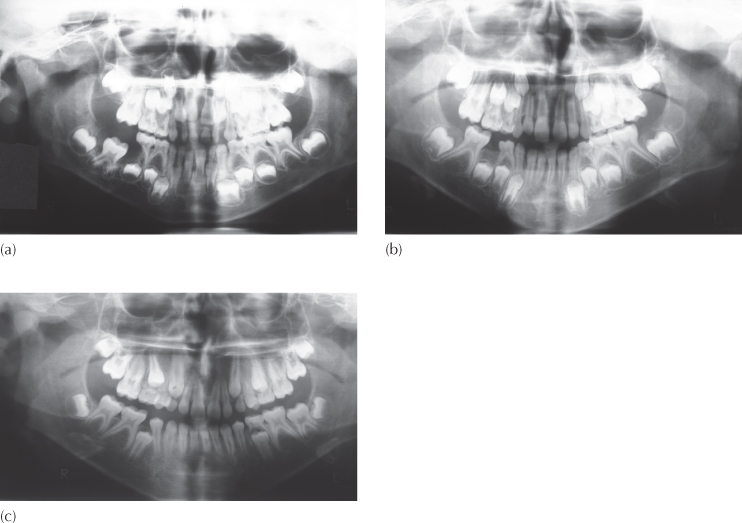
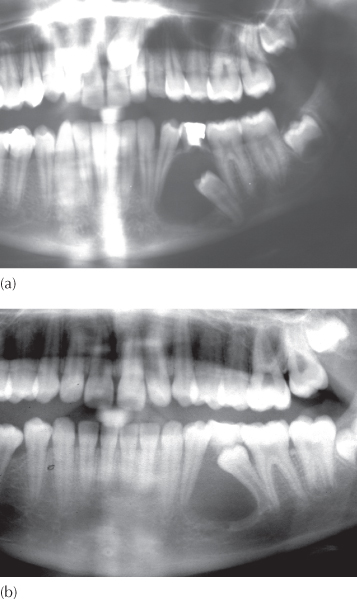
Fig. 11.1 A dentigerous cyst surrounds the crown of the mandibular right first molar has arrested eruption and has apparently slowed down root development. (b, c) The follow-up radiographs, taken two and five years later, show space closure having occurred from both the distal and the mesial, impacting the second premolar. The bizarre root morphology of the molar is the same on the affected and unaffected sides. Nevertheless, for what seemed a short root of questionable prospects for further growth in its initial position, growth has rebounded very impressively.
Regarding the affected tooth itself, its long axis is generally perpendicular to the epithelial outer wall of the cyst at its CEJ (Figure 11.2a). A good portion of the apical section of its root remains firmly in bone, but the pressure-generated enlargement of the cyst will cause its lining to circumferentially and progressively outline more and more of the otherwise bared coronal portion of the root, by a resorptive squeezing out of the crestal area of bone.
Fig. 11.2 A large cyst occupies much of the right side of the maxilla. (a) The anterior occlusal film shows the central incisor ‘backed up’ in line with its long axis. (b) The initial panoramic film shows the lateral incisor and both premolars laid out horizontally in the floor of the cyst. The canine has become displaced posteriorly into the molar region (arrow). The location and orientation of these teeth defines the perimeter of the cyst. Because the central incisor has been displaced superiorly and posteriorly, and is distant from the film, its image is beyond the focal trough of the film and hence has largely disappeared. (c) A Waters projection radiograph of the skull shows the degree of buccal displacement of the canine (arrow), indicating the lateral boundary of the cyst.
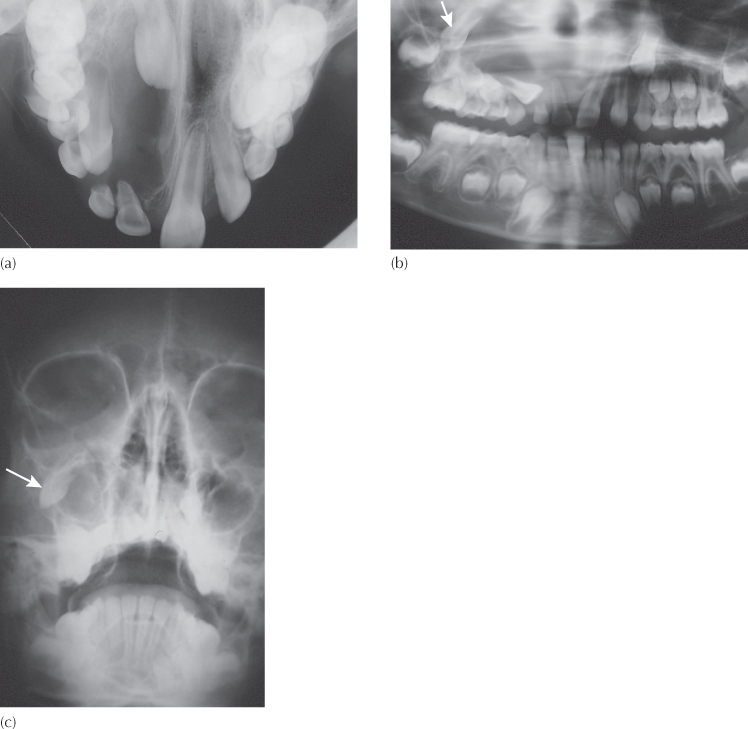
With further expansion, the lateral aspects of the cyst come up against adjacent unerupted teeth, which become pushed aside as their supporting bone becomes thinner and as the cyst lining comes into direct contact with their periodontal ligament (PDL). Each of these teeth then becomes profiled in the walls of the cyst, with only a thin epithelial lining to cover one side of the bared tooth along its full length (Figure 11.2b, c). The other side of the displaced adjacent tooth is invested by bone, with PDL intervening over the root area and its own dental follicle intervening in the crown area. The degree of displacement of these teeth will depend on the size of the cyst, but they lie in and are oriented parallel to the walls of the cyst, in contrast to the perpendicular orientation of the causal tooth.
Histologically, the cyst lining is squamous or stratified squamous epithelium and as such is similar to the follicle from which it originated. Thus, the only criterion for distinguishing between an enlarged follicular sac and a dentigerous cyst is size, as seen on a periapical radiograph. Accordingly, a workable definition for a dentigerous cyst is when the distance between the crown of the tooth and the dental sac is larger than 2.5–3 mm on the film. This is the definition most frequently used in radiology and surgery. However, we may like to refine this definition with more discerning biological criteria, which take into account the implications of the increased hydrostatic pressure within the lesion. Thus, should the eruptive progress of the affected tooth be halted or reversed, or should the radiolucent outline of the lesion appear to connect with the tooth some way down the root, apical to the CEJ, these might be considered more valid diagnostic signs.
The aetiology of a dentigerous cyst is strictly unknown, although it is associated with chronic local inflammation, as may be seen when the deciduous predecessor has become non-vital and an apical granuloma has initiated cystic change in the follicular sac of the unerupted permanent successor. An incomplete root canal treatment may leave the deciduous tooth symptomless, but the chronic periapical lesion may remain unresolved and this may act as the irritant that induces a cyst to develop from the follicle of the permanent successor (Figure 11.3). Unerupted permanent teeth, particularly maxillary canines, often exhibit enlarged follicles, and these may sometimes become further enlarged (Figure 11.4). This seems to occur frequently when there is a close association with the roots of the lateral incisors, although no specific explanation is forthcoming.
Fig. 11.3 (a) An incomplete root canal treatment has been performed in the mandibular left deciduous canine, as seen on this panoramic view. (b) A routine follow-up panoramic radiograph, taken prior to impending orthodontic treatment, reveals the development of a dentigerous cyst around, and displacement of, the permanent canine.
(Courtesy of Dr M. Barzel.)
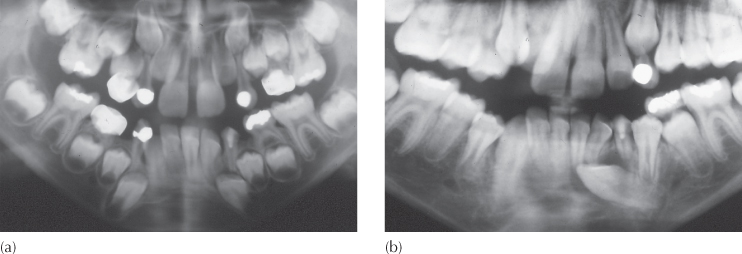
Fig. 11.4 The anterior portion of a panoramic view showing cystic enlargement of the follicles of the two maxillary permanent canines.
Radicular Cysts
After root formation of a tooth is completed, Hertwig’s root sheath disappears, leaving behind only the epithelial rests of Malassez in the immediate area. These remnants may sometimes be stimulated by the presence of a periapical granuloma to become cystic [2]. The radicular cyst is therefore to be found at the apex of a non-vital tooth, and it too may grow at the expense of the surrounding bone, to displace and partly envelop unerupted adjacent teeth, with the crowns and roots covered by the cyst epithelium. In this case, all the displaced teeth will be found in the walls of the cyst and oriented at a tangent to the cyst lining that covers them. No tooth will have its entire crown enveloped within the cyst, and the cyst lining will not be attached to the cervical area of any one of the teeth involved.
Histologically and clinically, the radicular cyst is similar to the dentigerous cyst and the clues to its identity are largely clinical (Figure 11.5). Accordingly, the following discussion of treatment and outcome will not differentiate between the two in any substantial manner.
Fig. 11.5 This figure shows two similar situations arising from different causes. (a) The crown and coronal part of the root of the second premolar are encompassed within the cyst and the orientation of the tooth is towards the middle of the cyst. The asymmetry may be due to the relative ease with which the first premolar root has been moved away from the lesion, while the more robust, two-rooted molar has withstood the cyst pressure. This is a dentigerous cyst. (b) The root of the erupted first premolar has been displaced mesially as with the above case, but the second premolar has been pushed distally against the molar and there has been distal root movement away from the cyst. There has been total stripping of bone support of the entire mesial side, while a thin wedge of bone can be seen between the molar and the affected premolar. This is a radicular cyst, presumably due to an incomplete root treatment on the second deciduous molar.
Treatment Principles
Surgery
Professional intervention may influence the future of the displaced tooth, depending on the type of treatment employed to resolve the cyst. The cyst may be opened and its lining completely shelled out in a procedure called enucleation [3]. The excised tissue is then sent for histological examination. Following the procedure, the crown of the tooth is left fully exposed within the cystic cavity and the tooth itself exhibits a high degree of mobility, due to its very rudimentary and reduced supporting periodontal attachment. A complete and hermetic closure of the surgical flap is usually attempted, sealing the former cyst cavity from the exterior to protect the exposed bone and soft tissue from infection. The aim is that this will fill with a blood clot and healing is by primary intention.
If the cyst is very large, then the chances of infection and breakdown of the clot become significant and, even in successful cases, the associated unerupted tooth becomes deeply buried in the newly forming bone, and it will need to erupt a considerable distance through this repairing bony tissue. In such circumstances, spontaneous eruptive movement of the tooth may be slight and a tooth grossly displaced by a large cyst may remain in an inaccessible position, following a filling-in of the surrounding tissues. Its extraction may then be unavoidable [4]. The prognosis for its eruption would appear to be in inverse proportion to its distance from the oral cavity. In the event that the blood clot breaks down due to infection and the area is left to heal by secondary intention, the entire former cystic area remains exposed to the exterior and will require some form of protective dressing or pack. In this situation, most of the teeth involved will need to be extracted, leaving a large defect of the basal bone in the final analysis, which may alter the shape and contour of the patient’s face. This will have marked functional, cosmetic and psychological consequences in the long term [4], with the need for artificial replacement of the missing teeth and, possibly, even a maxillofacial prosthesis to overcome the basal defect. Accordingly, enucleation is generally recommended for relatively small cysts.
For larger cysts, a two-stage procedure is often advised, in which the first stage is aimed at decompression and drainage of the cyst without removing its epithelial lining. Several months later, when the cyst has reduced in size, the lesion will be reopened and the remaining epithelium shelled out, in what has been termed the ‘curative enucleation of the cyst lining’ [4]. There can be little doubt that total removal is not always easy to achieve, since the exercise may threaten the unerupted teeth that are lodged in the walls of the cyst (Figure 11.6). These teeth have a very limited, rudimentary and tenuous periodontal attachment to the adjacent bone. Thus, the teeth themselves may be inadvertently plucked from their places and, conversely, some detached areas of epithelium may remain within the healing tissues, which may later regenerate.
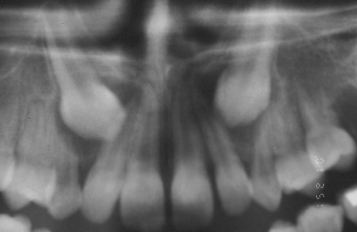
Fig. 11.6 (a) A radicular cyst, due to unresolved periapical pathology after root canal treatment of a second deciduous molar. The very rudimentarily developed second premolar has become severely displaced inferiorly in the lower border of the mandible. (b) The same view immediately after enucleation of the entire cyst lining. (c) The same view six months later, showing bony fill-in.
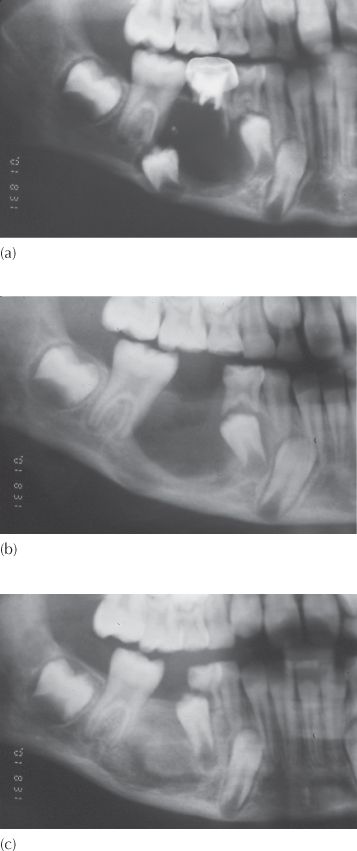
Figure 11.6a shows a portion of a panoramic view of the right side of the lower jaw of a 7-year-old patient, in which a large cyst is present. It seems likely that this is a radicular cyst related to the non-vital second deciduous molar, which has pushed aside the developing and largely rootless unerupted second premolar, whose long axis is parallel to the wall of the cyst. This patient was treated by extraction of the deciduous tooth, together with excision and complete enucleation of the cyst. In the accompanying transfer letter, the surgeon noted that he had found it necessary to remove the second premolar, and the second film (Figure 11.6b), taken postoperatively, shows the absence of this tooth.
From the surgeon’s perspective, three points are noteworthy in the management of this patient:
1. The very underdeveloped second premolar had a minimal attachment to its surroundings, as seen on the original film.
2. The cyst lining itself probably constituted a significant part of the attachment of this tooth.
3. During a surgical procedure of this type, visibility inside a cyst cavity is poor.
The surgeon may have judged that a tooth in this position, with this orientation, with an obvious absence of bony support and in the absence of a developed root had a poor prognosis and therefore removed it. Indeed, had the tooth remained in place, there is room to question whether it would have continued to develop a normal root and if it could ever have been expected to erupt into the mouth, either spontaneously or with orthodontic help. However, its root shows the very earliest stages of its development, is wide open and is vital, indicating potential for the genesis of a reasonable root, which will generally occur in time, as illustrated above (Figure 11.1).
One remaining possibility is that under these exceptional circumstances it is conceivable that this very early developing tooth, with its very tenuous attachment to its surroundings, had been dislodged inadvertently during the removal of the cyst lining!
It should be remembered that the lining of a dentigerous cyst arises from the inner and outer enamel epithelia of the tooth germ. In the long term and under normal circumstances, this epithelial tissue of the follicle eventually fuses with the epithelium of the oral mucosa, opens and everts to form the normal gingival attachment of the healthy tooth (see Chapter 6). During cyst formation the lining usually remains unaltered, and opening it to the oral environment, with a marsupialization procedure, will allow it to become contiguous with the oral mucosa. In time, a metaplasia of its epithelium will occur, as is the case with every normally erupting tooth, following which the former cyst lining will become histologically indistinguishable from the remainder of the oral mucosa.
Marsupialization is the surgical treatment option that is to be preferred for the larger lesions of this type [5–8]. This involves opening the cyst into the oral cavity at its most superficial point and maintaining the patency of this orifice over a long period of time.
The cut linings of the cyst and the oral mucosa fuse to become continuous with one another. The teeth involved directly or indirectly with the lesion are deliberately left undisturbed and remain covered by the thin epithelial continuum of the cyst lining.
In time, the lined cyst cavity becomes smaller and smaller as bony regeneration occurs behind the epithelium, to fill the defect in from the bottom up. As it does so, the causal tooth is generally carried bodily forward, as if on the crest of a wave, in the vanguard of the naturally occurring regeneration.
Understanding this natural process was, no doubt, the stimulus that caused periodontists to invent guided tissue regeneration in which bone will regenerate under an artificial membrane, by deliberately preventing the encroachment of epithelium.
Of much greater significance, the areas of root surface that had earlier become denuded by the enlarging cyst, with only the thinnest epithelial covering of cyst lining, now become infused with new bony support. Bone levels return to the more normal values seen in other unerupted teeth due to the osteogenesis that lifts the epithelial lining away from the root surface. In this way, teeth that previously appeared to be in hopeless situations may now take on a new lease of life, provided that orthodontic treatment may later be instituted to complete any final eruptive assistance they may need and then to align them. However, any attempt to apply orthodontic traction to teeth before complete resolution of the cyst and before the maximum amount of spontaneous eruption has occurred will extrude them ahead of the advancing bone, thereby weakening their bony and periodontal support and prejudicing their longevity.
Spontaneous resolution of the impaction may be expected to occur to a significant degree when the cyst is eliminated in this way, and several truly remarkable cases have been reported in the literature [5, 6]. From our experience in Jerusalem, these case reports are by no means exceptional and, with rational and careful management, have been repeated with a high degree of reliability in the most extreme cases that have come under our care [8].
It is therefore to be concluded that the cyst must be treated first and that monitoring of the healing process should be instituted until the bone has completed the reparative fill-in of the bony defect. Only at that point, which will be many months later, should an assessment be made of how much improvement has occurred naturally, how much more may be expected and how much orthodontic treatment is needed to improve the positions of the teeth. Not only, therefore, is there no value in bonding an attachment to the tooth at the time that the marsupialization is undertaken initially, but the procedure is likely to be quite harmful to the natural recuperation and positional improvement of the target teeth and for the health and integrity of the surrounding tissues – not least the cyst lining.
From the point of view of the oral and maxillofacial surgeon, treatment of this cyst is a priority in order to confirm the relatively innocent diagnosis. It must be remembered that, until a biopsy and pathological investigation are performed, the diagnosis is only tentative. The more s/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


