Pharmacology
General Considerations
Definitions
A Pharmacology—the study of drugs and their effects on living organisms
B Pharmacotherapy—the use of medications to treat different disease states
C Pharmacodynamics—the action of drugs on living organisms
D Pharmacokinetics—what the body does in response to the drugs (e.g., absorption, distribution, metabolism, excretion)
E Pharmacy—the practice of compounding, preparing, and dispensing drugs and of counseling clients about their medications
F Toxicology—the study of the harmful effects of drugs on living organisms
1. Drugs—biologically active substances that can modify cellular function; used in the prevention, diagnosis, treatment, and cure of disease or in the prevention of pregnancy
2. Nomenclature—each drug has several names
a. Chemical name—based on the drug’s chemical formula (e.g., N-acetyl para-amino phenol)
b. Trade (proprietary) name—each drug company makes up its own product trade name (e.g., Tylenol, Peridex, Atridox, Arestin)
c. Brand name—technically, the name of the drug company itself, but often used interchangeably with the trade name (e.g., either Astra [company that makes Xylocaine] or Xylocaine can be considered the brand name)
d. Generic name—official name of the drug determined by the U.S. Adopted Names Council that is used by all manufacturers of a particular drug (e.g., acetaminophen, chlorhexidine gluconate)
G Table 11-1 lists the Latin abbreviations used in prescription writing
TABLE 11-1
Common Latin Abbreviations Used in Prescription Writing
| Abbreviation | Interpretation |
| a., ante | Before |
| a.c., ante cibum | Before meals |
| A.D., auris dextra | Right ear |
| A.L., auris laeva | Left ear |
| b.i.d., bis in die | Twice per day or twice daily |
| gt., gutta | Drop (plural gtt.) |
| h., hora | Hour |
| h.s., hora somni | At bedtime |
| o.d., oculus dexter | Right eye |
| o.s., oculus sinister | Left eye |
| o.u., oculus uterque | Each eye |
| p.c., post cibum | After meals |
| p.o., per os | By mouth |
| p.r. | By rectum |
| p.r.n., pro re nata | As needed |
| q.d., quaque die | Once per day or once daily |
| q.i.d., quater in die | Four times per day |
| q.o.d. | Every other day |
| q.h. | Every 6 hours |
| sl. | Sublingual |
| supp. | Suppository |
| t.i.d., ter in die | Three times per day |
| u.d. | As directed |
References
1. Physicians’ Desk Reference (PDR)1—provides an index of drug manufacturers, brand and generic names of drugs, product categories, drug identification and information guide, and diagnostic information; updated yearly; most commonly used reference in the oral health care environment; inclusion of a drug in this reference is paid for by the manufacturer (seldom-used products not listed); information about the drug is similar to that found in the package insert, but this information is not updated regularly
2. Facts and Comparisons2—drugs organized by pharmacologic classes; complete listing; updated monthly; contains both prescription and over-the-counter (OTC) drugs; prepared by independent editors
3. Applied Pharmacology for the Dental Hygienist;3 Oral Pharmacology for the Dental Hygienist;4 Basic Principles of Pharmacology with Dental Hygiene Applications5—basic pharmacology textbooks for the dental hygienist; all three focus on dental hygiene considerations and provide the necessary information to avoid adverse reactions and drug interactions
4. Mosby’s Dental Drug Reference6—provides comments on a limited number of drugs specifically related to dentistry; includes dental drug interactions, oral side effects, and dental considerations
5. Drug Information Handbook for Dentistry7—provides an alphabetical listing of drugs and their effects on dental therapy; sections on managing medically compromised clients and treating specific oral conditions; information on dental office emergencies; comprehensive appendix on dental drug interactions and OTC dental products
6. Drug Information for the Health Care Professional, Volume 1, and Advice for the Patient, Volume 2;8 published yearly and updated quarterly by U.S. Pharmacopoeia; includes basic information regarding pharmacology, pharmacokinetics, adverse reactions, drug interactions, doses, and advice to the patient
B CD-ROM sources—more titles are becoming available; it is important to preview CD-ROMs before purchasing them because the ease of computer access (“user-friendliness”) varies considerably; many can be purchased with quarterly updates included
C Internet sites—extensive and growing volume of information; use a search engine to explore sites related to dental hygiene (see the table titled “Web Site Information and Resources” at the end of this chapter)
Agencies and Legislation
A U.S. Food and Drug Administration (FDA)—determines drugs to be marketed in the United States; after considering safety, efficacy, and physical and chemical data, the FDA requires quality control of manufacturing facilities, determines what drugs are sold by prescription, and regulates the advertising and labeling of prescription drugs
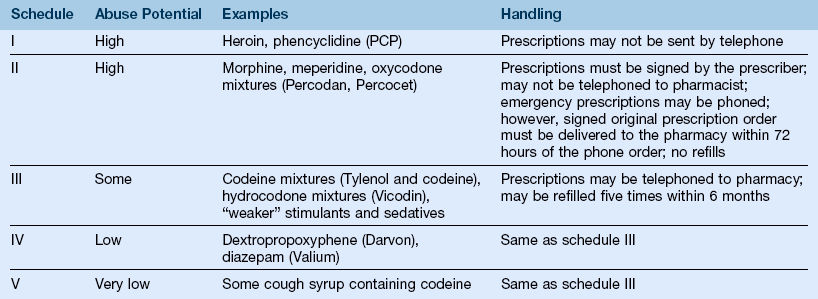
B U.S. Drug Enforcement Administration (DEA)—branch of the Department of Justice; determines the degree of control for substances with abuse potential; controlled substances used in dentistry are classified under Schedules I to V (Table 11-2)
Drug Action
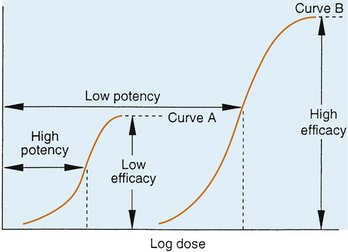
A Log dose–response curve—as the dose of a drug increases (x axis), the percentage of maximum response increases (y axis) until increasing the dose further produces no increase in the percentage of response (the effect of the drug reaches a plateau) (Figure 11-1)
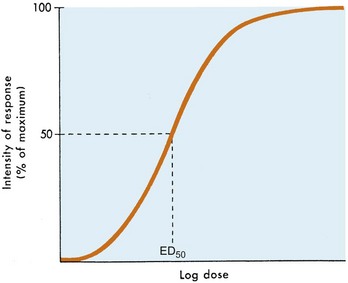
FIGURE 11-1 Log dose-effect curve. ED, effective dose.
1. Effective dose (ED) 50—dose that produces 50% of the maximum response, or the dose of a drug that produces a specific response in 50% of the subjects
2. Lethal dose (LD) 50—dose that is lethal to (kills) 50% of the subjects; laboratory animals are used to derive LD
3. Therapeutic index (TI)—LD50 divided by ED50; a measure of the safety of a drug
4. Onset—time required for a drug’s effect to begin; onset is short if the drug is given intravenously, longer if administered orally
5. Duration—length of time a drug’s effect lasts; related to a drug’s half-life
6. Half-life ( )—time required for a drug’s serum concentration to decrease by 50%; five half-lives are required for a drug to be eliminated from the body
)—time required for a drug’s serum concentration to decrease by 50%; five half-lives are required for a drug to be eliminated from the body
7. Potency—amount of drug (e.g., in milligrams) needed to produce an effect; the more potent an agent is, the lower is the dose needed to produce an effect (Figure 11-2)
8. Efficacy—the desired effect elicited by a drug, independent of dose (see Figure 11-2)
9. Tolerance—physiological response to the same dose produces less effect, or a higher dose is required to achieve the same effect
1. Oral (PO)—by mouth; easiest to use; good client acceptance; however, a latency period exists
2. Rectal—administration by suppository or enema; produces either local or systemic effect
3. Parenteral—a route other than an oral route; usually refers to an injection
4. Intravenous (IV)—administration into a vein; shortest onset of action and higher risk of adverse events compared to other routes of administration
5. Intramuscular (IM)—administration into the muscle; sometimes painful
6. Subcutaneous (SC, SQ)—injected beneath the skin (e.g., insulin)
7. Intradermal—injected into the dermis (e.g., skin test for tuberculosis produces a bleb [bump]; progesterone implants are administered intradermally)
8. Intrathecal—administered into the spinal fluid (e.g., to treat meningitis)
9. Intraperitoneal—injected into the peritoneal cavity (abdomen)
10. Oral or nasal—particles, volatile liquids, or gasses that are inhaled (e.g., nitrous oxide–oxygen (N2O O2) analgesia; as are some medications used to treat allergies and asthma)
O2) analgesia; as are some medications used to treat allergies and asthma)
11. Topical—ointments or creams applied to the skin or mucous membranes (e.g., hydrocortisone)
12. Sublingual—a tablet that dissolves or a solution that is sprayed under the tongue (for systemic effect)
2. Tablet—compressed or molded dosage form
3. Ointment or cream—semi-solid for topical application
4. Suppository—penile, rectal, or vaginal; systemic or local
5. Solution—single-phase system consisting of more than one constituent
6. Suspension—insoluble particles in liquid (e.g., milk of magnesia)
7. Emulsion—two immiscible (not mixable) liquids (e.g., oil and water)
8. Elixir—sweetened and hydroalcoholic (water and alcohol mixture)
1. Varies depending on the client’s:
a. Age—older adults may require lower doses because they may metabolize and excrete drugs more slowly
b. Weight—total body weight, muscle-to-fat ratio, and body size can affect drug absorption
c. Condition (disease)—many different disease states can affect drug absorption, metabolism, or excretion (e.g., congestive heart failure slows down metabolism; hyperthyroidism speeds up metabolism)
Adverse Reactions
Side Effect
A Side effect on a nontarget organ—effect on an organ other than that intended to be altered (e.g., insomnia resulting from a β2-agonist or theophylline); dose-related and often predictable
B Toxic reaction—predictable and dose-related effect on a target organ (e.g., insulin can lower blood glucose levels to the point of hypoglycemia)
C Allergic reaction—varies from mild rash to anaphylaxis; involves an antigen–antibody reaction (e.g., rash from penicillin); can include urticaria, soft tissue swelling, and difficulty breathing; not predictable and not dose related
D Idiosyncrasy—abnormal drug response that is genetically related
E Interference with natural defense mechanisms—body is less able to fight infection (e.g., steroids weaken the immune system)
F Teratogenic effect—adverse effect on a fetus (e.g., alcohol intake during pregnancy produces fetal alcohol syndrome)
G Safety—related to the therapeutic index; therapeutic index: LD50/ED50. The measure of a drug’s safety can be determined using this formula; the larger the number of this ratio, the safer is the drug
Pharmacokinetics
1. Degree of ionization—the more ionized (charged) the drug, the less it will be absorbed; conversely, the less ionized the drug, the more it will be absorbed; with weak acids or bases, this is a function of pH
2. Lipid solubility—the more lipid soluble the drug, the more readily it will be absorbed; the less lipid soluble it is, the less readily it will be absorbed
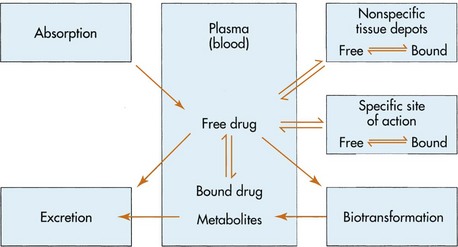
B Distribution of the drug (Figure 11-3)9
1. Drugs are transported to the site of action
2. Only the free, or unbound, drug can cross cell membranes (indicated by arrows between boxes in Figure 11-3)
3. In each cellular compartment, equilibrium is reached between the bound and unbound (free) drug
4. Redistribution—the drug moves from one tissue (where it exerts an effect) to another tissue (where it is inactive); this is one method of terminating a drug’s effect
5. Protein binding—drugs bind to protein receptors to varying degrees; once the drug binds to a protein receptor, it cannot exert its pharmacologic effect; when more than one drug is present in the system, the drugs may compete for the same receptor site; the drug with the stronger affinity will bind to the receptor site, and the drug with the weaker affinity will then exert its pharmacologic effect
6. Tissue binding—some drugs can also bind to body tissues and cause significant chemical effects (e.g., tetracycline has an impact on developing bones and teeth of the fetus and of a young child)
C Metabolism (biotransformation)—takes place mainly in the liver by hepatic microsomal enzymes; metabolites are more polar, less protein bound, and more easily excreted; drugs metabolized by microsomal enzymes can affect their own metabolism or that of other drugs (e.g., either increasing [as with barbiturates] or decreasing [as with cimetidine, erythromycin] the rate of metabolism); biotransformation is a source of drug interactions
D Excretion—usually by way of kidneys (urine); can also occur through feces (enterohepatic circulation), sweat, tears, or lungs (e.g., N2O is exhaled)
Receptors
An area in the body to which a drug binds
A Agonist—a drug that has an affinity for a receptor site and binds to it, producing an effect (e.g., opioid [narcotic] analgesic agent)
B Antagonist—a drug has an affinity for a receptor site and binds to it but produces no effect; competitively blocks the effect of an agonist (e.g., naloxone, an opioid [narcotic] antagonist blocks the effect of the agonist, an opioid)
Autonomic Nervous System Agents
Sympathetic (Adrenergic) Agents
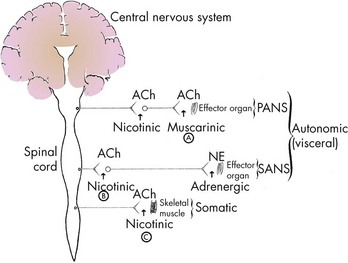
A Mimic the action of the sympathetic autonomic nervous system (SANS); act like norepinephrine (NE) in the SANS, producing stimulation of the SANS; epinephrine produces the same effect (Figure 11-4)
1. The SANS is activated by fear (the “fight-or-flight” response)
2. Catecholamine—chemical structure of some adrenergic agents
C Pharmacologic effects and adverse reactions
1. The central nervous system (CNS)—stimulation produces increased alertness; may also cause anxiety, anorexia
2. Stimulation of the heart—S+, produces
a. Positive chronotropic effect (increased HR)
b. Positive inotropic effect (increased strength of contraction of the heart)
c. Arrhythmias, with higher doses
d. α-Receptor stimulation—decreases HR because of the indirect (reflex vagal) effect
3. Vascular effects (on the arterial tree) result from
a. α-Receptors—causing vasoconstriction of blood vessels
b. β-Receptors—causing vasodilation of skeletal muscle blood vessels
c. Total peripheral resistance (TPR)—force against which the heart works to circulate blood
4. Mydriasis (pupil dilation) and reduced intraocular pressure; useful in treating glaucoma
5. Bronchodilation (by action of β2-agonist); useful in treating clients with asthma
6. Alterations in the blood glucose level; persons with diabetes mellitus must be observed for adverse reactions
D Drug interactions—examples of interactions caused by adrenergic agents are listed below:
1. Tricyclic antidepressants (e.g., amitriptyline [Elavil], imipramine [Tofranil])—interaction increases blood pressure; produces dysrhythmias
2. β-Blockers (e.g., propranolol [Inderal])—produce hypertension and bradycardia (slowed HR)
3. Antidiabetic agents (e.g., insulin, glipizide [Glucotrol], glyburide (DiaBeta)—increase the blood glucose level
4. Monoamine oxidase inhibitors (MAOIs)—no problem with epinephrine; indirect-acting amines (e.g., pseudoephedrine) must be avoided
5. General anesthetics—halogenated hydrocarbons (e.g., halothane [Fluothane]) sensitize the myocardium to catecholamines; epinephrine is a catecholamine; increase the chance of arrhythmia/dysrhythmias
E Dental hygiene considerations—the client’s pulse and blood pressure must be checked; all of these medications can increase heart rate and blood pressure
F Therapeutic uses (Table 11-3)
TABLE 11-3
Adrenergic Agents and Their Use
| Adrenergic Agent | Receptor Stimulated | Comments |
| Epinephrine (Adrenalin) | αβ | Endogenous catecholamine; local anesthetic additive |
| Methylphenidate (Ritalin) | α | Attention deficit hyperactivity disorder (ADHD) |
| Phenylephrine (Neo-Synephrine) | α | Nasal decongestant |
| Levonordefrin (Neo-Cobefrin) | α > β | Local anesthetic additive |
| Amphetamine | αβ | Diet pill (abused) |
| Pseudoephedrine (Sudafed) | αβ | Orally active nasal decongestant |
G Adrenergics as vasoconstrictors are contained in local anesthetic solutions
2. Advantages of adrenergic vasoconstriction
a. Prolongs duration of anesthesia
d. Reduces absorption (vasoconstriction)
e. Increases concentration of anesthetic at the nerve membrane
3. Disadvantages of adrenergic vasoconstriction
a. Excessive amount produces systemic toxicity
b. In persons with cardiovascular disease:
(1) Reasonable amounts can be used in local anesthetic additives for clients whose cardiovascular conditions are stable
(2) Avoid using epinephrine-impregnated retraction cords
(3) Maximum (safe) dose (MD) varies for normal and clients with cardiovascular disease
c. Hyperthyroidism—vasoconstrictors may produce a thyroid storm in clients who have not received treatment and in those receiving drug therapy; thyroid storm or thyroid crisis is characterized by an acceleration of all body processes (e.g., increases in heart rate, blood pressure, respiration, body temperature, and pulse); pulmonary edema and congestive heart failure can occur
α-Adrenergic Blockers (α-Blockers)
See the section on “Cardiovascular Agents” for a more detailed discussion.
β-Adrenergic Blocker (β-Blocker) Antagonists
See the section on “Cardiovascular Agents” for more information.
A Mechanism of action—drug blocks SANS action (β-receptors); some β-blockers are more selective for the β1-receptor than β2-receptor; some drugs are formulated to target β1-receptors, others to β2-receptors; other drugs target both β1 and β2 receptors
B Used to treat hypertension, angina, arrhythmias; also congestive heart failure, anxiety, and glaucoma; and used to prevent myocardial infarction (MI, heart attack)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses