11
Orthognathic Surgical Uses
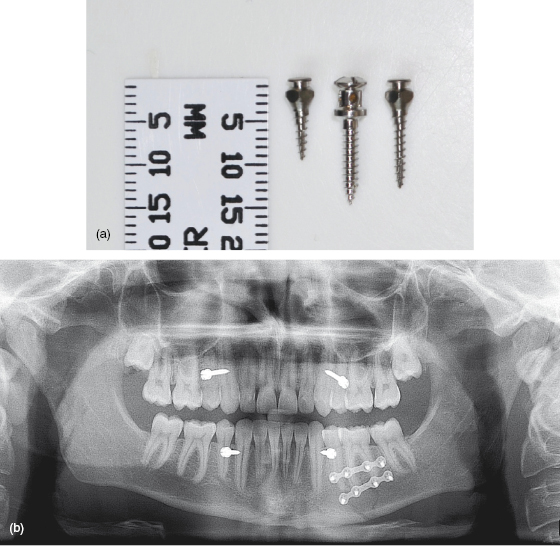
Orthodontic mini-implants provide a variety of novel applications for adult patients undergoing orthognathic surgical correction of their dentoskeletal deformity. For instance, some patients have traditionally been viewed as unsuitable for orthognathic treatment because their dental status is suboptimal (due to insufficient teeth or periodontal support). This contraindicates intra-operative intermaxillary fixation (IMF) and post-operative elastic traction, or even pre- and post-surgical fixed appliance phases. However, it is now feasible to effectively manage such patients during the peri-operative period using mini-implants, either as an alternative to fixed appliance surgical hooks, whereby heavy elastic traction on vulnerable teeth is avoided, or in lieu of an orthodontic (labial) appliance altogether. In particular, mini-implants’ relatively small body diameters and head sizes (Fig. 11.1a) mean that they pose less risk to dental roots and cause less trauma to the soft tissues, respectively, than conventional surgical intermaxillary (IMF) screws (Fig. 11.1b).1, 2, 3 Conventional pre- and post-surgical orthognathic treatment phases also benefit from the adjunctive use of mini-implants as described here.
Figure 11.1 (a) Photograph of 6 (left) and 9 (right) mm length IMT mini-implant versions with an IMF screw in the centre. (b) Panoramic radiograph showing close root proximity and poor mesio-distal orientation of IMF screws in a trauma case.
Clinical objectives
The range of orthognathic treatment problems which may be overcome by the adjunctive use of mini-implants includes patients with:
- An insufficient number of teeth or periodontal tissue support to tolerate intermaxillary forces.
- Teeth at risk of extrusion due to short roots (during the use of intermaxillary traction).
- Treatment with lingual appliances, requiring a means of fixation on the labial side.
- A contradiction between incisor decompensation (involving proclination) and space closure.
- Absence of the lower first or second molars such that the mandibular third molar should ideally be protracted and preserved, rather than sacrificed as part of the mandibular surgery plan.
- Facial asymmetry which is primarily transverse, but where pre-surgical levelling of an associated occlusal cant will optimise the transverse and antero-posterior surgical correction.
- An incomplete or unsatisfactory surgical outcome, where further surgery is contraindicated or declined.
Treatment options
- Conventional surgical hooks for fixation and traction from a (labial) fixed appliance.
- Surgical fixation using archbars.
- Surgical anchorage using IMF screws (Fig. 11.1).
- Bimaxillary surgery, for asymmetry cases, where the occlusal plane is levelled by the maxillary osteotomy.
- Orthodontic mini-implants for intra-operative fixation and post-operative traction.
Relevant clinical details
The stages during the orthognathic treatment pathway when mini-implants may be utilised are during the:
- Pre-surgical orthodontics.
- Orthognathic surgical episode, when IMF is required.
- Immediate post-operative phase, when intermaxillary traction is required.
- Post-surgical orthodontics.
- Long-term after surgical relapse has occurred.
The most relevant clinical details in determining mini-implant usage in this group of patients are the:
- Presence of an occlusal cant/vertical facial asymmetry.
- Periodontal status and root lengths of teeth since prolonged and/or heavy intermaxillary traction will have a deleterious effect on such teeth.
- Height of buccal/labial attached gingiva in areas where mini-implants are indicated.
- Root proximity of teeth adjacent to the planned insertion sites.
Biomechanical principles
- Ideally insert the mini-implants in sufficient numbers (typically five to six for full arch support), in both dentate and edentulous sites, where they will provide fixation points consistent with the planned lines of traction and occlusion.
- Elastics are less likely to be dislodged from a mini-implant which has been inserted in a horizontal direction (parallel to the occlusal plane) rather than at an oblique angle.
- Traction to ‘settle’ an unsatisfactory post-operative occlusion should be applied before maturation (solidification) of the osteotomy site callus.
Clinical tips and technicalities
- Remember that mini-implant insertion is a specific technique, which differs from that of both maxillofacial bone (screw) fixation and dental implantology. It is essential that whoever places the mini-implants must understand this fundamental issue, and pre-learn the relevant clinical instruments and steps. In particular, mini-implant insertion is a gentle technique using light forces, and one where the angles of insertion are carefully defined. These details can be critical since mini-implants typically remain in situ for months, relying on secondary stability, not just primary stability at the time of surgery. Surgical usage is further complicated by access problems since it can be surprisingly difficult to line up the correct path of insertion when the patient is supine and surgical drapes restrict lateral access. In such circumstances it is not unusual for fixation and surgical IMF screws to be inserted with their tips angled posteriorly. This can still be the case for posterior mini-implant insertions, as illustrated in Fig. 11.2 where mini-implants were inserted through the maxillary first molar furcations rather the adjacent interproximal spaces. All clinicians involved in surgical cases should be aware of this directional problem, and if in doubt then consider pre-surgical fabrication of a guidance stent.
- If the labial frenum is prominent then minimise patient discomfort, and soft tissue interference or overgrowth (over the mini-implant head), by either avoiding mini-implant insertion in the midline or performing a frenectomy.
- Horizontal angles of insertion (i.e. parallel to the occlusal plane) and full insertion of the mini-implants also help to minimise irritation of the lip/cheek soft tissues. Conversely, over-insertion makes it more likely that the intermaxillary wires/elastics may impinge on the adjacent gingival tissues.
- Consider pre-surgical root divergence to create interproximal space at the ideal mini-implant insertion sites. For example, limited fixed appliance alterations of the root alignment may be undertaken to facilitate mini-implant surgical usage. This may be particularly beneficial for sites such as the mandibular incisor region where the interproximal widths are typically narrow and the roots closely approximated.
- The anterior alveolar depth can be measured on a lateral cephalogram (Fig. 11.3). This will indicate whether the midline area provides sufficient depth for a long (e.g. 9 mm) body length mini-implant when it is inserted horizontally (parallel to the occlusal plane).
- Ideally use a mini-implant head with a rounded contour and low profile, e.g. the Infinitas IMT (Intermaxillary Traction) version with its mushroom-shaped head (Fig. 11.4). This ensures patient comfort when the mini-implants are inserted in relatively remote sites and are more likely to rub against the cheeks and lips (without a nearby fixed appliance to buffer the soft tissue contact). The generous undercut of the Infinitas IMT mini-implant head also helps the patient to place and retain elastics used for traction.
Figure 11.2 Panoramic radiograph showing mini-implants inserted in an orthognathic case, including two located in the maxillary first molar furcation areas.
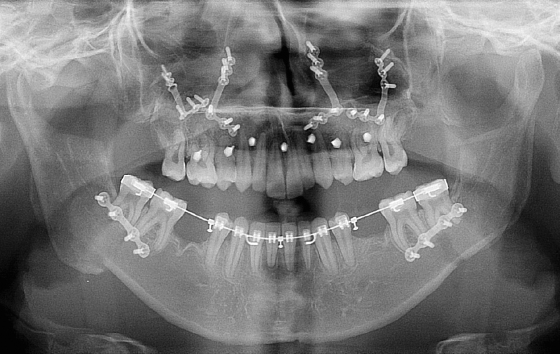
Figure 11.3 A lateral cephalogram showing the alveolar depth in the anterior maxillary and mandibular regions. The posteriorly directed angle of mini-implants inserted in theatre at the time of the osteotomy is also seen.
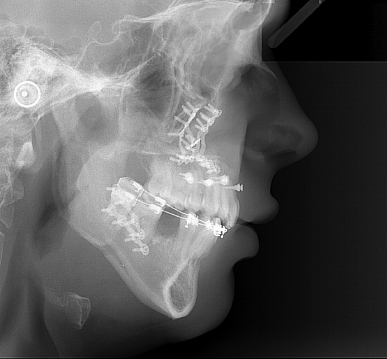
Figure 11.4 Close-up views of the IMT mini-implants showing their head’s large external undercut and mushroom-shaped top.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


