1
Mini-implant Principles and Potential Complications
The origins of orthodontic bone anchorage
Orthodontic-specific skeletal fixtures were developed from two distinct sources:
- restorative implants
- maxillofacial surgical plating kits.1
Orthodontic implants were first produced in the 1990s by modification of dental implant designs, making them shorter (e.g. 4–6 mm length) and wider (e.g. 3 mm diameter). However, they retained the crucial requirement for osseointegration, i.e. a direct structural and functional union of bone with the implant surface causing clinical anklyosis of the fixture. In contrast, mini-plates and mini-implants (mini-screws) are derived from bone fixation technology, and primarily rely on mechanical retention rather than osseointegration. In effect, modification of the maxillofacial bone plate design, adding a transmucosal neck and intra-oral head, resulted in the mini-plate; whilst adaption of the fixation screw design produced the mini-implant. Since the start of this millennium a wide variety of customised orthodontic mini-implants have been produced and these are now used in the vast majority of orthodontic bone anchorage applications. Orthodontic implants are no longer in standard use and the invasive nature of mini-plates appears to limit their use to orthopaedic traction (e.g. Class III) cases.
Using the right terminology
Unfortunately a misleading array of terms has been used for bone anchorage devices and their applications in both journals and the commercial literature. Essentially it is best to encompass all types of fixtures which provide skeletal anchorage under the umbrella terms: Bone Anchorage Devices (BADs) or Temporary Anchorage Devices (TADs), although the latter term does not indicate the essential role of bone in this anchorage. This book covers only one of the three types of BADs: mini-implants. Whilst the terms mini-implant and mini-screw are used interchangeably in the literature, it is erroneous to use the terms micro-screws or micro-implants since these fixtures are small (mini) and not microscopic. I prefer the term mini-implant since it conveys the small size and implantable nature of these temporary fixtures.
Second, there appears to be much misunderstanding over whether mini-implants osseointegrate. Most mini-implants are made from either titanium or titanium alloy and histological studies show variable levels of bone–implant contact (BIC).2,3 However, it is misleading to refer to this as osseointegration. Rather, clinical usage and percussion indicate that mini-implants are mechanically retained (like bone fixation screws) rather than forming a clinically discernible ankylotic union with the bone (which occurs with restorative implants secondary to the initial BIC phase). Hence, mini-implants can be immediately loaded and easily unscrew, usually without anaesthetic, at any time after insertion. This may be because of their relatively smooth surface and possibly because the surface contact is more a physical phenomenon than a biochemical one.
Principal design features
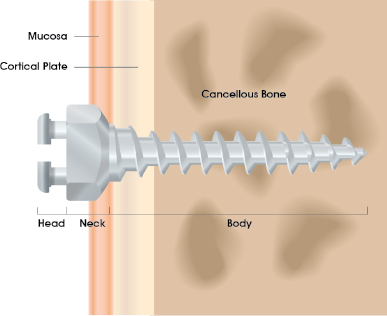
Most mini-implants have three constituent parts: the head, neck and body (Fig. 1.1), and are fabricated from a titanium alloy such as surgical grade five (Ti-6Al-4V). The head is the platform which connects to orthodontic appliances or elastic traction. The neck is the part that traverses the mucosa. The body is the endosseous section with threads around a core and a tapered tip. Mini-implants were initially available only in self-tapping (non-drilling) forms whereby a full depth pilot hole had to be drilled before mini-implant insertion. However, many self-drilling screws are now available. These have a tapered body shape with sharp tips and threads, and are inserted in a corkscrew-like manner. Full depth pre-drilling is avoided, although shallow perforation of the cortex is still advantageous where the cortex is thick or dense, e.g. the posterior mandible and palate.
Figure 1.1 Diagram showing the three principal sections of a mini-implant: the head superficial to the tissues, the neck traversing the mucosa, and the threaded body within the cortical and cancellous bone.
Clinical indications for mini-implants
Mini-implant usage may be broadly divided according to the case application and form of anchorage.
Routine cases
- Cases with high anchorage demands, e.g. retraction of prominent upper incisors or centreline correction (especially where unilateral anchorage only is required). Orthodontists new to mini-implant usage may find it easiest to introduce them into their clinical practice in such cases since the other aspects of the treatment are usually uncomplicated, enabling the orthodontist to readily recognise the anchorage effects and gain experience.
- Adults and older adolescents who wouldn’t comply well with other anchorage options, especially headgear.
- Where extrusive tooth movements would be unfavourable (risking an anterior openbite or vertical excess).
Complex cases
- Where conventional biomechanics would be limited, e.g. molar intrusion to correct an anterior openbite.
- Where conventional dental anchorage is limited by an inadequate number of anchor teeth (due to tooth loss or hypodontia) or periodontal support.
Direct and indirect anchorage
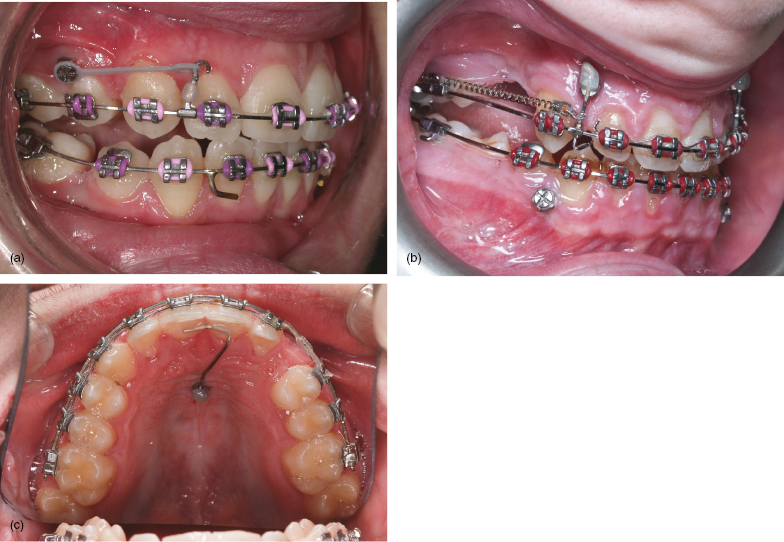
- Direct loading is when traction is applied from the mini-implant’s head to an appliance, typically with elastic chain or nickel titanium (NiTi) coil springs (Fig. 1.2a).
- Indirect loading involves using the mini-implant to reinforce anchor teeth, from which traction is applied (Figs 1.2b,c). Whilst indirect anchorage avoids some potential biomechanical side-effects (as discussed in Chapter Three) it risks insidious anchorage loss through flexing of the intermediary wire and undetected tipping or bodily translation of the mini-implant. Consequently, I prefer to use direct anchorage wherever possible and this will be elucidated in the clinical scenario chapters.
Figure 1.2 (a) Direct anchorage where this grey elastomeric attachment provides traction from the mini-implant head to a powerarm on the fixed appliance for en masse retraction of the anterior teeth. (b) The maxillary mini-implant provides indirect anchorage for molar protraction in this hypodontia case. Horizontal traction is applied, using a NiTi coil spring, connected to a vertical auxiliary wire, which in turn is joined to both the main archwire (using a cross-tube attachment) and the mini-implant head (where its position is secured by composite resin). (c) Indirect anchorage of the upper incisors during unilateral molar protraction, using an elastomeric chain on the fixed appliance. This involves a 0.019 × 0.025 stainless steel auxiliary wire from the mid-palatal mini-implant’s head to the central incisors’ palatal surfaces, secured to both with composite resin.
Potential mini-implant complications
A number of risks and side-effects have been observed with mini-implant clinical usage and in the research literature. Fortunately, these are reversible in most clinical situations, but it is important to consider them i/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


