CHAPTER 11 Mechanical and Chemotherapeutic Home Oral Hygiene
As the technological level of health care increases, it is important not to lose sight of the basics of patient care. In dentistry, this means establishing and maintaining effective preventive habits in our patients. No matter how sophisticated our dental techniques and procedures have become, preventive dentistry is the foundation on which all oral health care must be built. In 1960, McDonald discussed how pediatric medicine had changed in the previous 30 years (since 1930) from 90% treatment and 10% prevention to just the reverse.1 He stated that preventive measures for dentistry were available and remained to be applied, as they had been in pediatrics. With this preventive philosophy, dentistry, particularly dentistry for children, has come a long way toward reaching this ratio of 90% prevention to 10% treatment.
At the core of this preventive foundation is home oral hygiene and plaque control. The area of oral hygiene has undergone recent developments that have turned a mundane subject into a field of surprising growth and research. Modern biology has made new inroads in the area of plaque control and will continue to exert a strong influence on how we look at oral hygiene and plaque in the future. The traditional focus of oral hygiene has been and will continue to be the control of the two most prevalent oral diseases: caries and periodontal disease. Although plaque control is essential to oral hygiene, unlike with periodontal disease, no clear relationship exists between plaque control and the prevention of caries. As discussed in Chapter 10, the complex etiology of decay centers on the following factors: tooth susceptibility, bacterial plaque, refined carbohydrates, and time. Many other variables, such as oral sugar clearance, salivary flow, and pH and immune factors, add to the complexity of this process. This may help explain the difficulty in demonstrating a relationship between oral hygiene practices and caries prevention.
Despite this ambiguity, plaque control remains an essential element for oral health. Although Marsh has shown that the natural oral microflora confers several benefits on the host, in the absence of oral hygiene, dental plaque accumulates, which leads to shifts in bacterial populations away from those associated with health.2 Treatment should therefore be designed to control rather than to eliminate dental plaque.
MICROBIAL ASPECTS OF ORAL HYGIENE AND PLAQUE FORMATION
Although Miller proposed in the late nineteenth century that microorganisms play a role in dental disease,3 definitive evidence of the microbial etiology of dental caries and periodontal diseases did not appear until three fourths of a century later with the work of Keyes4 and of Löe and colleagues.5 Since these seminal studies were performed, the major focus of dental research has been to define the specific microorganisms in dental plaque that mediate these diseases. Although great progress has been made in identifying these pathogens, our primary tools in preventing dental diseases remain mechanical removal of plaque and promotion of the remineralization of the tooth surface. Therefore the following brief review of the timing, mechanisms, and biology of plaque formation provides a scientific rationale for any clinical program of oral hygiene and prevention.
The development of anaerobic culturing techniques and, more recently, genetic techniques that allow for the detection of uncultivable species have identified more than 700 bacterial species and numerous distinct bacterial habitats in the mouth. Interestingly, only a limited number of species are found in high numbers in dental plaque.6–8 These species are uniquely suited to this habitat. The formation of plaque on the tooth surface is characterized by progression from a limited number of pioneer species (mainly streptococci and other gram-positive organisms) to the complex flora of mature dental plaque. This maturation involves initial adherence of bacteria to the salivary pellicle and subsequent formation of a complex multispecies biofilm. Most oral bacteria have evolved specific adherence mechanisms that enable them to colonize the tooth surface. In addition, bacteria undergo a number of phenotypic changes as they initiate the formation of a biofilm. The molecular mechanisms that underlie these processes have been intensively studied. Kolenbrander and Kuramitsu have provided recent reviews of these areas.8–10 Although their reports offer the possibility of new methods of plaque control, mechanical plaque removal with supplementation by chemotherapeutic agents currently offers the most practical method of controlling plaque.
Not only do microbial changes occur as plaque matures on the tooth surface, but mature dental plaques associated with oral diseases appear to differ from those associated with oral health. Many studies have demonstrated that, in dental caries, the pathogenicity of plaque is related to the numbers of Streptococcus mutans and related species present.11 In contrast, the plaques associated with gingival inflammation are characterized by a predominance of gram-negative bacteria rather than the predominantly gram-positive flora found in oral health. This transition seems to coincide with inflammatory changes that occur at the gingival margin. Plaque control efforts should be directed toward two goals: (1) limiting the numbers of mutans streptococci in dental plaques for prevention of caries by mechanical elimination of supragingival plaque and limitation of dietary sucrose, and (2) maintaining the predominantly gram-positive flora associated with gingival health by mechanical removal of plaque from the subgingival area on a regular basis. The use of chemotherapeutic agents, particularly chlorhexidine, can also play a role in maintenance of gingival health. The incorporation of these methods into the daily routines of patients and their parents is perhaps the greatest challenge facing the dentist.
MECHANICAL METHODS OF PLAQUE CONTROL
MANUAL TOOTHBRUSH
The toothbrush is the most common method for removing plaque from the oral cavity. A number of variables enter into the design and fabrication of toothbrushes. These include the bristle material; length, diameter, and total number of fibers; length of brush head; trim design of brush head; number and arrangement of bristle tufts; angulation of brush head to handle; and handle design. In addition, many features, such as the use of neon colors or familiar cartoon caricatures, are designed to attract the attention of potential purchasers (Fig. 11-1).
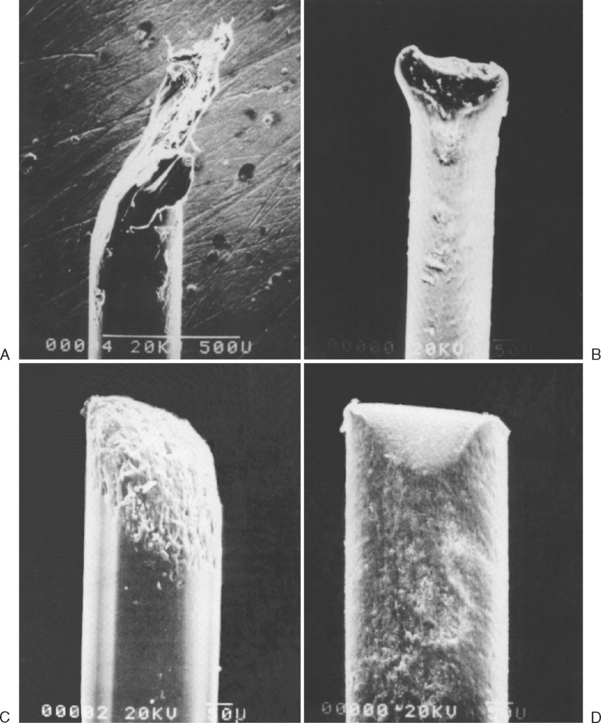
Today, most commercially available toothbrushes are manufactured with synthetic (nylon) bristles. Park and colleagues identify the bristle and head of the toothbrush as the most important part of the toothbrush, noting that the length of most bristles is 11 mm.12 Toothbrushes are classified as soft, medium, or hard based on the diameter of these bristles. The diameter ranges for these classifications are 0.16 to 0.22 mm for soft, 0.23 to 0.29 mm for medium, and 0.30 mm and greater for hard. In addition to the bristle diameter, the bristle end has been studied to determine the most beneficial type for plaque control. Of the three types of bristle ends (Fig. 11-2A to C), coarse-cut, enlarged bulbous, and round, the round end is the bristle type of choice because it is associated with a lower incidence of gingival tissue irritation. However, even the coarse-cut bristles round off eventually with normal use (see Fig. 11-2D).
The soft brush is preferable for most uses in pediatric dentistry because of the decreased likelihood of gingival tissue trauma and increased interproximal cleaning ability. In evaluating the best toothbrush head and handle for children, Updyke concludes that it is best to use a toothbrush with a smaller head and a thicker handle than an adult-size toothbrush to better access the oral cavity and facilitate the child’s grip of the handle.13 However, no single toothbrush design has been scientifically proven to be superior for removal of plaque. Multiple variables influence a toothbrush’s ability to remove plaque; therefore the practitioner should make recommendations only after assessing a patient’s individual needs.
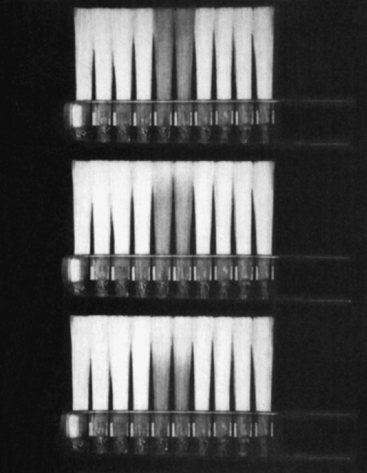
Wear rates of toothbrush bristles and their subsequent ability to remove plaque raise another concern. Dean suggests that toothbrushes remain effective well after patients identify a brush as being worn out.14 The cleansing effectiveness of toothbrushes is maintained until pronounced toothbrush wear has occurred. This implies that patients are much more likely to dispose of a brush well before its clinical usefulness actually ends than to continue to use a toothbrush that no longer cleans effectively. In this regard, one manufacturer claims that their commercial toothbrush (Oral-B Indicator, Oral-B Laboratories, Inc., Belmont, Calif) indicates when the brush should be replaced by means of centrally located tufts of bristles dyed with food colorant. When the blue band fades to halfway down the bristle, it is time to replace the brush (Fig. 11-3). The company states that on average this occurs after 3 months but that the time varies depending on the individual’s brushing habits.
FLOSS
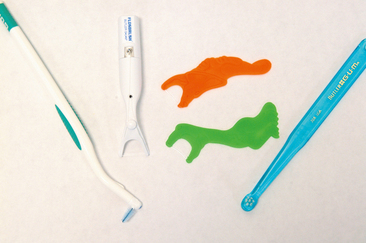
Although toothbrushing is the most widely used method of mechanical plaque control, toothbrushing alone cannot adequately remove plaque from all tooth surfaces. In particular, it is not efficient in removing interproximal plaque, which means that interproximal cleaning beyond brushing is necessary. Indeed, Corby and colleagues found that after a 2-week study period of 12- to 21-year-old well-matched twins, tooth and tongue brushing plus flossing significantly decreased the abundance of microbial species associated with periodontal disease and dental caries.15 Many devices have been suggested for interproximal removal of plaque, such as interdental brushes, floss holders and floss, and end tuft brush (Fig. 11-4). According to Mauriello and associates, there appears to be no substantial difference between these devices in their ability to remove plaque and their tendency to produce gingival inflammation effects when they are used properly; however, floss is the standard device to which other devices are most often compared.16 The other devices are more often recommended in certain unique circumstances, for example, the interdental brush may be recommended for orthodontic patients. Unfortunately, regular flossing does not occur daily in most households. Chen and Rubinson demonstrated that daily flossing was practiced by only 20% of mothers, 12% of fathers, and 6% of children within families.17 In addition, 28% of mothers, 45% of fathers, and 48% of children never floss their teeth. This low compliance rate, particularly in children, is a problem requiring our attention as practitioners.
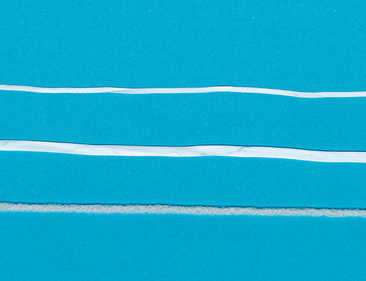
Several different types of floss are available: flavored and unflavored, waxed and unwaxed, and thin, tape, and meshwork (Super Floss, Oral-B Laboratories, Inc., Belmont, Calif) (Fig. 11-5). Almost all commercially available floss is made of nylon, although floss made of Teflon material (polytetrafluoroethylene) (Glide, W.L. Gore and Associates, Inc., Flagstaff, Ariz) is also available. The manufacturer claims that, because the material has a lower coefficient of friction than nylon, this floss does not shred, slides easily between tight contacts, and minimizes snapping of the floss.
Based on the work of Bass, unwaxed nylon-filament floss has generally been considered the floss of choice because of the ease of passing the floss between tight contacts, the lack of a wax residue, the squeaking sound produced by moving the floss over a clean tooth, and the fiber spread, which results in increased surface contact and greater plaque removal.18
However, more recent work indicates clearly that individual patient needs and preferences should be taken into account before floss selection recommendations are made. Carr and colleagues tested four different types of floss: waxed, unwaxed, woven, and shred resistant.19 They studied the reductions in interproximal plaque scores for 24 dental hygiene students. Statistical analysis revealed no significant differences between floss types in cleaning efficacy, comfort of use, or ease of use.
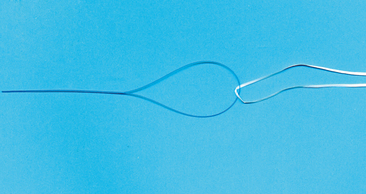
With these results kept in mind, it may help when making floss recommendations to parents for their children to consider both the parent’s and the child’s preferences and individual needs. From the perspective of patient acceptance, flavored waxed floss may be most effective. In addition, many parents complain that their fingers are too large for their child’s mouth. Floss-holding devices (see Fig. 11-4) are an excellent alternative for parents when this complaint is voiced or when the dexterity of the parent or child prevents handholding of floss. For orthodontic patients, the use of Super Floss or a floss threader (Fig. 11-6) helps in negotiating the floss under the archwires to allow for interproximal cleaning. For orthodontic patients, flossing is a tedious process but is nonetheless essential to maintenance of oral health.
POWERED MECHANICAL PLAQUE REMOVAL
The use of powered or electric toothbrushes has received considerable attention since the 1960s. The rationale for using powered brushes is that many patients remove plaque poorly because they lack adequate manual dexterity to manipulate the brush. The powered brushes should decrease the need for dexterity by automatically including some movement of the toothbrush head. However, initial studies into the plaque removal effectiveness of powered toothbrushes failed to demonstrate greater efficacy for powered than for manual toothbrushes. Although improvement was seen initially, over time the level of cleaning achieved with power toothbrushes declined to the same level obtained using manual toothbrushes. Kerlinger refers to this as the Hawthorne effect: almost any change or experimental manipulation will induce an improvement in behavior, apparently because of a novelty effect.20 The introduction of powered toothbrushes caused an initial increase in use, and therefore plaque and gingivitis were controlled. Over time, however, the results were comparable to those achieved with manual toothbrushes.
The Sonicare uses sonic technology in the form of acoustic energy to improve removal ability of traditional toothbrush bristles. The brush has an electromagnetic device that drives the bristles’ motions at 261 Hz, or 31,320 brush strokes per minute. Ho and Niederman found that the Sonicare toothbrush was significantly more effective than the manual toothbrush in reducing the plaque index, gingival index, percentage of sites that bled on probing, pocket depth, and total gram-negative bacteria in a subgingival plaque sample.21 Nowak and colleagues have demonstrated a 40% improvement in the debris index component of the Simplified Oral Hygiene Index in children aged 4 to 9 years who were using the Braun Oral-B Kids’ Power Toothbrush (D10).22 Studies by Grossman and Proskin23 and by Jongenelis and Wiedemann24 also compared the effectiveness of electric versus manual toothbrushes when the toothbrushes were specifically designed for children. Both studies concluded that the powered toothbrushes removed significantly more plaque than the manual toothbrushes for children. Finally, Heanue and associates performed a meta-analysis showing that power toothbrushes with a rotation-oscillation action design removed more plaque and reduced gingivitis more effectively than manual brushes in both the short and the long term.25 No other powered toothbrush designs were consistently superior to manual toothbrushes.
The Toothbrush Acceptance Program Guidelines of the American Dental Association (ADA) Council on Scientific Affairs list several requirements for powered toothbrushes that are not imposed on manual toothbrushes.26 Among these are evidence that the product can be used under unsupervised conditions by the average layperson to provide a 15% statistically significant reduction over baseline in gingivitis and a statistically significant reduction in plaque.
Also noteworthy is the development of the Braun Oral-B Interclean. (Braun GmbH, Kronberg, Germany). This electrically powered cleaning device requires only single-handed usage while its filament rotates to undergo an elliptical movement, disrupting plaque attached to adjacent and proximate teeth. Gordon and colleagues compared the effect of Interclean use and manual flossing over a 4-week period on level of interproximal plaque, gingivitis, and papillary bleeding in 52 healthy volunteers.27 The results demonstrated no statistically significant difference between manual flossing and use of the electric interdental cleaning device. Results from the personal preference phase of the study demonstrated that significantly more subjects preferred the interdental cleaning device (69.5%) to floss (24.5%). This new type of interdental cleaning device may be particularly helpful for adolescent orthodontic patients
DENTIFRICES
These formulations are useful because a child is more likely to practice oral hygiene procedures if the tools to be used are pleasing. Although the caries-preventive efficacy of fluoride toothpastes in children has been well documented, the impact of dentifrices on the total fluoride intake in children must be considered. Adair and associates confirmed that children tend to use larger amounts of dentifrice, brush for a longer period, and rinse and expectorate less when using a children’s dentifrice than when using an adult dentifrice.28 Levy and Zarei-M studied toothbrushing habits and quantities of toothpaste used on toothbrushes in children from birth through 6 years of age. Fig. 11-7 shows their results.29 This study did not quantify the amount of toothpaste, and therefore of fluoride, ingested from the use of this much toothpaste on the brush. However, the investigators suggest that ingestion was likely a substantial source of systemic fluoride for these children during the years when a risk of dental fluorosis is present. It is interesting to note that many toothpaste advertisements show children with large amounts of toothpaste on their brushes. Clearly, this is not the perception dentists want the public to have when regarding the use of fluoridated toothpastes in young children.
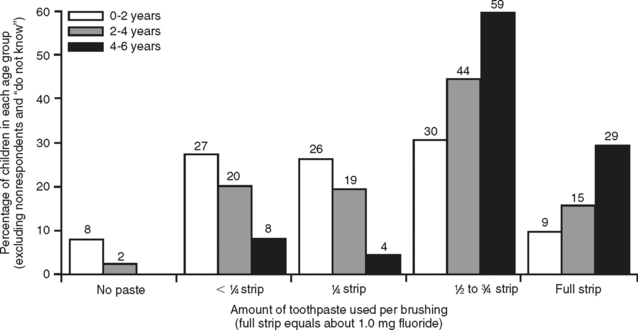
Figure 11-7 Quantity of toothpaste used by children from birth to 6 years of age.
(From Levy SM, Zarei-M Z. Evaluation of fluoride exposures in children. J Dent Child 1991;58:467-473.)
Simard and colleagues concluded from their study of 12- to 24-month-old children that 20% of the children ingested more than 0.25 mg of fluoride per day by toothbrushing alone.30 They suggest the following to reduce the chance of dental fluorosis in children secondary to toothpaste ingestion. Manufacturers should market a low-fluoride dentifrice for infants or reduce the diameter of the tube orifice. Parents should be advised to delay the use of fluoride dentifrice until the child is older than 36 months and to use small, pea-sized quantities of toothpaste. Pediatricians should take into consideration all sources of fluoride before prescribing supplements. In the wake of these recommendations, one manufacturer has developed a dentifrice for children called Baby Orajel Tooth and Gum Cleanser (Del Pharmaceuticals, Inc., Plainview, NY). The manufacturer states that it is nonabrasive, nonfoaming, without fluoride, safe for infants, and ideal for babies aged 4 months to 3 years. It contains a mild surfactant and simethicone, is sugar-free, and comes in vanilla and fruit flavors.
DISCLOSING AGENTS
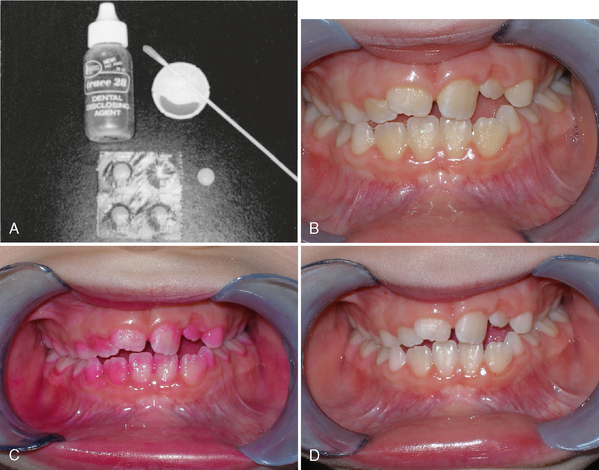
To increase the patient’s ability to remove plaque, several agents have been developed to allow for patient visualization of plaque. These include iodine, gentian violet, erythrosin, basic fuchsin, fast green, food dyes, fluorescein, and a two-tone disclosing agent. Use of these agents is particularly helpful in teaching children toothbrushing techniques and educating them on the rationale for oral hygiene. FDC red No. 28 is a plaque-disclosing agent commonly used either as a liquid to be dabbed onto the teeth with a cotton swab or in the form of a chewable tablet (Fig. 11-8). Unfortunately, this dye stains the oral soft tissues and dental pellicle, as well as plaque, leaving an objectionable pink discoloration that lasts up to several hours after use. Most younger children do not appear to be bothered by the discoloration, but as children approach adolescence it can become a problem. Fluorescein disclosing agents were developed to address this problem because fluorescein is not visible under normal light. Their use does, however, require special equipment.
In a study by Lim and colleagues, four different techniques were compared for clinically detecting plaque in patients using different dietary regimens.31 Subjects ranging in age from 18 to 27 years had their plaque levels assessed using a caries probe, a plaque-detection probe, erythrosin, and a two-tone disclosing agent at 3, 6, and 18 hours after thorough cleaning of their teeth. Thirty-eight patients were assigned to a sucrose-restricted (SR) diet in the first part of the study, and 32 patients were assigned to a sucrose-supplemented (SS) diet in the second part of the study. At 3 hours, plaque was detectable on more than 12% of sites in those consuming the SR diet and up to 23% in those on the SS diet. After 18 hours, the proportion of plaque-covered surfaces had increased to between 52% (SR diet) and 73% (SS diet). For minimal amounts of plaque, the disclosing solutions were found to be the most sensitive assessment techniques. For moderate and abundant plaque deposits, however, the probe techniques were more sensitive.
The clinical significance of these data is that, in measuring a patient’s oral hygiene abilities, one must assess plaque deposits immediately after the patient has cleaned his or her teeth. Otherwise, allowances must be made for factors such as the time elapsed since the teeth were cleaned and the patient’s diet. If a patient is seen several hours after the teeth have been cleaned, the quality of plaque control may be deemed unsatisfactory regardless of the quality of the patient’s performance. Disclosing agents also have some antimicrobial activity, according to Baab and colleagues.32 Although short-term quantitative inhibition of plaque growth has not been observed clinically, long-term home use of disclosing agents may contribute to qualitative differences in plaque composition. Further studies are needed to measure the long-term in vivo effect of these agents.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses