Chapter 11
Management of Cysts
Aim
This chapter describes the management of cysts of the mouth and jaws.
Outcome
After reading this chapter you should have an understanding of the techniques used to treat cysts affecting the oral structures.
Introduction
Cysts are pathological cavities containing fluid, semi-fluid or gaseous contents. They do not contain pus unless secondarily infected. They are usually epithelial-lined but the solitary (traumatic) bone cyst and aneurysmal bone cysts are exceptions to this. The radicular cyst (associated with the apex of a non-vital tooth) is the commonest odontogenic cyst. Cysts are not neoplastic. Very rarely malignant change may occur.
How do Cysts Form?
There are several theories of cyst formation. One of these suggests proliferation of the epithelial lining due to some unknown stimulus. Another theory suggests accumulation of fluid in the cyst as a result of hydrostatic forces resulting in resorption of any surrounding bone. Bony resorption is integral to facilitating cyst enlargement when the cyst lies within bone.
Clinical Presentation (Table 11-1)
Dental cysts are often asymptomatic and are noted as incidental radiographic findings. Others may produce signs and symptoms. Any infected cyst may present with pain and swelling, much like an abscess.
| Presentation of cysts |
| INCIDENTAL FINDING ON A RADIOGRAPH
SWELLING BONY EXPANSION INFECTION (PAIN AND SWELLING) DISPLACEMENT/LOOSENING OF TEETH/DENTURE ALTERED SENSATION |
Swelling may occur in the absence of infection (Fig 11-1). If enough bony resorption has occurred, an ‘eggshell’ layer of overlying subperiosteal new bone is present, which will often be felt to crack on palpation. Depending on the position of the cyst, displacement or loosening of teeth may occur. An enlarging cyst may cause problems in relation to the fit of a denture.

Fig 11-1 A dentigerous cyst associated with an unerupted lower second premolar. (a) Clinical appearance at presentation showing buccal swelling (b) Radiographic appearance at presentation. (c) Clinical appearance after treatment by marsupialisation showing erupted lower second premolar.
Altered sensation may be produced by pressure on anatomically related nerves. The latter is less common than might be expected, given the relatively slow speed of cyst enlargement. A rapid increase in size may occur if the cyst is infected. Altered sensation is a symptom that should always be taken seriously, as it may imply neoplasia.
Occasionally, a large cyst may cause a pathological fracture of the mandible. Cysts of the minor salivary glands (Fig 11-2) occur on the lip vermillion, cheeks, floor of mouth and palate. The cause is often trauma (e.g. lip or cheek biting). Saliva can then accumulate subsequent to duct rupture or stenosis. The two types recognised are mucous retention and mucous extravasation cysts. These are most common in children and adolescents. The cysts usually present as smooth fluid-containing bluish swellings. Periodically, they may burst but inevitably reform. In the floor of the mouth cysts arising from the sublingual gland may grow to large sizes and are denoted by the term ranula (Fig 11-3).

Fig 11-2 A mucocele in the lower lip of a three-year-old child.

Fig 11-3 A ranula.
Sometimes an ectopic part of the submandibular salivary gland invaginates the bone of the mandible near the angle. This appears as a well-defined corticated radiolucency below the inferior alveolar canal. It is known as a Stafne’s bone cavity or cyst but requires no treatment.
Investigations
History and clinical examination are important. Radiographic examination is also essential to determine the site and extent of intrabony lesions. Often two views at different angles are useful to examine for expansion of bone (Fig 11-4), which may also be evident clinically. Well-corticated margins are usually seen, but these often become indistinct when there is a history of infection.
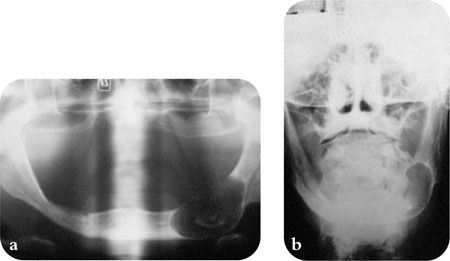
Fig 11-4 Radiographs showing a large residual cyst in the mandible. (a) A dental panoramic view. (b) A posterior-anterior mandibular view.
Electric pulp-testing of teeth close to the cyst can provide valuable information as to the etiology. Teeth with radicular cysts (see below) are non-vital.
In modern practice, aspiration is often not carried out initially. It may be carried out immediately prior to surgery, if there is doubt about the nature of the lesion. When managing more extensive lesions, a biopsy (see Chapter 13) should be taken of the cyst lining prior to more definitive surgery, once the nature of the lesion has been elucidated. An aspirate containing less than 40g per litre of soluble protein suggests an odontogenic keratocyst.
Classification
There are several classifications of cysts, but the World Health Organization (WHO) classification, which was revised in 1992, is often used. It is important to have an idea of cyst derivation as it may affect aspects of treatment (Table 11-2).
| EPITHELIAL CYSTS | AGE AT PRESENTATION (Decade) |
| Developmental | |
| Odontogenic | |
| Keratocyst | 2,3 |
| Dentigerous cyst | 3,4 |
| Lateral periodontal cyst | variable |
| Eruption cyst | &nbs/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


