Chapter 11. Endodontics in primary teeth
A. O’Donnell
SUMMARY
Endodontic treatment for deciduous teeth can be challenging due to the morphology of the root canal system, difficulties with correct diagnosis and behaviour management issues associated with a young patient. The vital, non-infected pulp should be preserved when appropriate. As with any endodontic treatment, the elimination of infection is critical to a successful outcome. There is a move away from formocresol and most paediatric dentists now prefer to use alternative medicaments. Root canal treatment of the infected primary tooth is, often, the best treatment option but it may be challenging and impractical to perform. A referral to a specialist may sometimes be necessary for endodontic management of primary teeth.
INTRODUCTION
The basic aims of endodontic treatment of primary teeth are similar to those for the permanent dentition: prevention or treatment of apical periodontitis, as well as the relief of associated symptoms including pain. It is generally accepted that primary molar teeth should be retained until they exfoliate naturally to avoid loss of space and crowding of the permanent dentition.
Although the response of primary teeth to infection is similar to that of adult teeth, morphological and physiological differences exist between primary and permanent teeth resulting in varying techniques for endodontic treatment. In addition, extra care must always be taken when carrying out endodontic treatment, especially on deciduous incisors. Parents must be warned of potential damage to the underlying permanent successor and the risks versus benefits discussed in full. A referral to a specialist paedodontic unit is sometimes necessary for endodontic management of primary teeth. When deciding on a suitable treatment plan for primary teeth, the clinician must consider whether the tooth should be saved with endodontic treatment or if extraction would be more advantageous. The following should be considered:
Factors related to the patient
• Patient cooperation – if a child is uncooperative or unable to cope with treatment in the dental chair, careful thought must be given to the potential benefits versus the risks of carrying out endodontic treatment under general anaesthesia. Although endodontic treatment enjoys a high success rate, the outcome cannot be guaranteed when there are compounding factors. If failure occurs, the child may be subjected to a repeat general anaesthetic to remove the tooth.
• Medical history – certain medical conditions will determine whether endodontic treatment should be undertaken. Children who are immunosuppressed, e.g. receiving chemotherapy, are not suitable candidates for endodontic treatment as there is the concern regarding a potential source of infection in the deciduous tooth. In patients at risk of infective endocarditis, endodontic treatment in deciduous teeth is also not recommended. However, endodontic treatment may be the treatment of choice in patients with coagulation disorders to avoid the risk of bleeding associated with an extraction. Children whose medical history contraindicates general anaesthesia, and who are unable to tolerate an extraction under local anaesthesia, may sometimes be able to cope with root canal treatment under local anaesthesia. For any child with a relevant medical history, the medical team should be consulted before deciding on the best treatment option.
• Irregular attenders and poor parental attitude to dentistry – this may lead the clinician to decide against endodontic treatment due to the inability to carry out regular clinical and radiological follow-up.
Factors related to the dentition
• Extent of dental decay – if the decay is extensive and restoration following endodontic treatment will be difficult or impossible then extraction is the treatment of choice.
• Extent of periapical infection – if gross, pathological resorption has occurred or the infection is severe, extraction may be the best option.
• Condition of the rest of the dentition – if this is poor and patient’s motivation to change diet and improve oral hygiene is not deemed to be high, extraction is usually recommended.
• Hypodontia – If there is no permanent successor, endodontic treatment may be the best option in order to keep the space for a future bridge or implant. 1 However, it is important to obtain orthodontic advice beforehand; the deciduous tooth may be best removed and, provided the timing is right, the space may be used orthodontically.
• Balancing in primary canines and first molars – if the contralateral tooth has been lost, it may be preferable to carry out a ‘balancing’ extraction rather than perform endodontic treatment, especially when the arch is crowded.
• Remaining natural lifespan of the tooth – it is generally accepted that primary molar teeth should be retained until they exfoliate naturally to avoid loss of space and crowding of the permanent dentition. However, if physiological root resorption has affected two-thirds or more of the roots, then endodontic treatment is not a sensible option as the tooth is close to being exfoliated.
TREATMENT OF PRIMARY TEETH
Primary teeth differ morphologically from their permanent successors both in shape and size; pulp space anatomy of primary teeth is covered in Chapter 4. In general, the enamel and dentine are thinner than in a permanent tooth. Pulpal changes in response to caries, therefore, occur more rapidly and even lesions that appear very minimal clinically can extend into the pulp (Fig. 11.1). Primary molars have fine tapered roots which are flattened mesiodistally to enclose a ribbon-like root canal system and their pulp chambers are relatively larger than permanent teeth. The single root canal may become partially calcified with age, 2 to produce several intercommunicating canals, thus making instrumentation of the radicular pulp space difficult. Many lateral canals have been reported to exist in the furcation of primary molar teeth, 3 and these may contribute to the early spread of infection from the pulp chamber to the interradicular area. 4
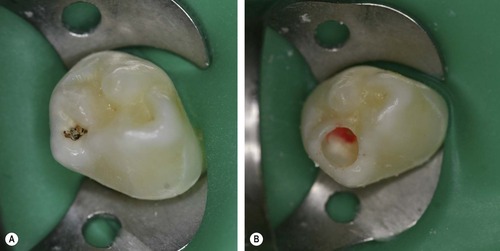 |
| Figure 11.1
Carious deciduous molar. (A) The carious lesion appears minimal clinically. (B) Pulpal exposure following total caries removal.
Reproduced courtesy of M.Vaidyanathan.
|
The correct diagnosis of pulp disease is important as this will determine which endodontic treatment procedure will be required. The diagnosis is dependent on the combination of a good history, clinical and radiological examination. A clear history of clinical symptoms is especially difficult to obtain in young patients because they are usually unable to give an accurate pain history, and parental report is usually relied upon. Symptoms of irreversible damage will include a history of spontaneous pain, severe pain at night and pain on biting. The clinical examination should begin with assessing the extent of the caries. It has been reported that in the majority of primary molars with marginal ridge breakdown there is pulpal inflammation involving the pulp horn adjacent to the carious lesion. 5 The presence of abnormal tooth mobility, intraoral swelling, discharging sinus tracts and tenderness to pressure will also indicate periapical pathosis. In primary teeth, sensitivity testing has been shown to be an unreliable guide to the histological status of the pulp,6.7. and 8. so a combination of the history, clinical and radiological examination provides an indication of the pulpal status.
If the child is cooperative, preoperative radiological examination is invaluable. This provides information regarding root morphology, periapical pathosis, resorption and calcifications, aiding diagnosis and assessment of any local contraindications to endodontic treatment. The treatment techniques that have been advocated for use on primary teeth may be grouped as follows:
• indirect pulp capping
• direct pulp capping
• pulpotomy
• pulpectomy.
In all cases, the administration of local anaesthesia and adequate tooth isolation, preferably with rubber dam, are advised. For vital maxillary teeth, infiltration anaesthesia is usually satisfactory, whereas a nerve block or intraligamentary injection may be more suitable for mandibular molar teeth. It cannot be overemphasized that a successful treatment outcome is dependent on correct diagnosis, appropriate technique and the provision of a definitive restoration, ideally a preformed metal crown, which will provide a good coronal seal. 9 All primary teeth that have had an endodontic procedure carried out should be followed up clinically and radiographically.
Indirect pulp capping
This is the term used to describe the placement of a dressing over residual carious dentine in an attempt to allow secondary dentine to be formed within the pulp chamber. 10 Exposure of the pulp is, therefore, avoided in teeth with deep carious lesions when there is no clinical or radiological evidence of pulpal or periapical disease. Removal of caries from the lateral wall ensures that there is an adequate seal between the tooth and the restoration so that microbes are deprived of the nutrients necessary for their survival. 11,12 Contraindications to this method of treatment include any evidence of an irreversibly inflamed or necrotic pulp such as a history of spontaneous pain, associated swelling, tenderness to biting, or abnormal tooth mobility. Likewise, preoperative radiographs must be examined for pathological root resorption, pulp calcifications or periapical radiolucency, which if present, would necessitate less conservative treatment.
At the initial visit, all soft carious dentine is removed with a bur in a slow-speed handpiece or by hand with an excavator. The amelodentinal junction must be free from all softened carious dentine. The area of dentine over the site of a potential pulpal exposure is covered with a layer of hard setting cement containing calcium hydroxide (e.g. Dycal, Dentsply, Weybridge, Surrey, UK) and sealed with an overlying structural base of a quick-setting, reinforced zinc oxide–eugenol preparation (e.g. IRM, Dentsply) or glass ionomer cement. A success rate of 92% for indirect pulp capping with calcium hydroxide in primary incisors followed for 42 months has been reported, 13 and 96% in primary molars after 1 year. 14 Alternatively, an adhesive resin system may be used, directly over the dentine which has shown to have a success rate of 96% compared with 83% for calcium hydroxide. 15 Other studies have shown success when glass ionomer is placed over the dentine, 16 which offers the additional benefit of fluoride release. The final restoration can then be placed. The indirect pulp cap technique has been shown to be clinically more successful than formocresol pulpotomy, 17,18 and therefore, offers an alternative to the pulpotomy technique. Some authors have advocated a two-stage procedure where the tooth is re-opened 3 months later and further caries removal is performed. 18 Due to the high success of the one-stage indirect pulp cap, this is no longer necessary and regular review of tooth vitality is preferable to subjecting the patient to subsequent re-entry into the tooth.
Direct pulp capping
Direct pulp capping is generally not advocated for primary teeth due to limited evidence of success in the literature. Inflammation within the pulp can persist and is followed by necrosis or internal resorption. The only possible application of this technique is when pulp tissue has been mechanically exposed as a result of cavity preparation, 19 or when the tooth is close to exfoliation. 20 Calcium hydroxide is placed on the exposure and encourages formation of a dentine bridge below the exposure site in an attempt to maintain pulp vitality (Fig. 11.2). The technique should not be used for carious exposures.
 |
| Figure 11.2
Pulp cap with calcium hydroxide.
Reproduced courtesy of T.Kandiah.
|
The exposure site should be gently irrigated with a non-irritant solution, e.g. saline, to remove any debris that may impede healing and also to keep the pulp moist. The capping material should be flowed gently over the exposure and allowed to set. Various capping materials have been employed. Calcium hydroxide used alone or in conjunction with zinc oxide–eugenol, has been most widely investigated. 21,22 The use of dentine bonding systems has also been advocated and promising results have been reported. 19,23 The advantage is that a polymer film can be layered over an exposure site without displacing the pulp, and onto surrounding dentine where it permeates the tubules. Further work is required before these materials can be recommended as capping agents. A more promising material is Mineral Trioxide Aggregate (MTA), which is biocompatible and has good sealing properties. 24 Favourable results have been reported for MTA direct pulp capping on deciduous molars compared with calcium hydroxide; 25 and clinical case reports have also supported the use of MTA. 26 Following pulp capping and final restoration, the tooth should be monitored clinically and radiologically for any signs of subsequent pulp necrosis or extensive resorption, indicative of treatment failure.
Pulpotomy
Vital (full coronal) pulpotomy involves the removal of the entire coronal pulp that has undergone irreversible inflammatory changes or necrosis, leaving remaining healthy vital tissue intact within the root canal system. The cut radicular pulp stumps are covered with a medicament which will result in either healing or ‘fixation’ of the tissue beyond the interface of dressing and radicular pulp. Vital pulpotomy provides the most suitable method for treating carious exposures in primary teeth without a history of spontaneous pain, swelling, sinus tract, any evidence of internal or external root resorption, or periapical pathosis. Its success is dependent on correct diagnosis, control of haemorrhage from the radicular pulp and achieving an excellent coronal seal. A preformed metal crown is the final restoration of choice as this minimizes the risks of tooth fracture and microleakage, and hence enhances the prognosis.
The basic technique consists of the following steps:
• Local anaesthesia and adequate isolation.
• Caries removal.
• Extend cavity so that entire roof of the coronal pulp chamber is removed.
• Rose head bur in a slow-speed handpiece or a hand excavator to remove coronal pulp tissue.
• Control haemorrhage with sterile cotton wool pledgets (if bleeding continues this may mean that initial diagnosis is incorrect and the pulp is irreversibly damaged, so pulpectomy is the treatment of choice).
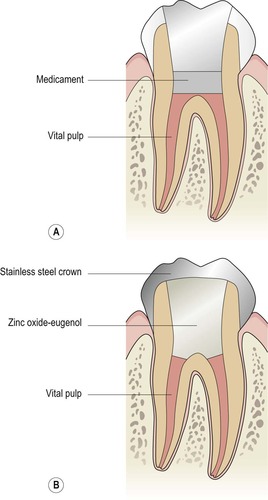
• Placement of pulpotomy medicament (Fig. 11.3A).
 |
 |
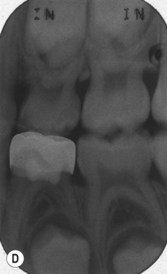 |
| Figure 11.3
Vital pulpotomy. (A) Following caries and coronal pulp removal, medicament is placed; (B) the pulp chamber is then filled with zinc oxide-eugenol cement and the tooth restored with a preformed metal crown (based on the original drawings by A Muir). (C) Clinical view of a preformed stainless steel crown. (D) Example of a follow-up radiograph.
Reproduced courtesy of M.Vaidyanathan.
|
• Coronal restoration of the tooth (Fig. 11.3B,C).
• Follow-up (Fig. 11.3D).
Electrosurgery may be used for pulpotomy procedures to either remove the pulp tissue or to control haemorrhage; the main advantage is that the need for any potentially toxic medicament can be avoided. However, it was reported that when electrosurgery was used to remove the entire coronal pulp and treat the remaining stumps, root resorption occurred. 27 An alternative method may be to remove the coronal pulp mechanically and treat the remaining pulp stumps electrosurgically28 in order to avoid excessive heat dissipation. Although a clinical and radiological success rate of 99% has been demonstrated at 2 years, 29 the electrosurgical pulpotomy technique is still experimental and not widely adopted. Lasers have also been suggested as an alternative instrument but some studies have shown carbonization, necrosis and inflammation of the pulp with little evidence of repair.19.30. and 31. A study on laser pulpotomy versus the formocresol technique carried out on caries-free primary molar teeth, which were scheduled for extraction reported comparable results. 32 Due to limited evidence, the expense involved and the success of alternative techniques, lasers are rarely used for pulpotomies in children.
Medicaments
Medicaments are used in endodontic treatment of primary teeth as wound dressings, tissue fixatives, disinfectants and inflammatory suppressants. A systematic review of the literature on the relative effectiveness of various medicaments and techniques for treating primary molar teeth with decay involving the pulp found that the evidence available did not support the superiority of one type of treatment over another. 33 Therefore, the choice of treatment is very much dependent on clinical presentation and the individual operator.
Formocresol
Buckley34 formulated a solution containing equal parts of formalin and tricresol. A commercial solution containing 19% formaldehyde, 35% cresol in a glycerine/water vehicle (Buckley’s formocresol, Cosby laboratories, Burbank, CA, USA), was later developed as a suitable medicament for the treatment of pulpally exposed primary teeth. The aim of this treatment technique is to fix the coronal portion of the radicular pulp and to maintain vitality of the remaining apical portion. 35,36 Formocresol acts through its aldehyde group and binds to the amino acids of protein and bacteria to prevent autolysis and hydrolysis so rendering tissue inert. 37
Over the years, there has been increasing concern about the toxicity, both local and systemic, of formocresol. Experimental evidence has shown that sufficient formocresol was absorbed systemically from multiple pulpotomy sites in an experimental animal to induce early tissue injury in the kidneys and liver.38.39. and 40. However, it was argued that due to the quantity normally used in man, the risk is much less and may therefore be negligible. A definite relationship between formocresol pulpotomies in primary teeth and enamel defects on their permanent successors has been demonstrated, 41 but not confirmed in other studies. 42,43 In addition, carcinogenic and mutagenic properties have been recognized, which together with local and systemic effects, have led to the use of a 20% (1 : 5) diluted solution. 44,45 The International Agency for Research on Cancer (IARC) classified formaldehyde as a carcinogen in 2004. Case control and cohort studies of workers exposed to formaldehyde daily have shown an association between formaldehyde exposure and nasopharyngeal cancer and leukaemia. This has raised questions as to the continuing use of formocresol in children. The use of alternative medicaments has been debated within the literature due to alternative methods being shown to be equally successful clinically.46.47. and 48. Although a recent evaluation of the research regarding safety of formaldehyde concluded that there was inconsequential risk of carcinogenesis associated with formaldehyde use in paediatric pulp therapy, 49 there is continuing unease. There is a growing movement away from using formocresol and most paediatric dentists now prefer to use alternative medicaments. Nevertheless, the clinician should always consider each case individually and involve parents in the decision-making process when treatment planning.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


