Caries Prevention
Göran Koch, Sven Poulsen, Svante Twetman, and Christina Stecksén‐Blicks
Concepts of caries prevention
The first carious lesion and its restoration marks the initiation of a series of event that during the tooth’s lifetime will end up in more and more complicated restorations. Today there is sufficient scientific knowledge about the etiology of caries and about factors that interfere in this process in order for us to develop effective preventive strategies. This knowledge should be used to its full extent in an attempt to control caries.
Though recent decades have seen a reduction in dental caries occurrence (see Chapter 10), it is still a common disease of childhood and adolescence. Therefore, caries prevention should be given a high priority by the dental profession as well as by local and national health authorities. In this context, the pediatric dentist has a very specific responsibility in meeting the challenge to assist keeping children and adolescents free from caries. For example, very young children with early signs of caries should be given special attention, as they tend to develop more caries compared to children without early signs of caries (see Chapter 10).
Even if the principles of caries prevention are simple, the implementation, management, and evaluation of programs and recommendations can be difficult. For example, it has been shown in controlled clinical trials that professional removal of plaque every second week combined with strong motivational activities resulted in almost complete caries control in children [1], whereas a field study with a similar regimen but carried out with less enthusiasm or motivation did not give the same results [2].
Different terms are used to categorize preventive activities. Oral health promotion is an activity which takes place at the community level with the purpose of making it easier for people to live a healthy life through so‐called “healthy choices.” Systemic administration of fluoride through different vehicles is an example of an oral health promotion activity. Water fluoridation, introduced in the 1940s, has been found to be the easiest and cheapest method of systemic administration and caries reductions of 40–50% have been reported. It is recommended by the World Health Organization as an important caries‐preventive measure but its use is limited to large communities with water plants of high technical standard. In rural areas with small water plants and less control of the implementation, water fluoridation must be considered unrealistic. Long‐term systemic fluoride exposure via water during the period of tooth development and mineralization and thereafter throughout life has a documented caries‐reducing effect in both children and adults. However, the caries reduction from community water fluoridation is now considerably less than when the method was introduced, mainly because of the increased exposure to other fluoride sources such as food, beverages, toothpastes, and topical agents. In areas without access to optimal levels of fluoride, and not established fluoridation programs addition of fluoride to milk or table salt has been recommended and tested, but the preventive effects are unclear (See: World Health Organization. Oral Health: Action plan for promoting and integrated disease prevention. Resolution WHA 60.17 May 2007. Geneva:WHO).
In addition, there has been an increasing scientific understanding and also acceptance that systemic administration of fluoride pre‐eruptively has little effect in a caries‐preventive perspective. Much of the effect of systemic application of fluoride has been explained by the simultaneous topical fluoride exposure posteruptively. So, if fluoride tablets are used they should be sucked or chewed.
Reducing schoolchildren’s access to sweet snacks through school policies is another example of oral health promotion. An important aspect of oral health promotion is that it may also result in the reduction of other health problems such as being overweight, because many health problems have common risk factors (the “common risk factor approach”: see Chapter 10). In contrast to health promotion, prevention aims at reducing the risk of a specific disease. Prevention is described at three levels: primary, secondary, and tertiary:
- primary caries prevention is preventing new caries lesions from occurring
- secondary caries prevention is early detection and intervention to arrest early caries lesions
- tertiary caries prevention is restoration of cavitated lesions in order to prevent further destruction, eventually leading to the loss of the tooth.
It can be argued that primary caries prevention in itself is not a meaningful category as all preventive methods can be categorized as both primary and secondary prevention. For example, fluorides in the biofilm slow down the biofilm activity and demineralization but also remineralize subclinical caries lesions and thus arrest their progression.
Evidence‐based prevention
Evidence‐based practice has now become the focus of all health care practices, including pediatric dentistry, and preventive care for children and adolescents. According to Sackett [3] evidence‐based care is “an approach to oral health care that requires the judicious integration of systematic assessments of clinically relevant scientific evidence, relating to the patient’s oral and medical condition and history, with the dentist’s clinical expertise and the patient’s treatment needs and preferences.” In pediatric dentistry – as in most other dental specialties – the scientific evidence for the efficacy of most of the interventions is relatively weak. In spite of this, the clinician has to approach a clinical problem according to his or her best ability, by balancing the three components of evidence‐based care shown in Figure 11.1.
Figure 11.1 The triad forming the base for evidence‐based practice.
The randomized controlled trial
The randomized clinical trial (RCT) is the most valid scientific method for assessing the efficacy of preventive methods and has been used for testing a number of caries‐preventive agents and procedures. New preventive methods are, however, continuously being launched. For this reason, the pediatric dentist needs a basic knowledge of the most important characteristics (Box 11.1) of RCTs on caries prevention to be able to assess the quality of trials, understand the results, and skillfully apply them in the development of effective and efficient preventive programs.
The strength of the RCT is its ability to eliminate bias through randomization and the use of blinding procedures. The design is shown in Figure 11.2. It usually runs for a minimum of 3 years and the efficacy of the method is assessed by calculating the difference in new caries lesions between a control group and the experimental group(s). When the first caries‐preventive trials of fluoride‐containing agents were conducted they comprised one or more experimental groups and a placebo‐treated control group. Since the caries‐preventive effect of fluoride agents is so well established it is no longer considered ethical to include nonfluoride‐treated groups in preventive trials of fluoride agents. Thus new preventive methods often have to be compared to groups receiving already implemented methods.
Figure 11.2 Basic design of the randomized controlled caries clinical trial. Study subjects should be assigned randomly to one or more experimental or intervention groups and a control or no intervention group. The outcome of the trial is measured by comparing caries increment in the group(s) from the beginning to the end of the trial (M1 to M2).
With today’s reduced level of caries in children and adolescents the size of the RCT becomes an important methodological issue. With the relatively high caries level 20–30 years ago, small sample sizes could still give sufficient statistical power. With the decrease in dental caries incidence, sample sizes of 1000 or more subjects per group may be necessary to give sufficient power to the trial. Some trials may require a sample size so large that they become unrealistic for logistic and other reasons. The statistical power of a trial is important for the interpretation of the results of the trial. A small trial might not have sufficient statistical power to detect an effect, and may erroneously be interpreted as “evidence of no effect,” while a correct interpretation is: “no evidence of effect.”
The efficacy is calculated as shown in Box 11.2:
- absolute difference
- prevented fraction
- number needed to treat.
Absolute differences are dependent on the level of disease in the population, and will have to be recalculated as Prevented Fractions (PF) in order to apply to other populations. PF may, however, be misleading when it comes to deciding on implementation in the field, since high percentage reductions may be of little practical importance in populations with low caries activity. Number needed to treat (NNT) is now also calculated as it has the advantage of giving the clinician an impression of how many individuals have to be treated in order to obtain an effect.
Where to find the evidence
For the pediatric dentist it will be impossible to keep up with the RCTs published in the literature for several reasons. First of all, the literature is large, and constantly growing. Second, the methodology – especially the statistical procedures for analysis – is beyond the competencies of a practicing dentist. Finally, it will be difficult to synthesize the information from the many individual trials to decide on what to do for a given patient or community. Clinicians find review literature (secondary literature), which summarizes RCTs more relevant and easier to understand (Box 11.3). The most valid kind of secondary literature is the systematic review, which is a highly formalized review procedure based on systematic search strategies of the literature, critical appraisal, and analysis of the evidence from the literature. The most well‐known systematic reviews are undertaken by the Cochrane Collaboration (www.cochrane.org). Other organizations are, however, also performing systematic reviews of relevance to the pediatric dentist, e.g., SBU (www.sbu.se), NICE (www.nice.org.uk), and SIGN (www.sign.ac.uk). In Box 11.4 examples of reviews on the effect of topical fluorides on caries are presented.
How does caries develop?
An important basis for prevention is an understanding of causation. In epidemiology, a cause is defined as a factor that influences the risk of disease, and causal factors are often arranged in what epidemiologists know as “webs of causation.” This concept has been used as a model for understanding dental caries [4], and Box 11.5 illustrates how causes of, e.g., early childhood caries can be identified and operated at several different levels:
- at the tooth surface, where a complex interplay takes place between host factors, diet, and the biofilm
- in the interaction between members of the family
- in the living conditions of children and their families.
This understanding has given rise to the concept of “upstream” and “downstream” causal factors. Downstream causal factors are those that are active close to where the caries lesion is observed, i.e., at the tooth surface; while upstream factors are those that affect the living conditions of the family. It is important to underline that it is the responsibility of pediatric dentists to try to reduce causal factors for dental caries at all levels. This means understanding and being interested in health promotion to improve general living conditions and health of children, as well as using all possible methods of prevention to prevent new caries lesions from occurring, and to detect and arrest early initial lesions. The remaining part of this chapter is mainly concerned with caries risk assessment and prevention, and is based on an understanding of the disease as being multifactorial and caused by the interaction between the biofilm, the substrate available for the biofilm, and host factors. The model developed by Rothman et al. [5] for understanding complex diseases and conditions may help in structuring our thoughts (Figure 11.3). According to this model, disease occurs when a set of component causes (in the case of caries: biofilm, sugar, and unfavorable host factors) combine to constitute a sufficient cause.
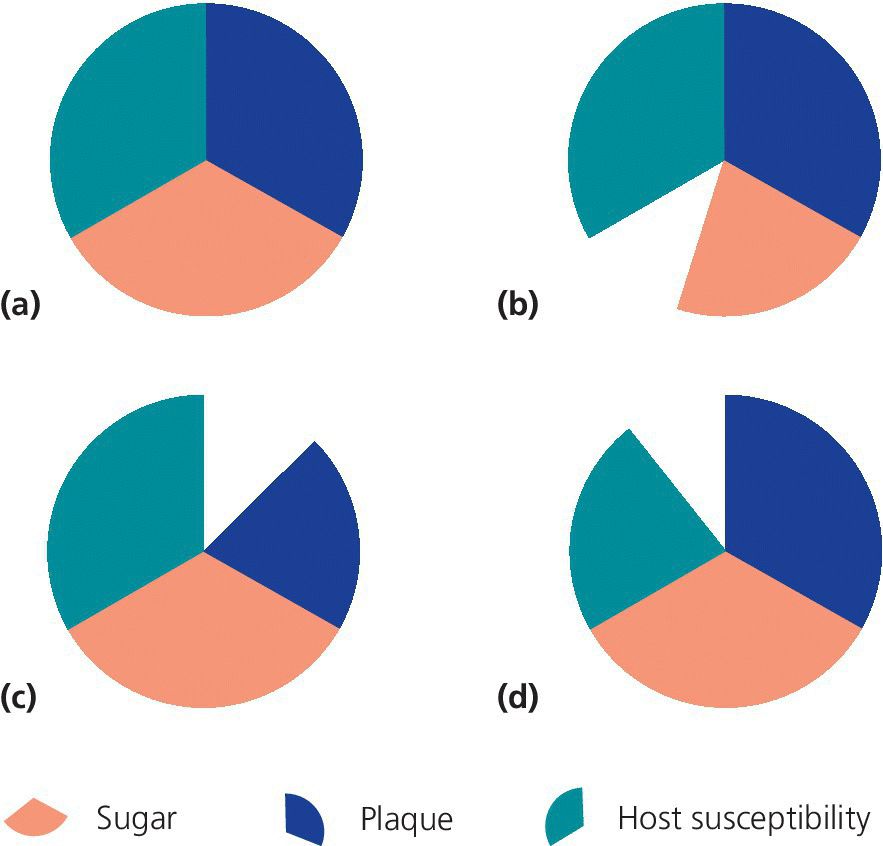
Figure 11.3 A conceptual model, where disease is explained as occurring when a number of component causes (sections of the circle) act together to form a sufficient cause (closed circle). (a) High level of plaque, high sugar intake, and high susceptibility to caries will result in a caries lesion. (b) If the sugar intake is reduced, (c) if the plaque level is reduced, or (d) if the susceptibility is decreased, caries lesions will not occur.
Caries risk assessment
A structured caries risk assessment is the clinical process of evaluating the patient´s caries risk factors and judging whether these will outweigh the preventive factors. Thereby, it is an essential component in the decision‐making process for adequate prevention and management of dental caries and for individual timing of follow‐up and recall intervals [6]. Ideally, etiologic risk factors or non‐etiologic risk indicators should forego the disease in order to institute upstream prevention. The clinical risk assessment process is sometimes mixed up with caries prediction, which is the scientific/statistical modeling of factors related to caries development in populations or defined groups of people. The validity of caries predictors is determined in prospective trials without any intervention and the outcome is expressed in continuous values such as sensitivity and specificity (Box 11.6). The sensitivity and the specificity can vary between 0 and 1, the higher the better in terms of accuracy. When the sum of sensitivity and specificity is 2, the predictor, or combination of predictors, is perfect. It is however important to underline that such predictive values only are “true” under the conditions of that specific investigation and the external validity is limited. Nevertheless, findings from predictive studies are often extrapolated to the practitioner’s situation. An individual caries risk assessment can only be proven right or wrong; the paradox is that the skilled clinician, making a correct risk assessment with subsequent adequate and effective primary prevention, may turn out to be “wrong.” Consequently, caries risk assessment is an inexact science that is difficult to master with high quality studies.
As caries is a biofilm‐mediated multifactorial disease, it is generally understood that a comprehensive risk assessment should be based on a range of risk factors associated with the disease that are balanced against a range of protective factors to which the patient may be exposed (Figure 11.4). Thus, multiple variables based on socio‐economy, lifestyle, behavior, general health, diet, oral hygiene, clinical observations, and past caries experience are commonly proposed, varying with the age group at which they are targeted. According to the current risk profile, the patient is then grouped into one of several fixed risk categories (e.g., low risk, moderate risk, or high risk). The higher the risk, the more extensive preventive care should be and offered. Likewise, a higher risk calls for more frequent follow‐ups.
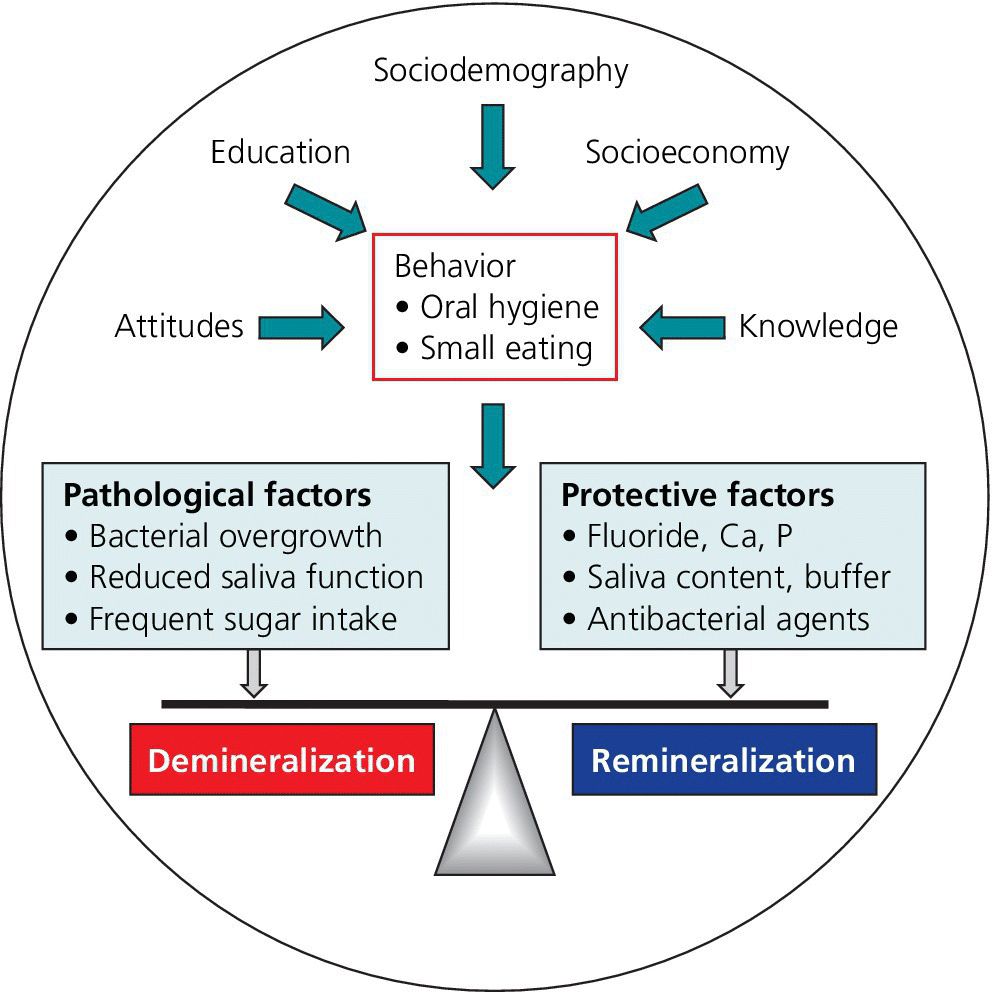
Figure 11.4 Caries balance as influenced by social, behavioral, and biological factors.
Risk ages
A clinical risk assessment should always be performed at the child’s first visit and then regularly throughout childhood since up to 50% of all children may change their risk category for better or for worse. It is also important to conduct caries risk assessments linked to social or medical life events such as onset of chronic diseases, disabilities, feeding problems, and divorce in the family. An additional strategy is to utilize the “risk age concept” which means that more or less all children exhibit increased caries risk at certain ages. The first period in life which merits special attention is 1–3 years during which the primary teeth are erupting. Several studies have emphasized the importance of an early risk assessment at one year of age in order to combat early childhood caries by assisting parents to establish good oral habits. Such activities are of special importance in vulnerable or immigrant groups. The second risk period in life appears at 5–7 years when the first permanent molars erupt with caries‐susceptible fissures that could be addressed with a structured sealant program. Finally, the turbulent teenage period (12–15 years) offers a high number of newly erupted molars and premolars susceptible for decay that warrants a risk‐based preventive approach.
Accuracy of caries risk estimations
A recent systematic review has evaluated the quality of evidence and ability of multivariate models and single factors to correctly identify future caries development in children [7]. The main results are summarized in Table 11.1. Despite extensive research, it seems obvious that there is no perfect or superior model or method to predict caries in children. In general, the clinical variables were stronger than the nonclinical and short‐term predictions (up to 2 years) were more reliable than long‐term predictions. Moreover, the multivariate models and baseline caries prevalence performed better in preschool children than in schoolchildren and adolescents. Sensitivity and specificity values above 0.8 are considered acceptable for caries risk and this could be reached with “best scenario” multiple models when applied to young preschoolers [8]. Past caries experience (dmfs/DMFS) was the most powerful single predictor in all age groups while quantification of bacteria levels in saliva displayed a high specificity but a poor sensitivity. In general, the probability of correctly identifying true high‐risk individuals was somewhat lower than the probability of finding the subjects with low caries risk. The quality of the evidence was generally low due to inconsistencies and study limitations [7].
Table 11.1 Accuracy and quality of evidence for various models and single factors to predict caries in children.
Adapted from the systematic review of Mejàre et al. 2014 [7]. Reproduced with permission of Taylor & Francis
| Age group/risk factor | Accuracy1 | Quality of evidence2 |
| Preschool children | ||
| Multivariate model | good/moderate | ⊕⊕OO |
| Baseline caries prevalence | good/moderate | ⊕⊕OO |
| Socio‐demography/economy | limited/poor | ⊕⊕OO |
| Dietary habits/attitudes to diet | poor | ⊕⊕OO |
| Oral hygiene/use of fluoride | poor | ⊕⊕OO |
| Mutans streptococci/lactobacilli | poor | ⊕⊕OO |
| Schoolchildren and adolescents | ||
| Multivariate model | limited | ⊕⊕OO |
| Baseline caries prevalence | limited | ⊕⊕OO |
| Dietary habits | limited | ⊕⊕OO |
| Oral hygiene/use of fluoride | insufficient | ⊕OOO |
| Mutans streptococci/lactobacilli | insufficient | ⊕OOO |
| Post‐eruptive age | moderate | ⊕⊕OO |
1 The accuracy (utility) of models and single predictors was graded in three levels according to the sum of sensitivity and specificity: ≥1.5 = good/moderate; <1.5 ‐ ≥1.3 = limited, and <1.3 = poor.
2 According to GRADE: Strong (⊕⊕⊕⊕): Based on high or moderate quality studies containing no factors that weaken the overall judgment; Moderate (⊕⊕⊕O): Based on high or moderate quality studies containing isolated factors that weaken the overall judgment; Low (⊕⊕OO). Based on high or moderate quality studies containing factors that weaken the overall judgment; Very low (⊕OOO). The evidence base is insufficient when scientific evidence is lacking, quality of available studies is poor or studies of similar quality are contradictory.
Practical considerations
A caries risk assessment should be an integrated part of the clinical process. For a comprehensive caries risk assessment, it is advisable to collect information from the case history, clinical and radiographic examinations, and supplementary tests.
Case history
The case history should cover the child’s social situation, medical background, and current medication. There are few general diseases that directly affect the teeth but the medication in combination with demanding care and parental anxiety may move the focus from normal oral care routines. Some drugs have a high content of sugar and/or a low pH and the depressing influence on saliva secretion is a clear risk for caries development. Neuropsychiatric or functional disorders such as attention deficit hyperactivity disorder (ADHD) are linked to impaired dental health. Poor economy and a troubled family or social situation can also contribute to neglected oral health routines and unhealthy eating. The collection of a dietary history gives important information on frequency and the total sugar intake that provides a starting point for motivational interviews. Information on present and past fluoride exposure as well as the current oral hygiene routines should also be used in the risk assessment process.
Clinical examination
The clinical examination provides information on the past and current caries situation and the prevalence is an indication of host susceptibility. It is important that the teeth are examined dry and clean in order to be able to detect early signs of enamel demineralization as an indication of an active caries process. The extension and appearance of such early lesions should be carefully assessed. For example, a whitish rough area in the enamel with loss of luster along the gingival margin is more likely to be active than a brownish shiny area with smooth surface. Furthermore, lesions could be staged as initial, moderate, or extensive to facilitate estimations of progression. Local aggravating factors such as crowded arches, deep fissures, and enamel morphology should also be taken into consideration. The level of oral hygiene can be estimated with a disclosing solution. The presence of gingivitis and visible plaque on the labial surfaces of maxillary incisors of a toddler may be a marker of risk.
Supplementary tests
Supplementary saliva tests can contribute with useful information on factors of importance for the caries process. Hyposalivation occurs rarely among children but estimations of the salivary secretion rate are important in medically compromised children. In childhood, the stimulated secretion rate is dependent on age and cooperation. For schoolchildren, stimulated values less than 0.5 mL/min should be considered low. Simple chair‐side tests can provide additional information on salivary buffer capacity and counts of aciduric bacteria (mutans streptococci and lactobacilli) as biomarkers of a cariogenic environment. In infants and toddlers, bacteria sampling can be carried out with the aid of a wooden cotton pin that is wetted in saliva and streaked along the gingival margin of the upper incisors. The pin is then rolled on the chair‐side tests for subsequent cultivation.
Some key factors that affect caries risk are listed in Table 11.2. There are several formal and informal methods and models available to establish a child’s caries risk profile and to compile the obtained data for risk categorization. According to a questionnaire, most dentists make an informal and subjective evaluation of their child patients based on previous caries, oral hygiene, saliva flow, and “gut feeling” [9,10]. Only 14% used a pre‐formed template or computer software [9]. It has been demonstrated that such algorithm‐based models increase both objectivity and consistency and must therefore be regarded as best clinical practice [11]. The accuracy per se may however not be significantly increased but the educational and interactive nature of a computerized risk assessment program makes them useful in patient communication and motivation. An example of such program, the Cariogram, is shown in Figure 11.5. Digital dental records are obtainable with some form of risk assessment tool integrated into the system but unfortunately, to date, none of them are validated against the true outcome.
Table 11.2 Example of factors that may affect caries risk in children
| Low caries risk | Elevated caries risk |
| Medical background | |
|
|
| Family and socio‐economy | |
|
|
| Oral hygiene | |
|
|
| Diet | |
|
|
| Caries | |
|
|
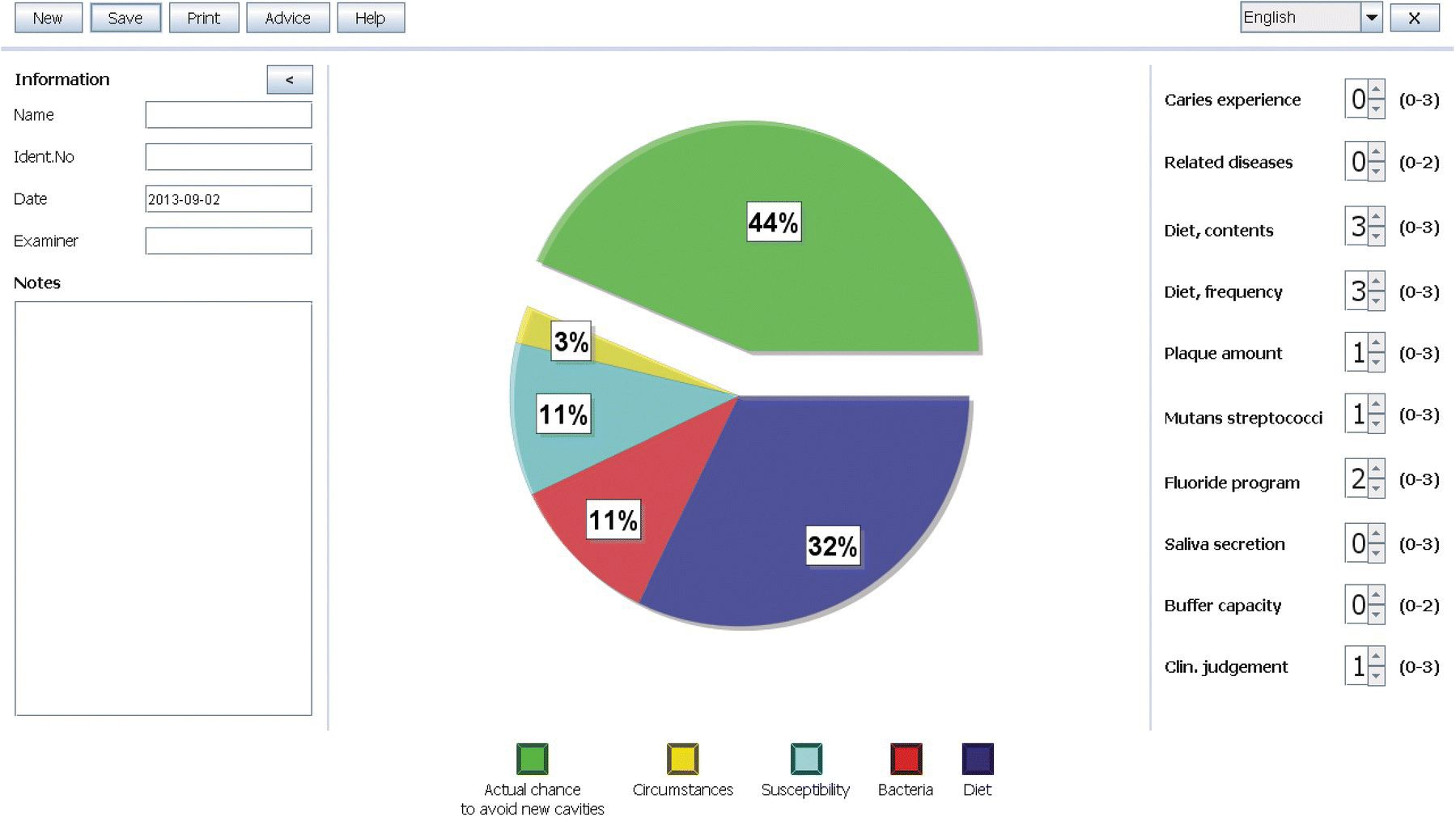
Figure 11.5 Caries risk assessment with Cariogram. Ten variables are computed and the program indicates a 44% chance of avoiding new caries lesions in the near future (green sector). The blue sector indicates that high sugar amounts and frequent intakes are the main contributing factor in this case. Targeted preventive measures linked to the individual caries risk profile are suggested. The program is available in several languages at www.mah.se.
Methods for caries prevention
Collaboration and interaction
In order to prevent, reverse, or slow down caries lesions, one or several of the following factors have to be utilized or altered: topical application of fluoride, diet, oral hygiene, and fissure sealants.
There are both local and general interventions. Remineralization with fluorides or fissure sealants are examples of local treatments. General intervention or behavior change interventions are strategies to enable the patient to control his own risk factors. The method is to inform about the disease and risk factors and to improve the patient’s oral health knowledge, attitudes, and behaviors. It must, however, be emphasized that the factors should not be looked on as separate entities but as highly interactive. For example, good oral hygiene enhances the effect of topical fluoride applications.
Especially in young individuals, the cooperation, the knowledge, and the capability of the parents and the child are important factors for the outcome of the preventive measures. In Figure 11.6 three different results of preventive activities on caries progression are presented where the parental cooperation was determinant.

Figure 11.6 Caries progression. (a) An 11‐month‐old girl exposed to frequent intakes of stewed fruits. The parents could not change the diet. (b) One year later the incisors had to be extracted. (c) A 4‐year‐old boy with developing initial caries lesions. Good parental cooperation. (d) Status after 1 year shows no progression of the caries lesions. (e) A 6‐year‐old boy with active caries. Intense prophylaxis. (f) Status 1 year later shows complete control of caries progression.
Many interventions related to child dental health aim to reduce caries by encouraging the establishment and maintenance of favorable oral health routines as these behaviors, once established, can endure throughout adulthood and provide lifelong protection against caries. These interventions can be performed in different arenas such as child health centers, dental clinics, and schools. The approach should be health promoting and deal with the conditions of oral health and not only the causes of diseases.
Attitudes, appraisals, and cooperation as well as social, ethnic, and economic circumstances in the family may act as barriers or facilitators for implementation of interventions. Limitations to assimilate information due to language problems are important for the compliance with interventions. Additionally, parents’ habits have impact on child behavior, particularly through modeling actions. Also parents’ perception of their own ability to deliver the behavior desired for dental health of the child, i.e., regular toothbrushing (self‐efficacy), may have a significant impact on child dental health. Parental cultural beliefs and influences, the parent’s level of autonomy in decision‐making within the family, coping skills and supportive networks, as well as parents’ past dental experiences are important for their self‐efficacy.
Behavior change interventions
Motivational interviewing (MI) is a technique for behavior change interventions defined by Miller and Rollnick in 2002 [12]. It is an individually tailored conversation technique for strengthening a person’s own motivation and commitment to change habits. The technique aims to strengthen the motivation for and movement toward a specific goal by eliciting and exploring the person’s own reasons for change within an atmosphere of acceptance and compassion. The principle of MI is to try to understand through an empathetic and reflective listening and not argue when the patient does not see any reason to change, but instead try to understand why and strengthen the patient’s belief in his own ability and the possibility of change. The therapists should help the patient to articulate his own understanding of his problems, his own arguments for changes, and to strengthen his determination and commitment to implement the change. The effectiveness of MI at improving oral health is still, however, inconclusive according to a recent systematic review [13].
Topical application of fluoride
Topical fluoride application is one of the most effective ways of preventing caries. Numerous clinical studies have been performed over the last few decades. Although the trials differ concerning sample size, age of the children, diagnostic criteria, caries activity, and methods of fluoride application, there is, without doubt, documentation for a considerable caries‐reducing effect of topical fluoride application. For detailed information the reader is referred to specialist textbooks and reviews on the use of fluoride in dentistry (Box 11.4). Generally, there is one important basic principle to obtain a good effect: apply fluoride in such a way that fluoride is present at the plaque/enamel interface where it will control dissolution and stimulate precipitation of minerals during caries challenges. This can be achieved by frequent application of low concentration fluoride solutions or preparations, or less frequent application of high fluoride concentration preparations causing fluoride deposits in or on the enamel that will slowly be released to the plaque–enamel interface. As a general rule the fluoride should match the caries activity of the child; that is, the greater the cariogenic challenge, the more intense the fluoride treatment.

VIDEdental - Online dental courses


