10 The Healthy Dental Practice: Infection Control and Mercury Safety
INFECTION CONTROL
Of course, HIV infection is not the only infectious disease to raise concerns about cross-infection during dental treatment. HBV infection is an ominous threat, and the risk of HBV infection is higher in the unprotected dental practice setting than in most other environments. Hepatitis B was around long before HIV infection, but it took the impact of HIV infection to force adoption of those old-fashioned barrier techniques of infection control that had never been a routine part of dental practice.
Guidelines for Infection Control
The American Dental Association (ADA) had a set of rather gentle infection-control guidelines in the pre-HIV era,13 mostly concerned with hepatitis, but the advent of HIV in the early 1980s led to a more stringent approach. Detailed guidelines were then developed by the ADA,16 and the American Association of Public Health Dentistry produced its guidelines in 1986.4 The definitive guidelines for dental practice, however, are those issued by the U.S. Public Health Service’s Centers for Disease Control and Prevention (CDC). These definitive guidelines were first issued in 1993,103 and the updated and considerably extended version was released in late 2003 after extensive public comments.104 The CDC has also developed infection control guidelines for field examinations for surveys or research studies.98 The ADA has now merged its statement on infection control with the CDC guidelines.
All of these guidelines are based on the concept of standard precautions (previously called universal precautions). The underlying philosophy is that infected patients cannot be differentiated from uninfected ones, so the prudent thing to do is to assume that all patients may be infected. A parallel approach, first presented in 1987,65 is referred to as body substance isolation, which focuses on reducing transmission of infectious material from any moist body substance of the patient to the health care worker. Both approaches emphasize that barrier procedures should be employed in treating all patients, which means that gloves, masks, and protective eyewear should be worn by dental personnel. They also focus on proper disposal of one-time-use materials, routine sterilization of other instruments and equipment, and proper handling of potentially infectious materials. The 2003 CDC guidelines moved toward combining the previous universal precautions regarding body substance isolation into a single set of recommendations known as standard infection-control procedures.70 Each recommendation in these guidelines is graded according to the strength of the scientific evidence to support it.
The barrier principles that form the basis of the CDC guidelines hark back to the beginnings of antiseptic medical practice, and they are effective: HBV infection was found to be twice as high among dentists who never wore gloves as among dentists who wore gloves routinely.48 With standard precautions, the risk of transmission of either HIV or HBV in the dental office is extremely low.29
OSHA and Dental Practice
Dentists, like all other employers, are subject to occupational health and safety laws and regulations that cover a variety of activities in the dental office. Although OSHA’s interests include a wide range of issues like ergonomics, waterlines, and indoor air quality, the OSHA regulation that has most affected dental practitioners is the bloodborne pathogen (BP) standard. This standard came into effect in March 1992 after a period of intense public debate in which the ADA played a prominent role. The BP standard was revised in January 2001.102 It applies to all activities in which health care workers come into contact with human blood or other bodily fluids, or are in a position where they may do so. The BP standard applies to hospitals and other medical facilities, paramedical and ambulance services, blood banks, research facilities, and of course dental offices. The BP standard is comprehensive and highly detailed. It requires each dental office to prepare an exposure control plan, which is intended to minimize employee exposure to infection. The BP standard covers instrument sterilization and storage, handling of potentially contaminated equipment, disposal of medical waste, and many related topics. It specifies that dentists must offer HBV vaccination to staff and includes meticulous requirements for reporting “incidents,” that is, accidents in which skin has been broken (e.g., a needlestick) and hence in which there is potential risk of infection. Details get down to the level of washing and storing laundry.
For dentists unaccustomed to reading the language of the federal government, the BP standard is a formidable document. To help practitioners meet the standards, the ADA has a set of manuals that outline the elements of an exposure control plan and put infection-control guidelines together with OSHA guidelines in standard operating routines for the dental office.5
Dentists have also complained about the high cost of compliance with OSHA standards,32 sometimes implying that these are dollars not well spent. Some of the more trivial aspects of the BP standard have been refined over time, which should have the effect of reducing costs, but compliance will always carry some price. In the long run it is patients who foot the bill, and so far the public seems to view the cost of compliance as money well spent.
HIV INFECTION AND AIDS
AIDS is the acronym for acquired immunodeficiency syndrome and is the end point of HIV infection. With the dominant position this condition now occupies in the lives of all health professionals, it is sobering to recall that HIV was identified only in 1983.76 The knowledge that has accumulated since then on the virology and epidemiology of the condition represents some impressive research, although the public hysteria that can surround AIDS is a reminder that humans have not fundamentally changed much since the Black Death in the fourteenth century.
The AIDS virus is human T-lymphotropic virus type 3 or lymphadenopathy-associated virus, a retrovirus usually called HIV. It attacks the CD4+ T lymphocytes in infected humans, which results in immunosuppression. As the number of CD4+ T lymphocytes is reduced, the affected patient becomes increasingly vulnerable to opportunistic infections, which can overwhelm the patient’s compromised defense systems. Pneumocystis carinii pneumonia is the most common serious opportunistic infection, though there are many others, including pulmonary tuberculosis. AIDS was at first defined solely by clinical conditions, but a 1993 revision of the classification system by the CDC redefined the stages of HIV infection in terms of three ranges of CD4+ T-lymphocyte counts and three groups of clinical manifestations, set out in a nine-cell matrix.25 These nine categories range from asymptomatic HIV infection or persistent generalized lymphadenopathy with a CD4+ T-cell count of 500/μl or more at the mild end of the scale, to the diagnosis of 1 of 25 AIDS-indicator clinical conditions plus a CD4+ T-cell count of 200/μl or less at the severe end. Dentally related conditions listed among the clinical diseases that are considered part of the AIDS diagnosis include oropharyngeal candidiasis, oral hairy leukoplakia, chronic herpes simplex, and Kaposi’s sarcoma.
The disease we call AIDS is the “finale in a progressive process of immunologic deficit mediated by the virus.”76 The primary epidemiology of HIV infection has been well described in terms of risk factors and modes of transmission, although research is still needed on the dynamics of transmission and infection. The average time between infection with HIV virus and the onset of AIDS-like symptoms is estimated to be 10 years,76 so that HIV disease is like a “time bomb.” HIV infection is diagnosed when results of a serologic test are positive; the condition becomes AIDS when a low CD4+ count is found in combination with one of the AIDS-indicator clinical conditions.
The principal mode of transmission in North America is homosexual contact among men followed by intravenous drug injection with contaminated needles and heterosexual contact.106 There are a small number of cases in which transmission has occurred perinatally (i.e., birth of an infant to an infected mother) and from transfusion with infected blood (e.g., as with the late tennis player Arthur Ashe in the early 1990s). The principal mode of transmission in poor countries is heterosexual contact. Despite the publicity given to the risk associated with certain sexual and drug-use activities, behavioral change among the highest-risk groups does not come easily. The epidemic is increasingly affecting women, minorities, the poor, and heterosexual persons.55
In the early days of the AIDS epidemic in North America, diagnosis with HIV infection meant virtually certain death within a few years. Drug therapy developed quickly, and protease inhibitors showed some good effects. A few years later treatment evolved into the “cocktail” of antiretroviral drugs known as highly active antiretroviral therapy (HAART), which greatly extended life expectancy and has allowed many HIV-positive persons to live more or less normal lives. HAART has probably reduced much of the fear that surrounded HIV infection a generation ago, which may or may not be a good thing. In any event, the success of HAART should not blind us to the fact that AIDS is a pandemic, a global epidemic of massive proportions that is devastating a number of poor countries. HAART is far too expensive to be used widely in these poor countries at market prices. Box 10-1, which shows some of the global data for 2002, indicates the enormity of the HIV pandemic.
BOX 10-1 Global Extent of AIDS/HIV Infection in December 2002118
Figures for the United States are not as mind boggling as the global data but still tell us that AIDS is a major epidemic.106 At the end of 2002, there had been 501,669 deaths from AIDS in the United States, including 5315 children under age 15. The death count had increased 39% over 6 years. The cumulative number of cases reported since the beginning of the epidemic in the United States was 886,575. The number of adults and adolescents living with AIDS was 384,906, an increase of 73% over a 6-year period. No one knows how many people are infected with HIV who have not yet been diagnosed, but it is likely to be over a million. It is because of this large number of undiagnosed HIV carriers that the estimates of the growth of the epidemic are ominous. Development of successful vaccines is not considered likely, and HAART treatment is expensive, so control of the epidemic falls back on the toughest measure of all: education to control risky human behavior.
AIDS presents some paradoxes. For example, despite the “time-bomb” implications of the extent of current infection and thus the near certainty of the continued growth of the epidemic, the responsible virus is really quite delicate and hard to transmit. Although dental professionals are at relatively greater risk than average members of the public because of their close contact with saliva and blood, they still have an extremely low risk of occupational exposure.56 A small number of health care workers have become HIV infected through occupational exposure, but the risk of seroconversion even after needlestick exposure to HIV-infected blood is still only about 1 in 200.111
A possible case of HIV transmission from an infected dentist in Florida to a patient was reported in 1990; the dentist died soon after the patient was diagnosed. In this case the patient had two maxillary third molars removed by the dentist. She reported pharyngitis 4 months later and had oral candidiasis 17 months later. Two years after the extractions, she was seropositive for HIV antibody and was diagnosed with P. carinii pneumonia. The dentist was reported to have worn gloves and mask throughout the procedure, and from the patient’s statement there was no evidence of exposure to the dentist’s blood. There were similar DNA sequences in peripheral blood mononuclear cells of both dentist and patient, like those found in many cases that have been epidemiologically linked. Soon afterward, evidence emerged that eight other patients treated in this practice were HIV infected, and there were strong indications that the dentist was the source of infection for at least five of them.26 The ADA responded quickly to this disclosure in early 1991 with an interim policy that HIV-infected dentists should not perform invasive procedures or should disclose their seropositive status to their patients.69 The CDC closed the case in 1992 without being able to reach firm conclusions about whether the dentist infected his patients.
Since then, the CDC has issued guidelines that place some limitations on HIV-infected practitioners, mostly restricting the performance of major invasive procedures. Some states have a legal requirement that an HIV-infected practitioner disclose this status to the patient, although usually this does not mean that the practitioner is not permitted to perform a given procedure.11 Again, it can be seen that the basis for these requirements is the effectiveness of the standard precautions.
Oral Manifestations of HIV Infection
All dental professionals should be thoroughly familiar with the oral manifestations of HIV infection. The principal signs are oral candidiasis, oral hairy leukoplakia, and Kaposi’s sarcoma, although periodontal conditions are frequently bad in persons with advanced immunosuppression117 and a number of less common disease entities are also found.89 The details of these conditions are covered thoroughly in oral pathology texts50 and workshop proceedings.81 The three principal signs are described only briefly here.
The particularly distressing condition of pediatric AIDS, in which HIV is transmitted from an infected mother, appears to be on the increase. Recognition can be difficult because of the varied presentation of the condition, but the most common oral findings include candidiasis, parotid salivary gland enlargement, and herpetic infections.94
HEPATITIS B AND C
Hepatitis is a far more prevalent disease than HIV, both worldwide and in the United States. The CDC estimates that 45% of the world’s population live in areas of high prevalence, 43% in areas of moderate prevalence, and only 12% in areas of low prevalence.107 Globally, the World Health Organization estimates that 2 billion people have been infected with HBV and that currently some 350 million people have chronic infection.119 In poor countries, 8%-10% of the total population is chronically infected, and in these regions liver cancer, a result of chronic HBV infection, is among the top three causes of death in men.119 By contrast, fewer than 1% of the population in high-income countries is chronically infected.
The United States and other high-income nations are areas of low prevalence, although there are still around 80,000 new infections per year in the United States.108 Hepatitis B is primarily a disease of young adults in the United States (peak age for new infections is 20-29 years), whereas in poor countries it is a childhood disease. Both HBV and HCV are transmitted by contact with infected blood, so the primary transmission routes are:
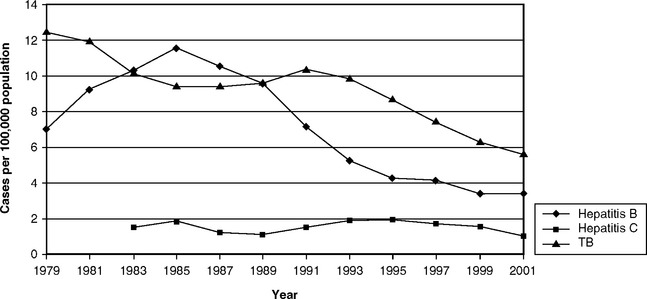
Although the case fatality rate from HBV infection is low (0.5%-1%) and most infected people recover completely in due course, a significant number of people develop chronic infection. It is in these chronically infected people that the most serious sequelae are found. HBV carriers are at risk of long-term sequelae such as chronic liver disease, cirrhosis, and liver cancer, though a more common outcome than death is severe and usually lifelong debilitation. The risk of becoming a chronic carrier of HBV varies with age at first infection. Among those first infected as young children, 30%-90% develop chronic infection, whereas among those who were adults when first infected only 2%-10% do. Chronic infection can be asymptomatic, but 15%-25% of this group can die prematurely from cirrhosis or liver cancer. The CDC estimates that there are some 150 deaths per year from acute hepatitis, although there are around 5000 deaths each year from chronic liver disease. Although the good news is that the number of new infections has been dropping in recent years (Fig. 10-1), the bad news is that there are still 1.25 million persons chronically infected with HBV and 2.7 million HCV-infected persons in the United States.108
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses