10
Temporomandibular Joint Surgery
INTRODUCTION
Temporomandibular joint surgery (TMJ) including noninvasive and invasive procedures such as arthrocentesis, arthroscopy, and open joint arthroplasty, like all other types of surgery, can result in complications.1 While it is not the intent of this chapter, it should be mentioned that nonsurgical therapy, such as bite splint therapy for myofascial pain or internal derangement, may result in complications such as malocclusion. The complications of managing the TMJ patient may be either transient and self-limiting, or long term and irreversible in nature.
For successful TMJ surgery, operative intervention should be reserved for cases where the source of pain and/or dysfunction is the TMJ apparatus itself and, in addition, following a trial of conservative or nonsurgical treatment. Distinction between myofascial and intracapsular pathology is crucial. Concomitant neurologic and psychiatric conditions should be adequately treated beforehand as well.
Appropriate decision making has proven to be difficult with respect to TMJ surgery because of the lack of support from well-designed, randomized, clinical trials. Most of the treatment algorithms are based on the assumption that most TMJ disorders are self-limited or managed with nonsurgical modalities.2 On the contrary, surgical intervention should not always be considered last resort, as in conditions such as severe ankylosis, tumors, and recurrent dislocation.2 Progress in our comprehension of molecular, cellular, and biochemical mechanisms has given surgeons the ability to better select the appropriate surgical intervention.2
It is also important that the patient’s expectations are realistic for a successful outcome. Reasonable expectations from TMJ surgery may include: (1) a postoperative interincisal opening of 30 to 35 mm; (2) pain reductions of 50% to 70%; and (3) 60% to 70% or normal dietary function.3 The goal of this chapter is to discuss commonly encountered complications associated with TMJ surgery and their management.
VASCULAR INJURY
Vascular injury can occur during arthroscopy or open joint surgery. The blood vessels that are most susceptible to injury during TMJ surgery include the branches of the external carotid artery, most commonly the superficial temporal artery and the internal maxillary artery, and the pterygoid plexus of veins. Rarely, injury to the middle meningeal artery can occur with inadvertent penetration into the middle cranial fossa. Because of the extensive collateralization of the vasculature in the head and neck, adequate tissue perfusion following injury is not compromised.
Punctures or lacerations to these vessels can result in obstruction in visualization of the surgical field and must be controlled to prevent potentially life-threatening hemorrhage. Some degree of bleeding is existent during most arthroscopic and open joint procedures. Control of hemorrhage includes direct pressure, ligation, electrocautery, laser ablation, local anesthetics with epinephrine, and embolization. Ensuring hemostasis prior to closure in arthrotomy and evacuation of blood clots in arthroscopy is essential to avoid hematoma formation, which can lead to infection and the risk for adhesions formation and potential ankylosis.
Goss and Bosanquet reported three cases of bleeding from branches of the superficial temporal artery in 50 arthroscopies.4 In a cadaveric study, Westesson et al. demonstrated the close proximity of the superficial temporal vessels to the site of the arthroscopic cannula system insertion.5 Bleeding from the superficial temporal vessels during arthroscopy can generally be avoided by palpation prior to puncture and with employment of anatomic landmarks for joint entry.6
During arthroplasty, branches of the superficial temporal vessels, which are identified during the dissection, can be prophylactically ligated and divided without compromising tissue perfusion because of the vast collateral circulation of the vasculature in the head and neck. On the other hand, injury to the superficial temporal vessels can be avoided by using the flap to retract them anteriorly, during a standard preauricular approach to the TMJ.
Hemorrhage from the internal maxillary artery can arise and be potentially life threatening.7 Hemostasis following an injury to the internal maxillary artery is challenging due to limited access and visibility of the surgical site. It crosses medial to the condylar neck and sigmoid notch and has been found to be on average 20 mm below the head of the condyle.8 Blind instrumentation in this area may result in damage to the internal maxillary artery and subsequent hemorrhage. If the injury occurs during condylectomy, the osteotomy should be completed in order to assist in direct visualization of the bleed. Upon discovery of the site of injury, the vessel, depending on its size, can be clamped, then ligated or cauterized. If the bleed cannot be pinpointed or access to it is limited, then the wound should be packed and direct pressure accomplished. Various hemostatic agents can also be used including thrombin-soaked sponges, gelatin sponges (Gelfoam®), microfibrillar collagen (Avitene®), fibrin matrix spray (Tiseel®), and oxidized cellulose (Surgicel®). Flo-Seal Hemostatic Matrix Sealant®, a bovine collagen-derived gelatin matrix consisting of cross-linked granules with topical human-derived thrombin has also been effective.9 If usual attempts in hemostasis have failed, then more invasive measures should be undertaken.
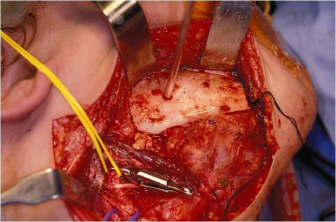
In total joint replacement surgery, the neck incision should precede the condylectomy so that external carotid artery ligation just distal to common carotid bifurcation can be quickly accomplished, hence halting blood flow to its branches in the event of uncontrollable hemorrhage (Figs. 10.1 and 10.2). However, multiple ligation sites have been found to be more effective since they reduce collateral blood flow.10 In an animal study, the effectiveness of ligation of the external carotid artery and its major branches, in the control of hemorrhage from the internal maxillary artery, was evaluated.7 From their findings, the authors concluded that hemorrhage from the internal maxillary artery is most successfully managed with ligation of the external carotid artery in the retromandibular fossa, distal to the origin of the posterior auricular artery, in addition to ligation of the superficial temporal artery at the root of the zygoma.7
Fig. 10.1. External carotid artery ligation above the posterior auricular branch and below the transverse facial is used to control hemorrhage following injury to the maxillary artery and its branches.
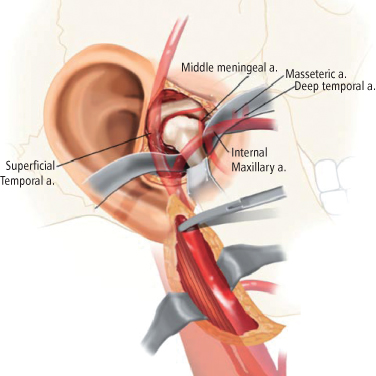
Fig. 10.2. Retromandibular approach for vascular control.
The ability to access a vessel closer to the area of injury decreases the risk of the collateral blood supply that would otherwise contribute to perfusion. Angiography and selective embolization via percutaneous femoral artery cannulation following hemorrhage in TMJ surgery has been reported.11 The Seldinger technique under fluoroscopic guidance is used to access the offending branch. A thrombus-inducing material is then introduced into the lumen of the vessel so that it is occluded and blood flow ceases. A variety of agents have been used including methylmethacrylate spheres, balloon catheters, cyanoacrylate tissue adhesives, gelatin sponges, polyvinyl alcohol sponges, silicone spheres, cotton, wool, stainless steel coils, and autologous blood and muscle.12
Potential complications, even though rare, can occur with arterial embolization, and include vasospasm, hemorrhage, dissecting aneurysm formation, infection, skin necrosis, cranial nerve injury, and inadvertent internal carotid artery cannulation or reflux with subsequent cerebrovascular accident (CVA) or death.12 The risk of permanent neurological complications with embolization is generally l%.11
Pseudoaneurysm of the superficial temporal artery following arthroscopy has been reported.13 A pseudoaneurysm, also known as a false aneurysm, is a leakage of blood from a disrupted artery into the surrounding tissue, forming a hematoma. The hematoma is contained by the surrounding tissues and continues to communicate with the artery. On physical examination, a thrill or a bruit is appreciated. Definitive diagnosis can be made with angiography or magnetic resonance angiography (MRA). Surgical exploration, with vessel isolation, ligation and excision or arterial embolization can be used to treat pseudoaneurysms.
Moses and Topper reported an arterio–venous (A–V) fistula between the right superficial temporal artery and vein following arthroscopy. At a subsequent operation, the A–V fistula was isolated and ligated with 3-0 silk sutures. At the 6-month follow-up, there was no evidence of vascular malformation.14
NERVE INJURY
Injury to the branches of cranial nerves V and VII can take place in TMJ surgery. Arthroscopy is less likely than arthrotomy to cause permanent malfunction manifesting as an interference with facial expression and cosmetic deformity. The reported incidence of facial nerve injury following TMJ surgery ranges from 1% to 25% and is typically transient in nature, resolving within 3 to 6 months.1 Causes of neuropraxia include edema, excessive flap retraction forces, electrocautery, inadvertent suture ligation, or clamping of tissues.
Surgical approaches to the TMJ have been designed to afford the most protection to the facial nerve. Regardless of the surgical approach that is utilized, facial nerve injury is always a risk. To prevent disruption of the branches of the facial nerve requires a comprehensive knowledge of the anatomy and meticulous surgical dissection. Factors that can increase the risk of nerve damage include use of improper surgical technique or abnormal joint anatomy as a result of a congenital abnormality, trauma, tumor or multiple previous surgeries.
The four basic incisions in TMJ surgery include the preauricular, the endaural, the postauricular, and the submandibular.15 The incidence of nerve injury has been found to increase when a separate skin flap is raised.16 During arthroscopy, a rotational versus a straight motion with insertion of the trocar and cannula is more likely to divert any nerves.6
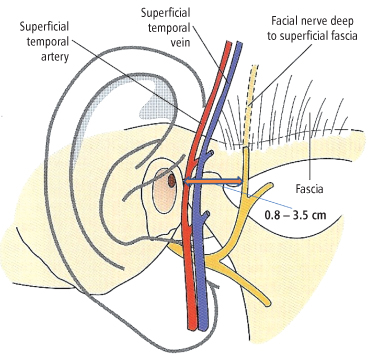
The temporal and then the zygomatic branches of the facial nerve are most prone to injury, presenting, respectively, as a loss of ability to raise one’s eyebrows, wrinkle one’s forehead, or close one’s eyes completely (Fig. 10.3). These branches cross the zygomatic arch in their course within the dense, inseparable fusion of the periosteum, temporalis fascia, and the temporoparietal fascia. From their classic cadaveric study, Al-Kayat and Bramley discovered that this dangerous area of fusion was on an average of 2.0 cm (range: 0.8–3.5 cm) from the anterior concavity of the external auditory meatus (Fig. 10.4).17 Therefore, a vertical incision made over the zygomatic arch that is less than 0.8 cm from the anterior concavity of the external auditory meatus allows safe entry into the joint. Furthermore, the inadequacy of the superficial muscular aponeurotic system (SMAS) at the lateral border of the frontalis muscle leaves the temporal branches susceptible to injury.
Fig. 10.3. Paresis of the right temporal and zygomatic branch of the facial nerve (CN VII). Inability to wrinkle forehead and raise eyebrow (top) and close eye (bottom) following injury to the temporal and zygomatic branches of the facial nerve (CN VII).
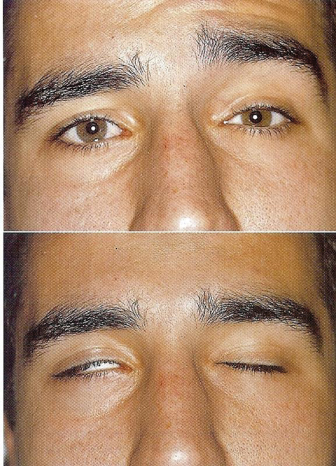
Fig. 10.4. The danger zone of fusion where the facial nerve (CN VII) is most prone to injury is where the upper division of the facial nerve crosses the zygomatic arch 0.8 to 3.5 cm from the anterior concavity of the external auditory meatus.17
Rudolph illustrated in his cadaveric facelift dissections that the facial nerve branches are deepest, or absent, behind the ear, inferior to the zygoma, and near the earlobe, and that the precarious area, where the temporal branches become superficial, is 5 cm from the parotid border and 2.3 cm ± 0.6 mm deep.18 Conversely, the zygomatic branch was found to be well protected in the facial fat upon exiting from the parotid gland, and it also has many anastomoses between its branches.18
Fortunately, in the majority of the proposed branching patterns of the facial nerve, there is distal branching that allows for multiple points of innervation of the frontalis muscle. Therefore, Hall et al. hypothesized that the most distal branch of the facial nerve that crosses the zygomatic arch could be transected 63% of the time without frontalis dysfunction.19
In the patient who has been operated on multiple times, definable surgical planes that make for safe dissection may not be present secondary to scarring. In these cases, the dissection should be carried out to the level of the temporalis muscle.20
In patients with facial nerve injury following TMJ surgery, it is necessary to assess the affected area and the degree of the deficit. In patients who have brow or forehead weakness, no immediate intervention is typically necessary. Postoperative measures for management of inadequate eyelid closure include use of artificial tears and ocular lubricant with taping of the eye at bedtime in order to prevent corneal desiccation and keratitis. Conservative treatment with exercises or electrical stimulation may be helpful. Should nerve function fail to return, depending on the affected branches, microneurosurgical repair can be considered. Botulinum toxin A injections to the corresponding muscles of facial expression on the opposite side can be used to mask the deficit. A gold weight implanted into the upper eyelid can also be used to manage permanent insufficient eyelid closure.
Injury to the trigeminal nerve branches (the infraorbital nerve, the inferior alveolar nerve, the lingual nerve, and the auriculotemporal nerve) is less common in TMJ surgery. Extravasation of irrigation fluid can cause paresthesia in the affected branch. In these cases, resolution is rapid without sequelae. More serious injury to the inferior alveolar nerve can occur from instruments used to clamp the mandible in order to distract the condyle inferiorly. It can also be damaged during condylectomy, or screw placement used to fixate mandibular implants, in TMJ replacement surgery. The prognosis for recovery from these injuries is less predictable.
The auriculotemporal nerve travels alongside the superficial temporal vessels commonly encountered with a standard preauricular approach to the TMJ. It is a mixed nerve and carries both sympathetic and parasympathetic nerve fibers. Auriculotemporal nerve injuries were found to represent 59% of all neurologic injuries during TMJ arthroscopy.21 Dolwick et al. found that in 56 patients who had undergone TMJ arthrotomy via a preauricular approach, all had subsequent paresthesia associated with the auriculotemporal nerve.22 However, its occurrence is most often temporary.
Auriculotemporal nerve syndrome, otherwise known as Frey’s syndrome, is a gustatory sweating, flushing, and warmth over the distribution of the auriculotemporal nerve and/or the greater auricular nerve during mastication of foods that are potent stimulants of saliva. It is believed to result from the misdirected regeneration of injured parasympathetic fibers to the eccrine sweat glands in the skin. Frey’s syndrome is an unlikely complication of TMJ surgery, and a small incision without an oblique superior extension may further decrease the risk.23 Kryshtalsky and Weinberg reported that 3 of 20 patients (15%) developed Frey’s syndrome following open TMJ surgery in which a preauricular approach was utilized.24
A Minor’s starch-iodine test can be used to diagnose Frey’s syndrome.24 A solution of 3 g of iodine, 20 g of castor oil, and 200 ml of absolute alcohol is applied. The region is then lightly dusted with starch powder. The patient is instructed to chew on a lemon drop for 4 minutes. A positive result occurs when sweat dissolves the starch powder and reacts with the iodine to produce a dark blue discoloration. A negative result occurs when there is no color change.
Treatment of Frey’s syndrome includes topical application of anticholinergic compounds, such as glycopyrolate, transection of the auriculotemporal nerve, or implantation of freeze-dried dura or fascia lata under the skin of the involved area.25
INFECTION
Postsurgical infections in TMJ surgeries when an implant is not placed occur infrequently. There are few case reports of postarthroscopic infections, including otitis media,26 joint infection,27,28 and infratemporal space infection.29
Forty-four out of 2,106 (2.09%) patients and 44 of 3,285(1.34%) implants had an infection following TMJ reconstruction with the TMJ Concepts® system. With total TMJ replacement, immediate infection of the components is atypical. Late infection can occur and is as/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


