10
Space planning for the dentition (space analysis)
INTRODUCTION
One way of viewing the clinical practice of orthodontics is to see it as the redistribution of space with, in addition, provision for the impact of growth in children and adolescents. In a majority of patients, where the skeletal elements are not particularly adverse, ideal positioning of the teeth is a reasonable expectation. However, an understanding of the available space is critical to orthodontic planning if the objectives are to be achieved. Various analyses have been described that measure one or more aspects of a malocclusion that impact on space1,2 but these offer only part of the information required to analyse space or are tied to specific techniques.3 By contrast, a space planning system used in the permanent dentition has been developed at the Royal London Hospital4,5 over many years, which allows for all the factors which can contribute to space distribution (Box 10.1).
Box 10.1 Benefits of comprehensive space planning
- A disciplined approach to treatment planning
- Defining whether the objectives are attainable
- Anticipating shortage of anchorage or excess of space
- Identifying whether extractions are necessary
- Planning the mechanics of anchorage
- Planning the mechanics of arch relationship correction
- Improving pretreatment patient information
- Obtaining valid informed consent
Apart form achieving the six keys of ideal occlusion,6 the dentition should be placed in an ideal position in the face in all three planes. However, the requirements of aesthetics may conflict with the requirements for stability, and therefore the space planning exercise for any individual is inextricably linked with the treatment objectives. Thus, space planning needs to be used in a flexible manner to allow for various treatment options to be explored. For example, while it may be necessary in some patients to achieve aesthetic objectives by tooth movements that are potentially unstable, space planning can identify the need to obtain patient consent for long-term retention.
ROYAL LONDON SPACE PLANNING
The space analysis system consists of two parts, the first identifying space requirements and, the second, the creation and utilisation of space. Both parts involve measurements of reference models and cephalograms, and incorporation of the space implications of treatment objectives and planning decisions.
Space Requirements
A shortage or consumption of space is recorded as a negative and a surplus or creation of space as a positive. There are fives factors to be considered in space requirement, the first three determined from the models and the other two based on the cephalogram. It is preferable to analyse each arch separately with the lower considered first as it is the template around which the upper arch is fitted. The only occlusal factor not assessed in the space requirements is the correction of the molar relationship, which is considered in the second part of the analysis (Table 10.1).
Table 10.1 Space requirements
| Lower | Upper | |
| Crowding and spacing | ___ mm | ___ mm |
| Levelling occlusal curve | ___ mm | ___ mm |
| Arch width change | ___ mm | ___ mm |
| Incisor A/P change | ___ mm | ___ mm |
| Inclination change | ___ mm | ___ mm |
| Total | ___ mm | ___ mm |
+ = space available or gained
− = space required or lost
A/P, anteroposterior.
Crowding and Spacing
Crowding can only be quantified in relation to an arch form, but this is not always obvious as the irregularity of the teeth can mean that more than one arch form could be used as a measuring reference. The simplest is to use an arch form passing through the majority of the buccal cusps and incisal tips (Figure 10.1). Individual teeth that do not lie on the arch form are easily identified. It is important to note that this arch form is used purely to quantify crowding and need not coincide with the intended post-treatment arch form as separate assessments will be made for arch width and labiolingual position of incisors.
Figure 10.1 The arch form selected for the assessment of crowding reflects the majority of teeth, not necessarily the most prominent central incisor.
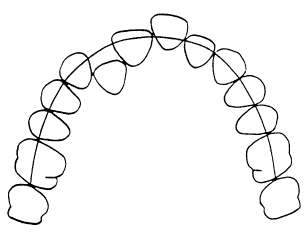
Teeth anterior to the first molars that do not lie on the selected arch form are measured mesiodistally using a clear ruler and crowding is calculated by subtracting the space available. The process is repeated for the upper arch. This method of assessing crowding has been shown to be accurate and repeatable.7 It is important to ensure that the incisors which contribute to the arch form are the same as those which are traced on the cephalogram and used to measure the overjet. In contrast, spacing is straightforward to measure as the alignment of the teeth in most cases is good and the process is simply one of adding up the spaces available for a (+) score of space.
Levelling of Occlusal Curve
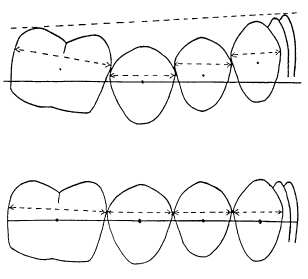
Generally, in the growing child, a small curve will exist between the lower first molars and the incisors (Figure 10.2). Provided the depth of curve is no more than a couple of millimetres, there is no need to make an allowance for space. A steeper curve, however, will have implications for the available space as there will be vertical contact point displacements. A level arch will produce the maximal space requirement with all the contact areas lined up. A curve of 3 or 4 mm, as measured against a flat plane from the distal cusps of the first molars to the incisal edges generally requires 1 mm of additional space to flatten the arch. Curves of 5 mm or more are likely to require 2 mm of space for the whole arch. The levelling of the second molars is not considered as this occurs as a process of distal movement8 and does not impact on space in the anterior or mid-arch segments.
Figure 10.2 Increased occlusal curves are due to slipped contacts in the vertical plane. Levelling the occlusal plane involves restoring the contact point relationships.
Arch Width Change
Posterior crossbites can be corrected by the contraction of one arch, expansion of the other, or a combination of both. It is necessary to identify any premature occlusal contacts and mandibular displacements, and to assess the shape and symmetry of the arches and whether any individual teeth are displaced. In terms of transverse arch relationship, the arch width between the tips of the mesiobuccal cusps of upper first molars should be 2 mm greater than the width between the buccal grooves of the lower molars. This can be determined by the use of dividers or by direct measurements with a ruler on the models. There is no evidence that more than 5 mm of expansion of the upper first molars can be achieved with a stable result. If the differential between the upper and lower intermolar widths is greater than 5 mm, a degree of lower arch contraction across the molars will be required if stable correction is to be achieved.
It has been shown in a number of studies that expansion also leads to a change of arch form with less widening across the premolars than across the first molars. The overall effect of 1 mm expansion across the upper intermolar width is the creation of 0.6 mm space.9–11 A 5 mm expansion of the upper intermolar width will result in approximately 3 mm additional space in the arch (5 × 0.6 = 3.0 mm). Similarly, contraction of the lower intermolar width will reduce the available space using the same formula. A space requirement to contract an arch will necessitate either enamel reduction, extraction or incisor protrusion.
Incisor Anteroposterior Position
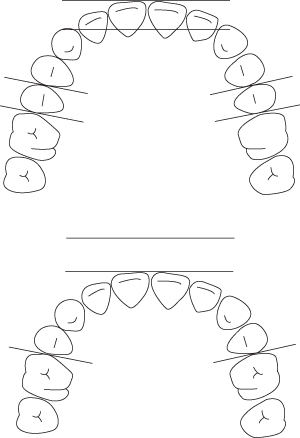
This requires cephalometric assessment. The treatment objective at the outset will determine whether the existing lower incisor position is acceptable. If a forward movement of the lower incisors is desired, for example in a Class II division 2 malocclusion, space will be created by this movement. If all four lower incisors are advanced by 1 mm, additional space will be created distal of the incisors by an equivalent amount on each side, totalling 2 mm space. Conversely, retraction of either the upper or lower incisors is a space requirement; a 1 mm retraction of all four incisors will require 2 mm space (see also Figure 10.3). It is essential that the incisors which are measured cephalometrically are the same incisors which are used for measurement of the overjet and for the assessment of the crowding or spacing when deciding on the arch form.
Figure 10.3 The retraction of incisors by a distance requires the same amount of space in each buccal segment. In the lower diagram, the inter-molar distance is equivalent to the distance between second premolars in the upper diagram.
Th/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


