Prosthodontic Considerations in the Implant Restoration of the Esthetic Zone
Ghadeer Thalji1 and Sandra Al‐Tarawneh2
1 University of Illinois at Chicago College of Dentistry, Chicago, Illinois, USA
2 University of Jordan, Amman, Jordan
The esthetic zone can be defined as any dentoalveolar segment that is visible upon full smile from an objective standpoint. Subjectively, it has been defined as any dentoalveolar area of esthetic importance to the patient.1 Unlike implant therapy in other segments of the oral cavity, implant treatment in the esthetic zone is one of the most intricate procedures in terms of creating harmonious gingival contours, and is often classified as advanced or complex according to the SAC classification.2 Therefore, esthetic risk assessment analysis and determination of patients’ expectations preoperatively are critical to successful implant therapy. Some of the challenging risk factors that make the case fall into the high‐risk category for esthetic results include:2–7
- high lip line (high smile line, revealing the total cervicoincisal length of the maxillary anterior teeth and a contiguous band of gingiva);
- highly scalloped thin gingival biotype (more prone for recession compared to flat thick biotype);
- triangular shape of tooth crown;
- acute infection at implant site;
- bone level at adjacent teeth more than 6 mm to the contact point, which makes interdental papillary fill very difficult, if not impossible;
- restored adjacent teeth;
- an edentulous space of two or more teeth;
- soft tissue defect;
- vertical bone deficiency;
- adjacent implant restoration (inadequate inter‐implant papilla);
- long junctional epithelium, low crest bony topography.
Esthetic risk factors should be recognized and explained to the patient before the initiation of implant therapy to avoid post‐treatment disappointment that can occur from unmet high expectations; patient expectations are higher with implant restorations than with conventional prostheses.8
Achieving predictable long‐term esthetics for an implant restoration requires a comprehensive multidisciplinary planning approach prior to surgical intervention and a restorative‐driven approach. Patients’ preoperative evaluation should include a comprehensive medical and dental history, diagnostic casts, photographs, site analysis, wax‐up, and the necessary radiographs, which may include cone‐beam computed tomography (CBCT) and virtual planning using suitable software. When a CBCT is selected, proper execution of the treatment plan is carried out through transfer of the virtual plan into real life through the surgical guide, and manipulation of the soft tissue architecture with the use of a properly designed interim restoration and, finally, the definitive restoration.
Adjunctive therapy, including orthodontics, additional restorative procedures, hard/soft tissue augmentation procedures, and/or periodontal therapy, should be considered and discussed with patients to optimize final treatment outcomes.
Examination and site analysis
A comprehensive evaluation of the site of interest is crucial and can provide a coherent guidance system for dental esthetics. A checklist for site analysis in the esthetic zone is included in Box 10.1.1,9–14
Diagnostic wax‐up, radiographic guide fabrication, and three‐dimensional imaging/virtual planning
Clinicians’ objectives should be targeted to achieving predictable outcomes in the short and long term that respect the biological, functional, and esthetic requirements.15 Ultimately, the desired tooth position must be the guide for final implant position. After performing a diagnostic wax‐up that determines the position of the proposed gingival zenith (as it represents the most apical part of the clinical crown),9,10 a radiographic guide can be fabricated and a CBCT obtained with the radiographic guide in place, if a three‐dimensional (3‐D) scan is deemed necessary. This allows the proposed position of the definitive restoration to be related to the surrounding soft tissues and underlying bone. A decision can then be made whether the available bone foundation is sufficient or augmentation procedures will be needed (Figures 10.1 and 10.2). Ideally, a minimum of 2 mm of facial bone thickness is needed once the implant osteotomy has been prepared to minimize facial bone loss and consequent peri‐implant soft tissue recession.16 Grafting should be considered to obtain this amount of bone in cases where there was a deficiency upon site evaluation. Virtual planning may be followed by fabrication of CAD/CAM implant surgical guides which may enhance accuracy of implant placement (Figure 10.3). The use of surgical templates is of great importance for proper implant positioning.

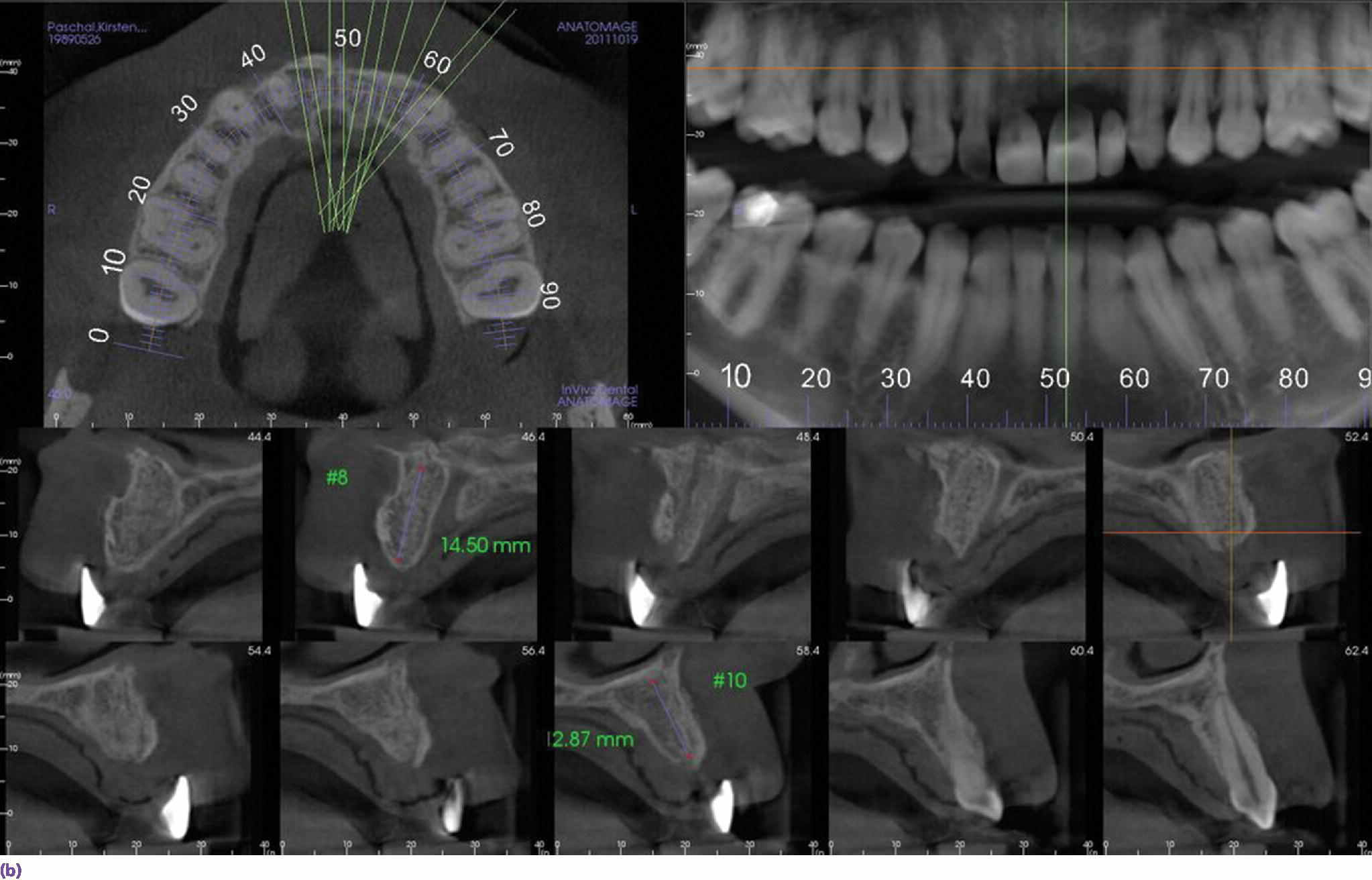
Figure 10.1 (a) Radiographic guide fabricated using radiopaque teeth tried intraorally prior to obtaining CBCT. GC resin occlusal jig in place to allow separation of teeth and stabilize the patient during the process. (b) Sagittal section through site #9 shows the exact relation of the proposed final restoration position to the available bone bed demonstrating availability of bone for proper 3‐D positioning of the fixture.
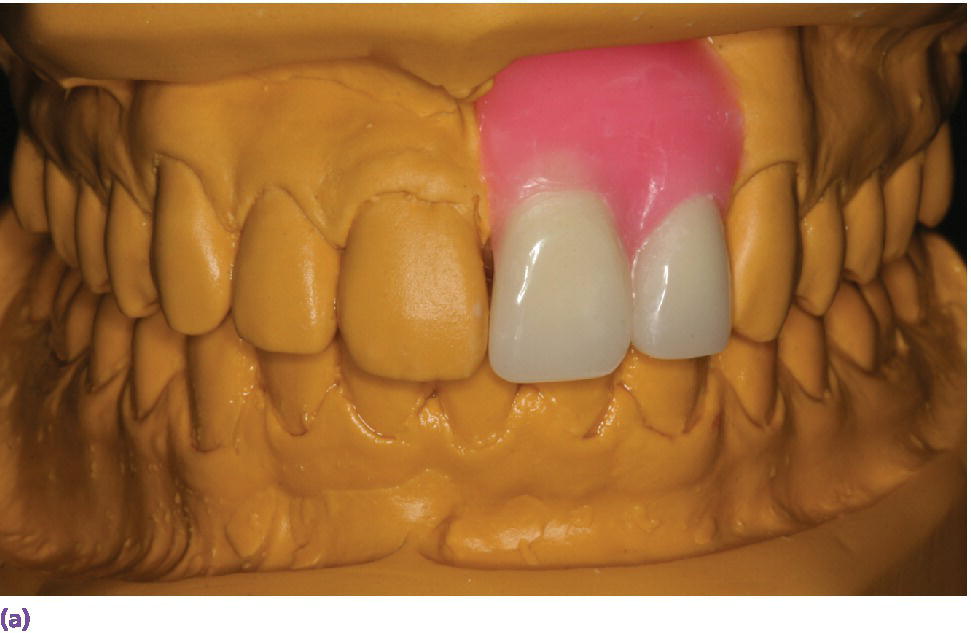


Figure 10.2 (a) Diagnostic wax‐up for the proposed definitive restorations on maxillary left central and lateral incisors. (b) Radiographic guide fabricated using a vacuum template with lead foils centered on each tooth tried intraorally, demonstrating deficiency in facial bone in relation to the proposed definitive restoration position. (c) Sagittal section through the CBCT volume showing deficiency in facial bone that was noticed clinically in a quantifiable manner. In such a case, augmentation would be considered based on these findings.
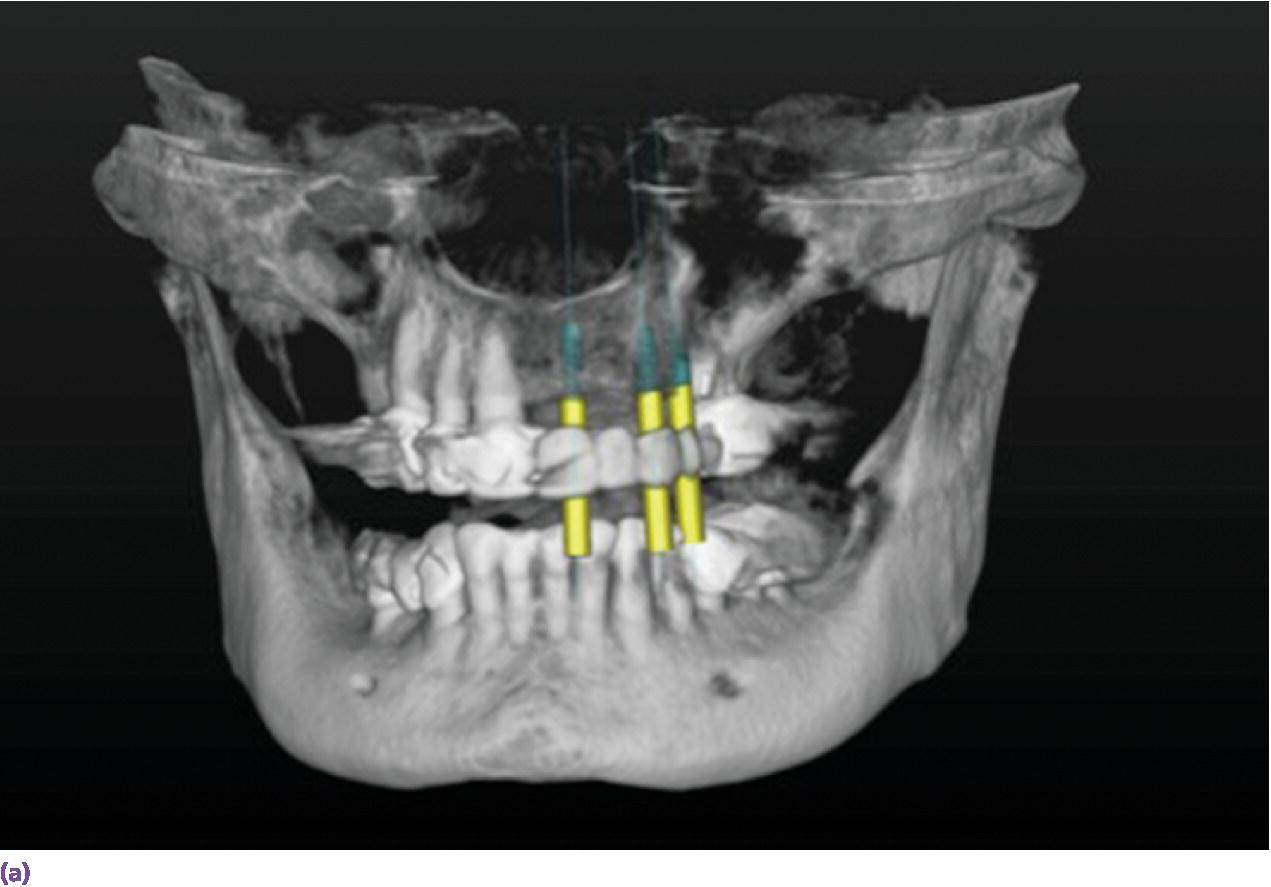


Figure 10.3 (a) Screen shot of the 3D view for virtual implant planning using Simplant Software. This is utilized to plan for implants at sites #9, 11, and 13. (b) Sagittal section that shows the long axis of implant planned at site #11. Planning was executed to allow for a screw‐retained prosthesis. (c) Occlusal view of the teeth‐supported CAD/CAM guide in place.
Planning the implant position
Single‐tooth implant restorations
Correct 3‐D implant placement is critical for an esthetic treatment outcome. It is well known that biologic width around implants is slightly more than the average dentogingival complex dimension,17–19 and the position of peri‐implant mucosa attachment tends to be subcrestal compared to natural teeth where biologic width always forms supracrestally.20 This makes maintaining or reforming the interdental papilla challenging and requires very careful planning for implant–tooth and inter‐implant distance. Tarnow and colleagues21 have shown that when the measurement from the interproximal coronal contact point to the crest of bone is 5 mm or less, the papilla is present almost 100% of the time. When the distance is 6 mm or greater, the papilla is present 50% of the time or less, and at 7 mm, the interdental space is completely filled about 25% of the time.21 Hence, in the esthetic zone, the distance from alveolar crest to the adjacent tooth cementoenamel junction should be 3–5 mm to achieve the ideal implant location and appropriate space for the peri‐implant sulcus to form.20–23
Control of the 3‐D implant placement is a prerequisite for a pleasing mucosal margin level. This includes its position in the apicoronal, mesiodistal, and labiopalatal directions. This can be achieved by placing the implant abutment interface 3 mm apically from the gingival zenith and displacing it palatally by 2 mm.9,10,24 Mesiodistally, it is recommended that a minimum distance of 1.5 mm be left between an implant and an adjacent tooth in order to maintain the bone and provide better esthetics.25 However, recent studies have shown that, when using the platform‐switching concept, it is possible to place the implant as close as 1 mm to the adjacent tooth without compromising crestal bone.26–31
Poor implant placement as a result of inadequate planning or poor execution of the plan can create significant esthetic complications. Placing the implant too deep or too facial might result in facial bone resorption and subsequent recession.16 Placing the implant too shallow results in a visible metal margin, while placing the implant too palatal results in an improper emergence with a ridge. However, when planned according to the correct parameters, an esthetic result is more predictable (Figure 10.4).



Figure 10.4 (a) Occlusal view of implant placed at site #8 demonstrating its facial and superficial misplacement. This creates a restorative challenge for providing a proper emergence profile and symmetrical midfacial gingival margin. (b) Facial view of zirconia abutment used to restore implant at site #8. Selection of zirconia was based on the patient’s thin tissue biotype. (c) Facial view of definitive implant restoration. Asymmetrical gingival zenith has resulted from inadequate implant placement.
Errors in the mesiodistal direction can substantially affect the generation of interproximal papillary support and bone crest resorption.9,12 Additionally, special care should be placed on selection of proper implant size, based on site anatomy and the planned restoration.
Multiple missing teeth
Multiple missing teeth in the esthetic zone require a great deal of attention. Critical factors that must be considered include the number of implants used, inter‐implant spacing, and angulation. Proper planning, with an ideal diagnostic wax‐up and utilization of a surgical guide to avoid misplacement at embrasure sites, are a must. It is commonly observed that it is more difficult to create a papilla between two adjacent implants than it is to maintain or create a papilla between an implant and a natural tooth.32 Tarnow and colleagues21 reported a mean papillary height between two adjacent implants as 3.4 mm. Reduced inter‐implant distance of less than 3 mm was shown to have a negative effect on the midproximal crestal bone levels. This is due to the extent of lateral bone loss. Maintaining a distance of more than 3 mm between two adjacent implants appears to preserve the interproximal bone peak and result in only 0.45 mm of resorption on average. In contrast, if the space between the implants is 3 mm or less, average resorption of the interproximal bone peak increases to 1.04 mm, which compromises support for the inter‐implant papilla.31,32 Selective utilization of implants with a smaller diameter at the implant–abutment interface may be beneficial when multiple implants are to be placed in the esthetic zone, so that a minimum of 3 mm of bone can be retained between them.32 In some cases involving multiple missing teeth, an implant‐supported fixed dental prosthesis may be a more preferable choice through alternating implants and pontics in order to optimize soft tissue esthetics.6 A greater projection of papilla may be seen around a pontic–pontic (6 mm) and implant–pontic (5.5 mm) than that between two implants (3.5 mm).33
Recent follow‐up studies using new implant designs with internal conical connection and platform switching have shown that inter‐implant bone levels can be maintained at similar levels when implants are placed at 2 mm or 3 mm inter‐implant distances.34–37 In cases where a significant amount of hard and soft tissue has been lost due to trauma or pathologies, it becomes imperative to plan for the use of pink ceramics or even the use of removable prostheses to compensate for the lost tissues.38
Anatomic factors
The presence of adequate bone and soft tissue volumes is crucial to achieving successful esthetic treatment outcome of dental implants in the anterior maxilla. Compromised esthetic outcomes, due to the crest collapse that occurs following extraction, in particular during the first 3 months after the extraction,34 is a major risk. A mean bone shrinkage of 3.79 mm horizontally and 1.24 mm vertically may occur following a tooth extraction in the maxilla.35 Greater bone loss takes place at multiple adjacent extraction sites.36 Ridge preservation can significantly limit the bone resorption process.37,39 Jambhekar and colleagues40 compared, in a systematic review, the clinical and histologic outcomes between various socket grafting procedures with the flapless extraction, after a minimum of 12 weeks of healing. The mean loss of buccolingual width at the ridge crest was lowest for xenografts (1.3 mm), followed by allografts (1.63 mm), alloplasts (2.13 mm), and sockets without any socket grafting (2.79 mm).40 Despite the reduced bone loss with ridge preservation, bone remodeling still occurs, resulting in a buccal concavity, which may ultimately cause an esthetic discrepancy. The amount of dimensional changes occurring following tooth loss is influenced by local factors, including periodontal status, presence of dehiscence, and the type and fit of the interim prosthesis, as well as systemic factors, such as patient’s general health and habits such as smoking. Preservation of the alveolar ridge dimension at both the hard and soft tissue level is critical to the functional and esthetic rehabilitation of missing teeth in the esthetic zone. Adequate soft tissue volumes may affect the soft tissue profile for the restorations. In addition, provision of proper hard tissue volume is necessary to allow placement of the dental implant as well as provide support of the soft tissues. There is a limit as to how much soft tissue can exist beyond the bone. The level of interdental papilla around single‐tooth implants is mostly dependent on the marginal bone level at the adjacent teeth rather than the peri‐implant marginal bone levels (Figure 10.5).22,41,42


Figure 10.5 (a) Facial view of implant crown at site #7 demonstrating deficient papillae on both the mesial and distal aspects. (b) Periapical radiograph at implant #7 demonstrating good marginal peri‐implant bone levels but reduced levels on adjacent teeth. Soft tissue levels around single‐tooth dental implants are affected by bone levels on adjacent teeth.
More favorable soft tissue outcomes are seen at non‐augmented sites than at augmented sites; this has been attributed to the scarring induced by additional surgical procedures rather than marginal bone levels, which are comparable at both sites.43 Long‐term studies have demonstrated that improvements in interdental papilla fill may occur over time following definitive prosthesis delivery.44–46
Patients with missing teeth may present with volumetric hard and soft tissue deficiencies in the vertical and buccolingual dimensions. Reconstruction of deficient tissues maybe ac‐complished by surgical and/or prosthetic treatment approaches. Hard tissue reconstruction may be obtained using block bone graft, guided bone regeneration, and orthodontic tooth extrusion and distraction methods. Vertical bone augmentation is more challenging than horizontal augmentation.47 Prosthetic methods include use of gingiva‐colored prosthetic material and creation of a long proximal contact area (Figures 10.6 and 10.7).48



Figure 10.6 (a) Missing maxillary anterior teeth and deficient hard and soft tissues as a result of trauma; vertical augmentation would not be predictable. (b) The definitive abutments with gold hue in place. (c) The use of pink ceramics was a necessity to compensate for the lost tissues and provide an optimum esthetic result.


Figure 10.7 (a) A three‐unit FDP adjacent to a natural tooth that needs a crown restoration. Custom abutments with gold hue are used to optimize esthetics. (b) Long proximal contacts were created to camouflage the short interdental papilla.
Advantages of prosthetic replacement of soft tissue include reduced morbidity associated with reconstructive surgeries, shortened treatment time, reduced treatment cost, and more predictable pink esthetics.38 Currently available gingiva‐colored prosthetic materials include acrylics, composite resins, or ceramics.38,49,50 Use of gingiva‐colored artificial materials, however, is technically demanding and requires skilled dental technicians. When this option is considered, bone reshaping to move the transition zone (junction between the prosthesis and natural gingiva) beneath the lip perimeter and to create a flat ridge between the implants may be needed.50
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


