Paediatric oral medicine, oral pathology and radiology
Michael J Aldred, Angus C Cameron and Anastasia Georgiou

Introduction
Although some disorders are confined to the mouth, oral lesions may be a sign of a systemic medical disorder. The majority of oral pathology seen in children is benign; however, it is essential to identify or eliminate more serious conditions. The presentation of pathology in children is often different from adult pathology and the subtleties of these differences are often important in diagnosis. In addition, many lesions change in form or extent with growth of the body. In this chapter, conditions will be grouped according to presentation, followed by a review of the most common causes and management of orofacial infections. It is important to remember that one disease entity may have different presentations while one presentation, e.g. an ulcer, may be representative of many different diseases.
Orofacial infections
Differential diagnosis
Odontogenic infections
The basic signs and symptoms of oral infection should be familiar to all clinicians.
Acute infection usually presents as an emergency:
Chronic infection typically presents as an asymptomatic or indolent process:
Presentation
• Maxillary canine fossa infections are predominantly Gram-positive or facultative anaerobic infections (Figure 10.1A). They may be misdiagnosed as a periorbital cellulitis (which is typically caused by Haemophilus influenzae or Staphylococcus aureus from haematogenous spread). Posterior spread may lead to cavernous sinus thrombosis and a brain abscess.
• Young patients may be dehydrated at presentation. It is important to ask about their fluid intake and ascertain whether the child has urinated during the previous 12 h (see Appendix B).
Management
The treatment of infection follows two basic tenets:
Criteria for hospital admission
Use of antibiotics
General considerations
• Extraction of involved teeth.
Or
• Root canal treatment for permanent teeth if it is considered important to save particular teeth (see Chapter 7).
Amoxicillin is usually the drug of first choice. This has the advantage that it is given only three times a day, achieves higher blood levels and is a more effective antibiotic than, e.g. phenoxymethylpenicillin (Penicillin VK). Often the extraction of the abscessed tooth alone will bring about resolution without antibiotic treatment.
Severe infections
• Drainage of any pus present. If the diagnosis or the correct management of an infection in the mandible has been delayed and the swelling has crossed the midline, or if there is swelling of the floor of the mouth, then extra-oral drainage with a through-and-through drain should be considered (Figure 10.1B). If a flap is raised, any granulation tissue should be removed and the area well irrigated. Flaps should be apposed but not tightly sutured. Soft flexible drains such as Penrose drains are better tolerated in children than are corrugated drains.
• Intravenous antibiotics. Benzylpenicillin is the drug of first choice (up to 200 mg/kg per day).
Osteomyelitis
Rarely, odontogenic infection may lead to osteomyelitis, most commonly involving the mandible. Radiographically, the bone has a ‘moth-eaten’ appearance. Curettage of the area is required to remove bony sequestra and antibiotics are given for at least 6 weeks, depending on the results of microbiological culture and sensitivity test results. A variant of osteomyelitis has been reported in children and adolescents, termed juvenile mandibular chronic osteomyelitis. In this condition, there is often no obvious odontogenic source of infection; there is limited response to a number of different treatment modalities.
Primary herpetic gingivostomatitis (Figure 10.2)
This is the most common cause of severe oral ulceration in children. It is caused by herpes simplex type 1 virus. Occasional cases of type 2 (the usual cause of genital herpes) infection have been reported, mainly in cases of sexual abuse. The clinical appearance of the two different strains of herpes simplex virus are, however, clinically identical in the orofacial region. Although the majority of the population has been infected with the virus by adulthood, less than 1% manifest an acute primary infection. This usually occurs after 6 months of age, often coincident with the eruption of the primary incisors. The peak incidence is between 12 and 18 months of age. Incubation time is 3–5 days with a prodromal 48-h history of irritability, pyrexia and malaise. The child is often unwell, has difficulty in eating and drinking and typically drools. Stomatitis is present, with the gingival tissues in particular becoming red and oedematous. Intraepithelial vesicles appear and rapidly break down to form painful ulcers. Vesicles may form on any part of the oral mucosa, including the skin around the lips. Solitary ulcers are usually small (3 mm) and painful with an erythematous margin, but larger ulcers with irregular margins often result from the coalescence of individual lesions. The disease is self-limiting and the ulcers heal spontaneously without scarring, within 10–14 days.
Diagnosis
Management
• Analgesics – paracetamol, 15 mg/kg, 4-hourly.
• Topical anaesthetics: lignocaine viscous 2% or lignocaine (Xylocaine™) spray.
Note: topical anaesthetics are often advocated; however, the effect of a numb mouth in a young child can be more distressing than the pain from the illness and can lead to ulceration from the decrease in sensation and subsequent trauma. In addition, it is often difficult to initiate swallowing with a soft palate that has been anaesthetized.
• Antiviral chemotherapy. Acyclovir oral suspension or intravenously for immunosuppressed patients. This treatment is only worthwhile in the vesicular phase of the infection, i.e. within the first 72 h.
Note: the use of antiviral medications is contentious and usually reserved for children who are immunocompromised. There is some evidence to suggest, however, that the administration of aciclovir in the first 72 h of the infection may be beneficial.
• Adequate pain control is also required with regular administration of paracetamol.
Herpangina and hand, foot and mouth disease
These infections are caused by the Coxsackie group A viruses. As with primary herpes, both of the above conditions have a prodromal phase of low-grade fever and malaise that may last for several days before the appearance of the vesicles. In herpangina (Figure 10.3A), a cluster of four to five vesicles are usually found on the palate, pillars of the fauces and pharynx, whereas in hand, foot and mouth disease up to 10 vesicles occur at these sites and elsewhere in the mouth, in addition to the hands and feet (Figure 10.3B). The skin lesions appear on the palmar surfaces of the hands and plantar surface of the feet and are surrounded by an erythematous margin. The severity of both diseases is usually milder than primary herpes and healing occurs within 10 days. Both diseases occur in epidemics, mainly affecting children.
Infectious mononucleosis (Figure 10.4A)
Varicella (Figure 10.4B)
This is a highly contagious virus causing chickenpox in younger subjects and shingles in older individuals. There is a prodromal phase of malaise and fever for 24 h followed by macular eruptions and vesicles. In chickenpox, oral lesions occur in around 50% of cases but only a small number of vesicles occur in the mouth. These lesions may be found anywhere in the mouth in addition to other mucosal sites such as conjunctivae, nose or anus. Healing of oral lesions is uneventful.
Measles
Measles is a highly contagious paramyxovirus infection, predominately of childhood that presents as an acute febrile illness, a maculopapular rash, keratoconjunctivitis, malaise, cough and the characteristic oral lesions – Koplik’s spots. These are small white papules surrounded by an erythematous margin and cover the buccal mucosa. They usually precede the typical measles rash by up to 4 days. The incubation period is 8–12 days with a prodromal phase of malaise, fever, cough and the oral signs. Healing of oral lesions is uneventful; however, some children may suffer other complications of the disease such as pneumonia (1 in 20) or encephalitis (1 in 1000).
Candidosis
Acute pseudomembranous candidosis
The most common presentation of candidal infection in infants is thrush. White plaques are present, which on removal reveal an erythematous, sometimes haemorrhagic, base. In older children, thrush occurs when children are immunocompromised such as in acquired immune deficiency syndrome (AIDS) or in diabetes, or when prescribed antibiotics, steroids, or during chemotherapy and radiotherapy for malignancies.
Median rhomboid glossitis
This characteristic but uncommon lesion, is a candidosis (rather than a developmental anomaly as was thought for many years) presenting as an erythematous, depapillated well-delineated area on the midline of the dorsal surface of the tongue anterior to the circumvallate papillae, often in children in response to the use of antibiotics.
Diagnosis
Some 50% of children will have Candida albicans as a normal commensal, and culture is of little benefit. Smears or scrapings for exfoliative cytology reveal hyphae when disease is present, but the clinical picture may be diagnostic.
Ulcerative and vesiculobullous lesions
Clinicians are often confused regarding the terminology of these lesions. An ulcer is regarded as the localized loss of the full-thickness of the epithelium. Partial thickness loss is termed an erosion. A vesicle is a small fluid-filled blister, while a bulla is a larger blister, generally, measuring >5 mm. Different conditions arise from cleavage of the epithelium at different levels (i.e. intraepithelial or subepithelial) and are important in determining a diagnosis. When these lesions burst, they leave an ulcer. A thorough history noting the number, frequency, duration and site of occurrence is very important.
Differential diagnosis
Lip ulceration after mandibular block anaesthesia
This is one of the most common causes of traumatic ulceration. Parents should be warned and children reminded not to bite their lips after mandibular block anaesthesia (Figure 10.5A).
Riga–Fedé ulceration
This is ulceration of the ventral surface of the tongue caused by trauma from continual protrusive and retrusive movements over the lower incisors (Figure 10.5B). Once a common finding in cases of whooping cough, it is now almost exclusively seen in children with cerebral palsy.
Management
Smoothen sharp incisal edges or place domes of composite resin over the teeth. Rarely, in severe cases, extraction of the teeth might be considered (see also Chapter 13).
Recurrent aphthous ulceration (Figure 10.6)
Recurrent aphthous ulceration (RAU) has been estimated to affect up to 20% of the population. Lesions are classification according to size, duration and severity. Two clinical groups have been described:
• Simple
• Major aphthae (Figure 10.6B).
• Complex
• This fourth form – complex aphthous stomatitis has recently been described.
Minor aphthae account for the majority of cases, with crops of two to five shallow ulcers measuring up to 5 mm and occurring on non-keratinized mucosa. There is a typical central yellow slough with an erythematous halo. Ulcers heal within 10–14 days without scarring. The cause of RAU is contentious, although it is commonly believed to be precipitated by stress and local trauma. There is some evidence for a genetic basis for the disorder, with an increased incidence of ulceration in children when both parents have RAU. Some studies have suggested that RAU is associated with nutritional deficiency states and so haematological investigation can be helpful. In major aphthae, the keratinized mucosa may also be involved, the ulcers are larger, last longer and heal with scarring.
Complex aphthous stomatitis accounts for less than 5% of cases that are recurrent, with multiple lesions that are extremely painful and are slow to heal. The differences between simple and complex forms are summarized in Table 10.1.
Table 10.1
Presentation of aphthous stomatitis
| Simple | Complex | |
| Frequency | Episodic; <6 episodes per year | Continuous rather than episodic; >6 episodes per year |
| Duration | Short-lived | Persistent |
| Number | Few/limited number of lesions | Many, rather than few lesions |
| Healing | Rapid healing and generally heal without scarring except for major aphthae | Slower to heal with scarring |
| Location | Generally confined to non-keratinized mucosa | Can involve both keratinized and non-keratinized mucosa |
| Pain | Minimal pain/discomfort with minimal disability | Extremely painful and disabling |
| Geography | Limited to oral mucosa | May have genital involvement Need to exclude Behçet’s disease |
Modified from Rogers, R.S. 3rd, 1997. Recurrent aphthous stomatitis: clinical characteristics and associated systemic disorders. Seminars in Cutaneous Medicine and Surgery 16, 278–283.
Diagnosis
Management
• Symptomatic care with mouthrinses:
• Chlorhexidine gluconate 0.2%, 10 mL three times daily.
• Benzydamine hydrochloride 0.15% and chlorhexidine 0.12% (Difflam C™).
• Triamcinolone in Orabase™ (although this may be difficult to apply in children).
• Beclomethasone dipropionate or fluticasone propionate asthma inhalers sprayed onto the ulcers.
• Betamethasone dipropionate 0.05% (Diprosone OV) ointment.
• Systemic corticosteroids only in most severe cases of major aphthous ulceration.
• Herpetiform ulceration seems to respond best to minocycline mouthwashes.
Biopsy should only be considered if there is any doubt about the clinical diagnosis. Haematological investigations should be carried out to exclude anaemia or haematinic deficiency states (when appropriate, replacement can improve the ulceration or bring about resolution). As with all oral ulceration, symptomatic care with appropriate analgesics and antiseptic mouthwashes is appropriate. In those cases of severe recurrent oral ulceration, systemic corticosteroids may be used, although their use is best avoided in children. Minocycline mouthwashes should not be used in children under the age of 8 years to avoid tooth discolouration. Major aphthae tend to occur in older children.
Behçet syndrome
This condition is characterized by recurrent aphthous ulceration together with genital and ocular lesions, although the skin and other systems can also be involved. Lesions may affect other parts of the body. Behçet syndrome can be subdivided into four main types:
• Mucocutaneous form – classical form with involvement of oral and genital mucosa and conjunctiva.
• Arthritic form with arthritis in association with mucocutaneous lesions.
• Neurological form with central nervous system involvement.
• Ocular form with uveitis in addition to oral and genital lesions.
Management
As for recurrent aphthous ulceration, but systemic treatment (corticosteroids) is usually required.
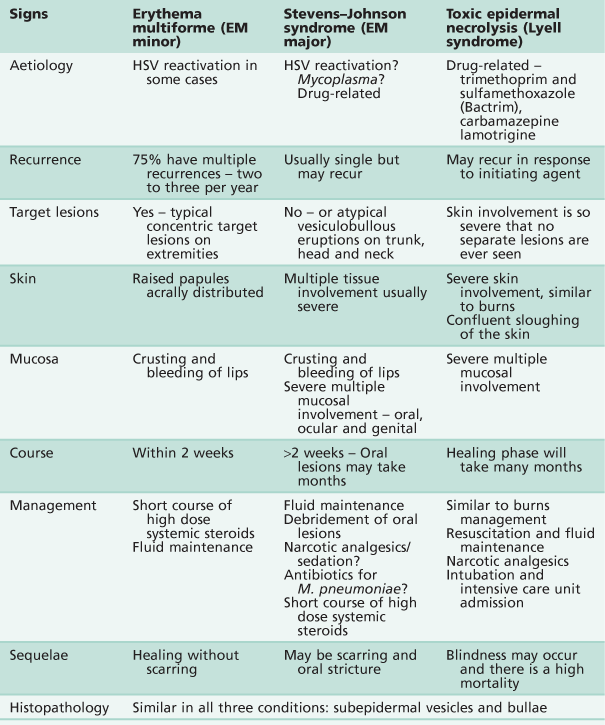
Erythema multiforme, Stevens–Johnson syndrome and toxic epidermal necrolysis
Three conditions exist that present with similar clinical signs and histopathological appearances. Like many conditions, varied nomenclature and misdiagnosis have clouded and confused the diagnosis/es. There is now a view that these are distinct pathological entities and, perhaps importantly, might be initiated by quite distinct aetiological agents. The alternative view is that these disorders represent different presentations of the same basic disorder, distinguished by the severity and extent of the lesions.
Erythema multiforme (von Hebra) (Figure 10.7A–D)
The original description of erythema multiforme was that of a self-limiting but often recurrent and seasonal skin disease with mucosal involvement limited to the oral cavity. The lips are typically ulcerated with blood-staining and crusting. The characteristic macules (‘target lesions’) occur on the limbs but with less involvement of the trunk or head and neck. These lesions are concentric with an erythematous halo and a central blister. Although the lesions are extremely painful, the course of the illness is benign and healing is uneventful.
Stevens–Johnson syndrome (Figure 10.7E,F)
The condition presents with acute febrile illness, generalized exanthema, lesions involving the oral cavity and a severe purulent conjunctivitis. The skin lesions are more extensive than those of erythema multiforme. Stevens–Johnson syndrome is characterized by vesiculobullous eruptions over the body, in particular the trunk, and severe involvement of multiple mucous membranes including the vulva or penis and conjunctiva. The course of the condition is longer and scarring may occur. Some authors have used the term erythema multiforme major for Stevens–Johnson syndrome, defining the condition as a severe form of erythema multiforme, but this is disputed by others. Although Stevens–Johnson syndrome patients are acutely ill, death is rare.
Toxic epidermal necrolysis (TEN)
Similar to the clinical presentation of Stevens–Johnson syndrome, TEN or Lyell syndrome is a severe, sometimes fatal, bullous drug-induced eruption where sheets of skin are lost. It resembles third-degree burns or staphylococcal scalded skin syndrome. Oral involvement is similar to Stevens–Johnson syndrome. TEN may be misdiagnosed as a severe form of Stevens–Johnson syndrome (given the controversy over nomenclature), but the use of steroids is contraindicated, given an increase in mortality with their use in this disease.
Aetiology
Erythema multiforme is often initiated by herpes simplex reactivation. There is some evidence that Stevens–Johnson syndrome is initiated by a Mycoplasma pneumoniae respiratory infection or drug reaction. TEN is drug-induced.
Clinical presentation
A summary of the three conditions is shown in Table 10.2. There is an acute onset of fever, cough, sore throat and malaise, followed by the appearance of the lesions on the body and oral cavity ranging from 2 days to 2 weeks after the onset of symptoms. These break down quickly in the mouth to form ulcers. The most striking feature is the degree of oral mucosal involvement that may lead in all three cases to a pan stomatitis and sloughing of the whole oral mucosa. There is extensive ulceration and crusting around the lips, oral haemorrhage and necrosis of skin and mucosa leading to secondary infection. There may be difficulty in eating and drinking, which complicates the clinical course, and there is usually extreme discomfort from both the skin and oral lesions that may necessitate narcotic analgesics.
Management
If there is a known precipitating factor such as herpes simplex infection, then antivirals such as topical aciclovir can be used in an attempt at prophylaxis. Management is generally symptomatic and supportive. A major problem during the course of the illness is fluid balance and pain, much of which arises from secondary infection of the oral lesions. Debridement of the oral cavity with 0.2% chlorhexidine gluconate or benzydamine hydrochloride and chlorhexidine (Difflam C™) is effective in removing much of the necrotic debris from the mouth. Extensive areas of ulceration tend to be less responsive to chlorhexidine and a minocycline mouthwash may prove more effective. The role of systemic steroids is controversial but they may be necessary in severe cases. Their use in recurrences may obviate the need for hospital admission.
Management also includes:
Pemphigus
Pemphigus is an important vesiculo-bullous disease mainly affecting adults; however, children can be also affected. The lesions are intraepithelial and rapidly break down, so that affected individuals are often unaware of blistering, complaining instead of ulceration, mainly affecting the buccal mucosa, palate and lips.
Diagnosis
There may be a positive Nikolsky sign (separation of the superficial epithelial layers from the basal layer produced by rubbing or gentle pressure) and cytological examination can reveal the presence of Tzanck cells. Direct immunofluorescence using frozen sections from an oral biopsy will reveal intercellular immunoglobulin (IgG) deposits in the epithelium that are diagnostic for this disease. Indirect immunofluorescence on blood samples is used to complement diagnosis.
Management
• Systemic corticosteroid therapy in conjunction with steroid-sparing agents.
• Topical corticosteroids are used for oral lesions.
• Antiseptic or minocycline mouthwashes and analgesia as necessary.
All of these mucocutaneous conditions in children heal with scarring and are managed similarly.
Epidermolysis bullosa (Figure 10.6D)
Epidermolysis bullosa is a term used to describe several hereditary vesiculo-bullous disorders of the skin and mucosa. Within the hereditary variants, there are three groups according to the location of skin separation:
Another form which is not inherited, is termed Epidermolysis bullosa acquisita.
Blisters may form from birth or appear in the first few weeks of life, depending on the form of the disease. Corneal ulceration may also be present and pitting enamel hypoplasia has been reported, mainly in the junctional forms of the disease.
Management
Management is often extremely difficult because of the fragility of the skin and oral mucosa. Intensive preventive dental care is essential to prevent dental caries, combined with treatment of early decay. Supportive care is required with the use of chlorhexidine gluconate mouthwashes and possibly topical anaesthetics such as lignocaine (Xylocaine viscous™). Fortunately, children may receive dental treatment under general anaesthesia without laryngeal complications. Because of oral stricture, however, access into the mouth is often difficult and in older patients, surgical release of the commissure may be necessary. It is important to cover instruments with copious lubricant; the use of rubber dam is essential.
Systemic lupus erythematosus
Systemic lupus erythematosus is a chronic inflammatory multisystem disease occurring predominantly in young women. The hallmark of systemic lupus erythematosus is the presence of antinuclear antibodies which form circulating immune complexes with DNA. Oral ulceration often occurs in systemic lupus erythematosus and treatment of the condition usually involves systemic steroids.
Orofacial granulomatosis and Crohn disease (Figure 10.8)
Although not primarily an ulcerative condition, oral ulceration may be the presenting sign in orofacial granulomatosis. Orofacial granulomatosis may be confined to the orofacial region and precede or be a manifestation of Crohn disease, an inflammatory condition of the gastrointestinal tract, or of sarcoidosis.
Presentation
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses