Orthodontics II
Management of occlusal problems
Chapter Contents
Overview
The management of malocclusion comprises a substantial part of orthodontic practice. It ranges from interception of developing occlusal problems through to comprehensive correction of established malocclusion in the adolescent or adult. It also encompasses the special requirements in orthodontic care of those with cleft lip and/or palate.
This chapter describes the management of the developing dentition and of all major anomalies of established malocclusion, including surgical correction. The occlusal problems particular to cleft lip and/or palate together with their management are also outlined.
10.1 Problem solving in the developing dentition
Although most orthodontic treatment is undertaken when the permanent dentition is established, some aspects of the developing occlusion may be better dealt with in the mixed dentition. Such interception may eliminate the need for, or simplify, later treatment. Systematic and regular screening of the developing dentition is essential to this process.
Anomalies of eruption and exfoliation
Both eruption and exfoliation of primary and permanent teeth may be premature or delayed.
Natal teeth
Natal teeth are usually lower incisors that are erupted at birth or appear soon after. Removal is indicated only if they interfere with suckling or if they are so mobile as to be at risk of inhalation.
Eruption of teeth
Other than natal teeth, the following points should be borne in mind:
Factors causing premature exfoliation or delay in the eruption and exfoliation of primary or permanent teeth are given in Table 10.1.
Table 10.1
Causes of premature or delayed eruption of primary or permanent teeth
| Causes | |
| Premature eruption | Familial tendency Primary dentition: high birthweight Permanent dentition: early-onset puberty, excess growth or thyroid hormone secretion |
| Delayed eruption | Primary dentition: very low birthweight, premature birth General causes: Down or Turner syndromes, severe nutritional deficiency, hypothyroidism/hypopituitarism, cleidocranial dysplasia, hereditary gingival hyperplasia, cleft lip and palate Local causes: ectopic crypt position, supernumerary or odontome, congenital absence, retention of primary tooth, dilaceration, primary failure of eruption, crowding |
| Premature exfoliation | Commonly caries or trauma Rarely hereditary hypophosphatasia, congenital neutropenia, cyclic neutropenia, Chediak–Higashi syndrome, histiocytosis X |
| Delayed exfoliation | Congenital absence of permanent successor Ectopic position of permanent successor Trauma Severe periradicular infection of primary tooth |
To ensure that any deviation in the normal eruption sequence is detected early, clinical vigilance is required during the developing dentition, supported by radiographic investigations where necessary. Particular attention should be given to the permanent maxillary incisors and canines, as early recognition of an anomaly in their eruption improves the prognosis.
Hypodontia
The most common missing teeth are:
Absent third molars
Extraction of a second molar, either to facilitate distal movement of the upper buccal segments or to relieve posterior crowding, should not be considered in the absence of a third molar. These start to calcify any time between 8 and 14 years.
Absent upper lateral incisors
Management options for the space created by absent upper lateral incisors are:
The final decision depends on:
• the patient’s attitude to orthodontic treatment
• the anteroposterior and vertical skeletal relationships
• amount of exposure of the upper canines and incisors on smiling
• the colour, size, shape and inclination of the canine and incisor teeth
The possible plans are best assessed by carrying out a trial set-up of each on duplicate study models, followed by joint consultation with a restorative colleague.
Space opening
In uncrowded or mildly crowded arches, when the buccal segment occlusion is class I or, at most, half unit class II, or in class III where proclination of the incisors is likely to correct an anterior crossbite, space opening is best. In addition, in patients with low Frankfort–mandibular plane angle (FMPA) or where the maxillary canine is considerably darker than the incisors, it may be best to open rather than close the anterior spaces. A fixed appliance may be needed to localise space for the missing units, followed by at least 3–6 months of removable appliance retention ensuring that the space is maintained by placing wire spurs in contact with the adjoining teeth. If it is possible to reposition the incisors and canines into their desired locations by tipping movements, a removable rather than a fixed appliance may be used. In selected cases, autotransplantation of lower premolars (extracted for relief of crowding) to the upper lateral incisor area may be possible. The prognosis is best when the root of the lower premolars is half to two-thirds formed; surgery must also be deftly planned and carried out to ensure optimal preparation of the donor site and prevent root surface damage. More commonly, the missing units may be replaced on resin-retained bridgework, and occasionally by implants at a later date. If bridgework is planned, it is important to ensure that sufficient interocclusal clearance exists for placement of the metal framework; if not, this should be created during appliance therapy.
Space closure
In crowded mouths, early extraction of the primary canines should be carried out to encourage mesial drift of the posterior teeth, but a later phase of fixed appliance therapy is usually needed to align and approximate the upper anterior teeth, followed by bonded retention. Recontouring of the canines in addition to composite build-up of their mesio-incisal aspects is advisable before treatment starts to assist with definitive tooth positioning; final restorations are placed following appliance removal. Bleaching of the canines may also be required to enhance aesthetics. Overjet reduction by space closure may be more favourable than resorting to midarch extractions and space opening. Space closure is likely to be facilitated in patients with increased FMPA, crowding and where the buccal segment relationship is a full unit class II.
Absent second premolars
The primary second molar should be retained where the arch is uncrowded or aligned. If the tooth starts to submerge, an occlusal onlay may be placed to maintain it in function. Removal of the lower second primary molar shortly after eruption of the lateral incisors will encourage spontaneous space closure in mildly crowded mouths, but in those with marked crowding, its extraction should be delayed until orthodontic treatment commences so that the resulting space may be used for arch alignment. In the upper arch, extraction of the second primary molar is again best deferred until orthodontic treatment is about to start. Rarely, a lower second premolar develops late and necessitates an alteration in the original treatment plan.
Absent lower central incisors
In the absence of permanent lower central incisors, root resorption and progressive incisal wear may lead to loss of the primary incisors in the late mixed dentition, although occasionally they can last for longer. A fixed appliance may be needed to close incisor spacing in a crowded mouth or to align the lateral incisors prior to placement of resin-retained bridgework in an uncrowded arch. Where one or both lower central incisors is missing and the space is closed orthodontically, mild crowding may result in the upper labial segment as six anterior teeth are arranged around four or five lower teeth.
Supernumerary teeth
Teeth additional to the normal number are termed ‘supernumerary’. Most commonly, they occur in the premaxilla (mesiodens) but they often also develop distal to the last tooth in each dental series (lateral incisor, second premolar and third molar) as an exuberant growth of the dental lamina, perhaps representing a tertiary dentition. They are more common:
• in the permanent than in the primary dentition (respective incidences 2% and 1%)
• in children with cleft of the lip and alveolus and cleidocranial dyostosis.
Those in the premaxilla can be categorised into three groups: conical, tuberculate and supplemental.
Conical teeth
Conical teeth occur between the upper permanent central incisors; they are often singular but can sometimes occur in combination with others of similar form. They may have no effect if they are well above the apices of the incisors. If there is no risk of damage to adjacent teeth with tooth movement, they can be left in place and observed. Often, however, they may displace the adjacent teeth, perhaps creating a large diastema, or they may delay eruption. In these instances, removal is indicated. Occasionally, a conical supernumerary tooth erupts and can be extracted.
Tuberculate teeth
Tuberculate teeth are the most common cause of an unerupted permanent maxillary central incisor. Suspicion should be raised if the lateral incisors erupt in advance of the centrals. In these cases, a radiograph of the premaxilla should be taken to allow early detection and localisation of any supernumerary, which should then be surgically removed. An attachment with gold chain or a magnet should be bonded to the unerupted incisor to allow provision for orthodontic alignment if the tooth fails to erupt spontaneously within 12 months of surgery. In conjunction with surgery, space to accommodate the unerupted tooth must be maintained or opened by appliance therapy; the latter may entail extraction of the upper primary canines.
Supplemental teeth
The supplemental tooth resembles the normal tooth in morphology and commonly produces crowding or displacement of adjacent teeth. Usually, the tooth, which is similar to the contralateral tooth, is better retained (provided it is not severely malpositioned) and the other incisor is extracted.
Anomalies of development
First permanent molars with poor long-term prognosis
The first permanent molar is never the extraction of choice for orthodontic reasons but is invariably enforced because of poor prognosis resulting from caries and/or enamel hypoplasia. Enamel decalcification on the lingual aspect of lower first permanent molars or on the buccal aspect of upper first permanent molars should be treated seriously, as it is often a hallmark of a high caries rate and possible limited lifespan of these teeth. When a two-surface or deep occlusal restoration is indicated in one molar 2–3 years after eruption, careful assessment of the malocclusion and the condition of the other first permanent molars should be made. Timely removal may lead to considerable spontaneous correction of the malocclusion in certain patients but it does little for relief of incisor crowding or correction of an incisor relationship unless appliance therapy is instituted.
A ‘cook book’ approach to each patient with poor-quality first permanent molars is not possible but some guidelines are listed in Box 10.1.
Infraoccluded primary molars
Between 1–9% of children are likely to exhibit this anomaly but estimates regarding its incidence vary. A genetic tendency has been suggested with absent premolars, ectopic position of the first permanent molars and palatal canine displacement identified as associated factors. Infraocclusion results from ankylosis of the tooth while alveolar growth and eruption of the adjacent teeth continues. Provided the permanent successor is present, exfoliation will occur eventually, but removal is indicated in its absence and where the infraocclusion is marked, with the crown of the tooth just visible, or where root development of the unerupted premolar is almost complete.
Impaction of the maxillary first permanent molar
Impaction of the maxillary first permanent molar occurs in 2–6% of children. It may correct spontaneously (unlikely after the upper lateral incisors erupt) or it may require disimpaction of the molar either by placing a brass wire separator between the adjacent teeth (in mild problems) or by appliance therapy (in more marked impaction). Extraction of the second primary molar is required if the impaction produces symptomatic resorption with pulpal involvement or to facilitate restoration of the first permanent molar. Crowding is exacerbated by the subsequent mesial drift of the first permanent molar, but this can be treated later.
Aberrant position of second premolars
Occasionally, the second premolars appear in slightly unfavourable positions when viewed on a radiograph, but generally this is of no long-term consequence and their final position is usually satisfactory. A grossly ectopic second premolar is rare and may be observed or surgically removed.
Posterior crossbite with mandibular displacement
Sometimes, a unilateral crossbite of the buccal segment teeth with mandibular displacement follows a prolonged finger- or thumb-sucking habit. In some children, grinding the primary canines can lead to correction and prevent perpetuation of the crossbite from the mixed to the permanent dentition; where this is not effective, arch expansion by using either a removable appliance and a midline screw or a quadhelix is required to reduce the chance of the crossbite being present in the permanent dentition. Alternatively, correction may be deferred until the premolars erupt (Fig. 10.1).
Treatment of anomalies by serial extractions
In 1948, Kjellgren, a Swedish orthodontist, ascribed the term ‘serial extractions’ to the following three-stage procedure:
This approach works best in children with class I malocclusion at about 9 years, with moderate crowding, average overbite and a full complement of teeth and where there is no doubt about the long-term prognosis of the first permanent molars. It was originally intended to remove the need for appliance therapy but, in practice, this is seldom the case. In addition, extractions under general anaesthesia is an unpleasant and often frightening introduction to dentistry for any child, which may psychologically scar their attitude to subsequent dental treatment. As a result, the full extent of the original technique is never adopted in contemporary orthodontic practice, but consideration is often given to the need to extract the primary canines in the following instances:
Other developmental problems
Early loss of primary teeth
Early loss of primary teeth is most commonly caused by caries but, occasionally, it results from premature exfoliation, often when there is severe crowding, or it may be planned (e.g. to encourage space closure by mesial drift of the buccal segments in children who are missing one or more permanent teeth). In all cases, consideration should be given to balancing (extraction of the same tooth on the opposite side of the arch) or to compensating (extraction of the equivalent opposing tooth) for an extraction. Premature loss of a primary tooth does not inevitably lead to premature eruption of the permanent successor.
The effects of early loss of a primary tooth depend on several factors including:
All of these influence the potential for crowding to be concentrated at the extraction site. In general, this potential is greatest in a young child with pre-existing crowding when a maxillary posterior tooth is removed with poor buccal segment intercuspation.
Incisors
Early loss of a primary incisor tends to have minimal effect as it usually exfoliates in the early mixed dentition. Premature loss of a primary incisor through trauma may, however, lead to dilaceration of the permanent successor.
Canines
Unilateral loss of a primary canine invariably leads to movement of the centreline and should be balanced to prevent this occurring.
First molars
Occasionally, displacement of the centreline follows early extraction of a first primary molar, but the need for a balancing extraction is best assessed by checking the midlines at subsequent reviews.
Second primary molars
Where the second primary molar is extracted, the first permanent molar migrates mesially and may lead to considerable space loss if the extraction is carried out before the permanent molar erupts; hence, it is preferable to delay extraction until the first permanent molar has erupted. The need for a lower compensating extraction should be considered carefully if removal of an upper second primary molar of poor prognosis would allow the first permanent molar to move forward to become a full unit class II from a half class II relationship.
Space maintenance for early tooth loss
Space maintenance is indicated:
A removable appliance will usually suffice in the upper arch but a lingual arch soldered to bands cemented to molar teeth is best in the lower.
Upper median diastema
Upper median diastema is a normal phase of dental development and usually reduces as the permanent maxillary canines erupt. It may, however, also result from:
• a midline supernumerary tooth
• missing or small upper lateral incisors
• incisor proclination in class II division 1 malocclusion (Section 10.3) or due to a digit-sucking habit
• a more generalised spacing condition due to mismatch in tooth/arch size (Section 10.2).
A radiograph of the upper incisor area should be taken to exclude the presence of a supernumerary tooth in those with a large midline diastema. Rarely, a low-lying attachment of the labial frenum is a primary cause, as the attachment usually recedes as the incisors approximate. In a spaced arch, this does not occur, indicating that the frenum is associated with, but not causative of, the diastema.
Where the frenum is implicated in causing a diastema, blanching of the incisive papilla usually occurs when the lip is pulled upwards or outwards, with characteristic V-shaped notching of the alveolar bone between the two central incisors visible radiographically. The need for fraenectomy should be assessed after eruption of the permanent canines and is preferably undertaken during space closure as the scar tissue will aid approximation of the incisors. Treatment of the diastema in the early mixed dentition may be necessary if there is insufficient space for the lateral incisors and the diastema exceeds 3 mm but vigilance is needed to ensure that the lateral incisor roots are not moved into the path of the erupting canines. A fixed appliance is usually required to close an upper midline space, with bodily approximation of the incisors followed by palatal bonded retention.
Dilaceration
Dilaceration is a sudden angular alteration in the long axis of the crown or in the root of a tooth. Most commonly it results from intrusion of a primary incisor driving the crown of the permanent successor palatally, and it leads to enamel and dentine hypoplasia. On occasion, dilaceration is developmental in origin, with a characteristic labial and superior coronal deflection of the affected tooth. Usually, a dilacerated incisor remains unerupted and requires surgical removal but, if the dilaceration is mild, surgical exposure and orthodontic alignment may be feasible when the root apex is destined not to perforate the cortical plate.
Traumatic loss of an upper permanent central incisor
As the adjacent teeth tend to tilt toward the site of loss in the first days following trauma, the space must be maintained, ideally by immediate reimplantation of the tooth or by fitting a denture carrying a replacement tooth. Later, autotransplantation of a premolar or adhesive bridgework may be considered. This is generally preferable to space closure, as a lateral incisor rarely gives an optimum appearance in a central incisor position, even with coronal build-up and gingival recontouring.
Incisors in crossbite
Early correction of a crossbite involving a permanent incisor is essential to prevent displacing occlusal forces compromising the periodontal support of the lower anterior teeth and to allow the occlusion to develop around an undisplaced condylar position. Provided there is likely to be adequate overbite of 2–3 mm, an upper removable appliance with a double-cantilever spring to procline the instanding incisor and posterior capping to disengage the occlusion will usually suffice (see Section 10.5 and Fig. 10.2). It may be necessary to remove the upper primary canines to facilitate crossbite correction on a permanent upper lateral incisor or the lower primary canines to allow alignment of a labially placed permanent lower incisor.
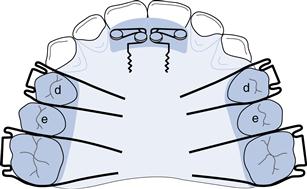
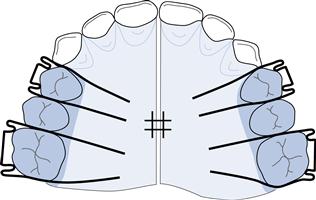
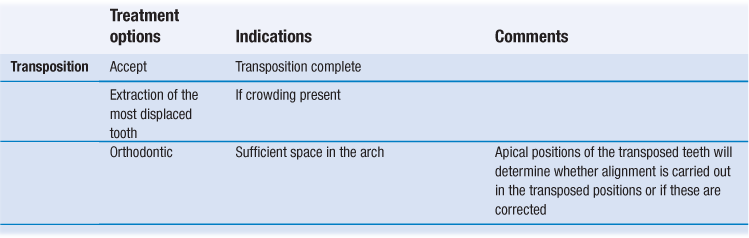
Fig. 10.2 Upper removable appliance to procline 1|1 in the early mixed dentition, assuming all primary teeth are in good condition.
Double cantilever springs 1|1 (0.5 mm SS wire); Adams’ clasps d|d (0.6 mm SS wire) and 6|6 (0.7 mm SS wire); posterior capping 2–3 mm in height to disengage the anterior occlusion.
Habits
Depending on the positioning of a finger(s) or thumb, the frequency and intensity of a sucking habit may:
Gentle persuasion to discontinue the habit should be given and simple measures adopted to effect this. An upper removable ‘reminder’ appliance may be fitted if the child is eager to stop.
Increased overjet
Where the overjet is greater than 3 mm, the risk of incisor trauma is more than doubled; trauma is more common in boys and the risk is greater with incompetent lips. An initial phase of functional appliance therapy to retract the incisors may be beneficial in these children but seldom produces complete correction of the malocclusion. Often, it is necessary to proceed to a second phase of treatment when the permanent dentition is fully erupted. This usually involves fixed appliances to detail the occlusion in combination with premolar extractions for relief of crowding. An early start to overjet correction can lead to protracted treatment, as the functional appliance will need to be worn as a retainer at least until a possible second phase of treatment commences and most likely until growth is complete. As this places considerable demands on patient co-operation, the likely benefits of early treatment must be deemed to outweigh any potential disadvantages before commencing on this course. There is also a potential risk of upper incisor root resorption if these teeth are retracted into the upper canine eruption path.
In recent years, the results of a randomised controlled clinical trial in North America have indicated that early skeletal effects produced by either functional or headgear therapy in the preadolescent period were not maintained long term. In addition, little or no differences existed following fixed appliance therapy in the permanent dentition between those who had been treated earlier or who had been observed until the permanent dentition erupted. A multicentre randomised controlled trial in the UK found that children treated at 8–10 years of age by a functional appliance had higher self-concept scores when evaluated 15 months later compared to those allocated to the control group. Many clinicians now prefer to wait until the permanent dentition is established before considering possible extractions for overjet correction and relief of crowding. A mixed dentition functional appliance phase, however, is beneficial to psychosocial wellbeing where the child is being teased because of the dentofacial anomaly; interestingly, a reduction in the risk of incisor trauma may not follow based on the findings of recent randomised clinical trials. The need for a custom-made mouthguard for sports, therefore, should be emphasised to those where treatment is deferred until the permanent dentition and in others following functional treatment.
Ectopic maxillary canines
The maxillary canine is ectopic in approximately 2% of the population, with 15% of these buccal and 85% palatal to the arch. Development of the maxillary canine begins about 4–5 months after birth and the crown is complete around 6–7 years of age. From an initial position high in the maxilla, the tooth moves buccally downwards and forwards to be guided into its final position by the distal aspect of the lateral incisor root. For this reason, absence or diminution in the size of the lateral incisor increases the incidence of displacement (×2.4). There also appears to be a greater incidence of palatal canine displacement where the maxillary arch is spaced or in class II division 2 malocclusion; a genetic link has been suggested and palatal displacement has a familial tendency, is more common in females than males, occurs bilaterally more than seems likely and is associated with absent or small teeth. Buccal displacement is more common in crowded arches. Where routine palpation of the buccal sulcus at 10 years fails to detect a canine prominence, the path of eruption is likely to be abnormal. In addition, considerable delay in the eruption of a canine compared with the opposite side of the arch points to canine displacement.
Transposition
Transposition is when the position of the canine is interchanged with that of an adjacent tooth. In the upper arch, the maxillary canine and first premolar, or the lateral incisor and canine, are involved, although the former arrangement is more common. In the lower arch, this anomaly affects solely the lateral incisor and canine teeth.
Estimating the maxillary canine position
Clinical estimate
Buccal and palatal palpation along with observation of the lateral incisor inclination give a hint to the canine position. When it is lying low and palatal or high and buccal, the lateral incisor is likely to be labially inclined.
Radiographic estimation
Although a dental panoramic tomogram is helpful in initial assessment of canine position, further radiographic views are needed to locate the position of the tooth. Most commonly an upper anterior occlusal view or two periapical films taken with a tube shift are needed to allow localisation, using vertical or horizontal parallax respectively. The axial inclination, apex location and the vertical and mesiodistal position of the canine relative to the incisor roots should be assessed. The permanent incisors should be checked carefully to exclude resorption, and the root length of the primary canine noted. Resorption of incisors is more common in females than males and there is a 50% greater risk of its occurrence should the canine be at a greater than 25° angulation to the midline when viewed on a dental panoramic tomogram. If incisor resorption is detected, urgent treatment is indicated. Removal of the impacted canine may arrest the resorption but extraction of the incisor may be required in those with severe resorption. Cone beam computed tomography (CBCT) can reveal the full extent of resorption.
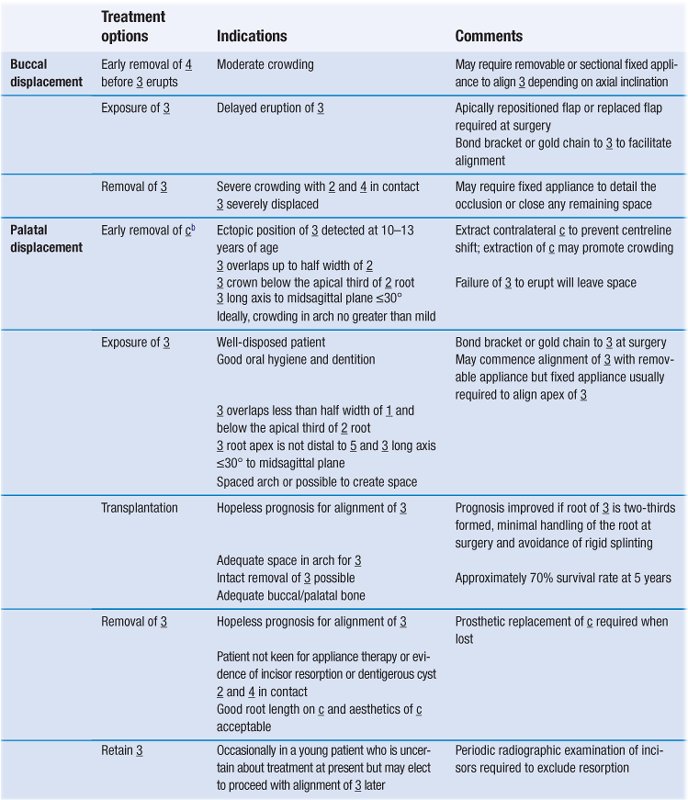
Management of canine displacement
The management of buccal or palatal maxillary canine displacement including transposition is described in Table 10.2.
Anomalies of size and form
Size
Teeth of a size that is greater or less than the norms for gender and for a given population are described as ‘megadont’ or ‘microdont’ respectively.
Megadontia has a prevalence of 1.1% in the permanent dentition, with maxillary central incisors most frequently affected, although lower second premolars are affected occasionally. The normal shape and absence of incisor notching distinguishes megadont maxillary incisors from ‘double teeth’. Megadont teeth may be found unilaterally on the affected side in unilateral facial hyperplasia, but more generalised megadontia is associated with gigantism. A megadont upper incisor may produce crowding, an increased overjet or both. If the tooth is only slightly enlarged, removal of about 1 mm of enamel from each proximal surface and appliance therapy to close the resultant space may suffice. In gross enlargement, extraction of the affected tooth and placement of a pontic following any appliance treatment may be necessary.
Microdontia is frequently seen in association with hypodontia, in Down syndrome and in ectodermal dysplasia. The prevalence is 0.2–0.5% in the primary dentition and 2.5% in the permanent dentition, with diminutive upper lateral incisors accounting for 1–2% of the latter. Short roots are often found on these teeth, which may be a factor in the aetiology of palatally displaced canines. In crowded mouths, where the lateral incisor is peg-shaped on one side of the arch and of normal size on the opposite side, removal of both lateral incisors may be optimal to achieve symmetry in the upper labial segment. If the diminutive lateral incisor is retained, orthodontic treatment should first create sufficient space to ensure that the tooth can be restored to normal dimensions. This space is maintained for at least 3 months with metal spurs on a removable retainer prior to final restoration.
Form
Double teeth
• Have a prevalence of 0.1–0.2% in the permanent dentition.
Clinical appearance can vary from an incisal notch in a tooth of enlarged mesiodistal width to an anomaly resembling two separate crowns. Treatment is best delayed until the pulp has receded. Separation may be possible if there are two separate pulp chambers and root canals, but recontouring of the crown to resemble two separate teeth or reduction of its mesiodistal width may be possible where one pulp chamber exists.
Prevalence in the primary dentition is 0.5–1.6% in Caucasians and it affects teeth mostly in the mandibular labial segment. In the presence of hypodontia, double primary teeth are followed usually by absence of permanent teeth, but supernumerary teeth are more common in the permanent dentition if all of the primary teeth are present. Occasionally, eruption of the permanent successor is delayed if a double primary tooth exists, and its removal, possibly in conjunction with that of permanent supernumeraries, may be indicated to allow eruption of the permanent teeth.
Accessory cusps and evaginated teeth
In the primary dentition, the maxillary molars are most commonly affected by additional cusps whereas the incisors, particularly the upper incisors, premolars and molars may be affected in the permanent dentition. An additional cusp on a maxillary incisor is termed a ‘talon’ cusp. As well as being unsightly, it may produce an occlusal interference or predispose to caries between the cusp and the palatal surface of the incisor. Treatment may be either by removal of the cusp and localised pulpotomy or by progressive grinding to encourage secondary dentine formation.
Evagination is characterised by a conical tuberculated prominence on the occlusal surface of a tooth and affects premolars most commonly. Treatment is as recommended for talon cusps.
10.2 Class I malocclusion
Aetiology
Skeletal factors
The skeletal pattern may be class I, class II or class III with the incisors compensating for any underlying skeletal discrepancy. An increase in lower anterior face height or a mild transverse skeletal discrepancy may also occur, creating an anterior open bite or buccal segment crossbite, respectively.
Soft tissues factors
Apart from bimaxillary proclination, where labial movement of the incisors may result from tongue pressure in the presence of unfavourable lip tone, the soft tissues are not prime aetiological factors.
Dental factors
A tooth/dental arch size discrepancy leading to crowding or spacing is the principal cause of class I malocclusion. Other factors, however, such as early loss of primary teeth, large or small teeth, supernumerary or absent teeth, can also influence any inherent dento-alveolar disproportion.
Occlusal features
There are several typical occlusal features:
Treatment
The need for treatment on dental health grounds is most commonly related to the presence of crowding or displacement of teeth; the latter may be caused by crowding, although ectopic developmental position, the presence of a supernumerary, retention of a primary tooth or, rarely, a pathological cause may be responsible. Treatment may be indicated also for spacing or for the management of vertical or transverse problems (see Sections 10.1 and 10.5).
Treatment planning
The basic principles of treatment planning have already been outlined in Section 9.4.
Crowding
The possible measures to be considered in relation to the management of crowding have been presented in Sections 9.4 and 10.1. Some basic guidelines, however, regarding the management of crowding in class I malocclusion are as follows:
• Late lower labial segment crowding occurs commonly in late teens and gradually increases throughout the third and fourth decades, representing largely an adaptation to growth changes in the facial skeleton. Other factors have also been implicated (see Table 9.2, p. 261), but the evidence associating the mandibular third molar with late lower incisor crowding is weak. Mild crowding is best accepted and monitored.
Bimaxillary proclination
Bimaxillary proclination (proclination of upper and lower incisors) is seen typically in Negros, where it can be regarded as normal, but it may occur also in Caucasians in association with class I, class II division 1 or class III malocclusions. In class I, the overjet is increased because of the incisor angulation. Treatment to retract the upper and lower labial segments is generally unstable, as lingual movement of the lower incisors away from their zone of labiolingual balance tends to relapse post-treatment unless retained permanently. The prospect of stability may be improved where the lips have good muscle tone and become competent following incisor retroclination. Where the soft tissue factors are unfavourable (e.g. grossly incompetent lips), treatment is inadvisable.
Spacing
In Caucasians, a generally spaced dentition is rare and is caused by a disproportion in the size of the teeth relative to the arch size or by absence of teeth. Where the spacing is mild, acceptance is usually best. Alternatively, consideration may be given to composite additions or porcelain veneers to increase the mesiodistal width of all the labial segment teeth. In more marked spacing, orthodontic treatment to concentrate the space at specific sites prior to fitting of a prosthesis or implant placement may be necessary.
Space between the upper central incisors is more common. Although this often exists in the early mixed dentition, it usually reduces considerably as the permanent maxillary canine erupts. Other factors that may cause an upper median diastema are given in Section 10.1. On average, the mesiodistal width of the upper lateral incisor is 80% that of the central incisor. Where the lateral incisor is narrower, it should be enlarged by composite or porcelain additions to assist maintenance of diastema closure.
In patients with missing upper permanent lateral incisors, the resulting space may be opened, closed or accepted (Section 10.1).
10.3 Class II malocclusion
Class II malocclusions are divided into divisions 1 and 2.
Division 1
Aetiology
The following factors contribute to the production of a class II division 1 malocclusion.
Skeletal relationships
Although the skeletal relationship is usually class II, class II division 1 malocclusion may exist on a class I or mild class III skeletal pattern. Where a class II skeletal pattern is present, mandibular deficiency is almost entirely the primary cause, although excessive maxillary growth or a combination of the two may be factors in other instances. In contrast, the developmental position or inclination of the teeth resulting from soft tissue or digit-sucking influences are to blame where the skeletal pattern is class I or mildly class III. The anterior vertical proportions of the face vary, and where these are greatly increased or reduced, treatment is likely to be difficult.
Lips, tongue and habits
The effects of the lips and tongue on the incisor position are determined principally by the skeletal pattern and thereafter by the manner in which an anterior oral seal is achieved. Where the skeletal pattern is class II, an acceptable incisor relationship may be achieved by proclination of the lower incisors under the influence of the tongue. In general, however, the greater the class II skeletal discrepancy, the more likely the lips are to be incompetent and to contribute to upper incisor proclination. Where lip incompetence exists along with a class II skeletal pattern and a reduced lower facial height, an anterior oral seal is likely to be produced by the lower lip lying under the upper incisors. This worsens the overjet by proclining the upper and retroclining the lower incisor teeth. In rare cases, the lower lip may be hyperactive and contribute to a class II division 1 malocclusion by solely retroclining the lower incisors. Where the lower facial height is increased, an anterior oral seal is often produced largely by forward positioning of the tongue, thus tending to reduce the overbite further and compensate for the class II discrepancy by proclining the lower incisors.
In very rare instances, a primary atypical swallowing behaviour will cause an overjet increase, but distinguishing this from an adaptive tongue thrust is difficult. The effect of a digit-sucking habit is to procline the upper incisors and retrocline the lower incisors although the overjet increase may be asymmetric depending on the positioning of the digit.
Occlusal characteristics
As forward mandibular posturing to disguise the overjet increase is seen in some patients, it is important to ensure that the mandible is in centric relation before recording the occlusal features.
Treatment
There is little need for treatment where the overjet is mildly increased and the arches are aligned (overjet 3.5–6 mm with competent lips; dental health component of the Index of Orthodontic Treatment Need (IOTN) (grade 2)). In such cases, the facial and dental appearance as well as the risks to dental health are minimal and acceptance of the malocclusion is reasonable. Where the overjet increase is between 6–9 mm or greater than 9 mm, the need for treatment on dental health grounds is great or very great, respectively. The factors that must be considered regarding any potential treatment are discussed in Section 9.4.
Special considerations in treatment planning
Skeletal pattern and profile
In general, the more the anteroposterior and vertical skeletal relationships deviate from normal, the more likely the profile is to be compromised and the more difficult treatment is likely to be. Where the nasolabial angle is obtuse or there is a marked ‘gummy smile’ or a short upper lip, treatment mechanics must ensure that overjet reduction does not worsen facial aesthetics; a combined orthodontic surgical approach may be best. Non-extraction treatment may be preferable to address mild-to-moderate crowding and avoid potential compromise to facial profile from extraction-based treatment.
Mandibular growth
The amount and pattern of mandibular growth can aid or detract from correction of a class II division 1 malocclusion in the growing patient. A forward mandibular growth pattern is favourable and is generally associated with situations where the lower facial height is reduced. A backward pattern of mandibular growth seen in individuals with increased lower facial height is unfavourable because the class II skeletal pattern is aggravated and the likelihood of lip competence post-treatment is reduced. In the non-growing patient, correction of both overbite and overjet of skeletal origin is difficult, and surgical correction may be required.
Form and relationship of the lips and tongue at rest and in function
It is important to assess the likely impact of the lips and tongue in the aetiology of the malocclusion and, more importantly, whether a stable correction is possible by altering or correcting their influence. As a digit-sucking habit may affect the swallowing pattern and the incisor position, it should be ceased before treatment commences.
Space requirements
Space is required in the lower and upper arches for overbite reduction and overjet correction, respectively (the former always preceding the latter), in addition to that needed for possible relief of crowding (see Section 9.4). On occasion, this may necessitate the loss of four units in the upper arch, usually where the lower labial segment is crowded and the buccal segment relationship is more than class II. Sometimes, in these cases, treatment may be started with a functional appliance to correct the molar relationship to class I, followed then by extractions for relief of crowding.
Where the lower arch is aligned, the buccal segment relationship typically half a unit class II and the overjet increase modest, space for overjet reduction may be obtained by moving the upper buccal segments distally using headgear or with the assistance of temporary anchorage devices (TADs) (screws or implants). Removal of the upper second permanent molars may be required.
Treatment in class I or mild class II skeletal relationship
Rarely, will treatment by tipping movements and upper removable appliance therapy alone be possible. Where the FMPA is average or slightly reduced, the arches are aligned and uncrowded and the upper incisors sufficiently proclined that, when the overjet is reduced, they will form no less than a 95° angle to the maxillary plane, then this may be considered. The highest quality outcome, however, is to be obtained with fixed appliances. Where occlusal factors (in particular, the inclination of the canines and maxillary incisors) are not amenable to tipping movements, fixed appliances are indicated (often in combination with extractions to allow relief of crowding) for correction of the incisor and buccal segment relationships. Removal of lower second and upper first premolars often favours the attainment of these occlusal goals. In the mixed dentition with a mild/moderate class II pattern, overjet reduction may be carried out using a functional appliance, although this is often followed by a phase of fixed appliance treatment, sometimes in combination with extractions, to optimise the final occlusal result (see Section 10.1).
Treatment in moderate-to-severe class II skeletal relationship
Three possibilities exist in relation to treatment in moderate-to-severe class II skeletal relationships.
Growth modification
Growth modification is only possible in the growing child. Ideally the arches should be uncrowded. Treatment should be undertaken just before and/or during the pubertal growth spurt. Success depends on creating a differential in the rate of growth of the maxilla and mandible. Depending on the relative contribution of maxillary prognathism or mandibular retrusion to the skeletal class II malocclusion, an attempt may be made to restrain horizontal and/or vertical maxillary growth, stimulate mandibular growth or both. While headgear restrains maxillary growth with forces of up to 1000 g in total, a functional appliance accelerates mandibular growth; the final mandibular size, however, with functional appliance treatment is little if any greater than it would have been without treatment. Wear of either headgear or a functional appliance or both for 14–16 hours per day, in conjunction with favourable growth, is necessary for a successful outcome. The correction achieved in the early mixed dentition with functional appliance or headgear has not been upheld long term; in addition, there were only minor, if any, differences following fixed appliance treatment in the permanent dentition between those who received early treatment and those allocated initially to the observation group. Consequently, in current practice, early treatment is only considered in those cases with psychosocial handicap.
When functional appliance treatment is planned, assessing standing height and secondary sexual characteristics assists in determining if a patient has begun the pubertal growth spurt. The stage of cervical vertebral maturation (CVM) viewed on a lateral cephalometric film has also been shown to be useful in assessment of optimal treatment timing. Following overjet correction, wear of the appliance as a retainer until growth has reduced to adult levels is required, unless a second phase of treatment to align the arches with fixed appliances and possibly extractions is considered.
Orthodontic camouflage
The skeletal discrepancy can be disguised by orthodontic tooth movement; this corrects the incisor relationship but the class II skeletal pattern remains. Invariably, treatment involves upper arch extractions, most commonly first premolars, and fixed appliance therapy to bodily retract the incisors. The effect of repositioning the teeth must not have a detrimental effect on the facial profile, otherwise ‘camouflage’ will have failed. Realistically this option is only acceptable where the class II skeletal pattern is no worse than moderate, the vertical facial proportions are good and the arches are reasonably well aligned so that the extraction spaces can be used for overjet reduction and not for relief of crowding. Where the lower incisors are retroclined by a habit, lip trap or deep overbite, it may be possible for them to be proclined by treatment and for this ‘camouflage’ to be stable.
Orthognathic surgery
Where growth is complete and camouflage would not produce optimal facial and dental aesthetics, surgical correction of the malocclusion is best (see Section 10.6). In such an individual, an overjet >10 mm is the best indicator that successful correction by camouflage is unlikely. This is especially so if the mandibular incisors are proclined relative to a short and deficient mandible and/or the total face height is increased.
Retention and post-treatment stability
The interincisal angle should be within normal limits, the overjet completely reduced with the upper incisors in soft tissue balance (i.e. no tongue thrust) and the lower lip covering at least one-third of their labial surface. Where these criteria are met, the prospect of stability is good. Retention planning is discussed elsewhere (see Section 11.4) but retention until growth is complete is required following functional appliance treatment.
Division 2
Aetiology
Skeletal relationships
The skeletal pattern in division 2 malocclusion is usually mildly class II, although it may be class I or mildly class III. A reduced lower facial height is common with an associated anterior mandibular growth rotation, which tends to increase the overbite. A relatively wide maxillary base may lead to a lingual crossbite of the first premolars.
Soft tissues
The high lower lip line (covering more than one-third of the upper incisor crowns) and resting pressure (about 2.5 times greater than that of the upper lip) are the most significant aetiological factors in retroclination of the upper incisors. The lower lip level depends largely on the lower anterior facial height; the more reduced the lower anterior facial height, the higher the lower lip line. Where the lower lip is also hyperactive, bimaxillary retroclination will result.
Dental factors
The upper incisor cingulum is often reduced or absent, which may exacerbate the overbite. In addition, there is an increased likelihood of the teeth being smaller than normal, as is the chance of a more acute crown/root angulation. Retroclination of the upper, and commonly of the lower, incisors also makes existing crowding worse.
Occlusal features
The main occlusal features are the following:
Treatment
Treatment planning
The following factors in particular must be considered in relation to treatment planning.
The underlying skeletal discrepancy, both anteroposteriorly and vertically
In general, the more class II the skeletal pattern and the lower the FMPA, the more difficult treatment is likely to be to achieve a normal incisor relationship.
The growth potential and pattern of facial growth
In a growing patient, correction of both a class II skeletal pattern and deep overbite is facilitated by favourable facial growth. Although a forward mandibular growth rotation aids correction of a class II skeletal discrepancy, it tends to increase the overbite.
Profile considerations
Occasionally, a non-extraction approach may be adopted, usually in those with bimaxillary retroclination, to prevent the proposed risk of adverse profile change that may result from an extraction-based plan. There is, however, little difference in lip fullness with either approach. When the profile is particularly unfavourable in an adult, usually with a marked class II pattern and very reduced FMPA, a combined orthodontic/surgical approach will be required.
The presence and degree of crowding
Lower arch extractions should only be considered where the crowding is marked. There is a risk of a deep overbite becoming traumatic as the lower incisors are allowed to drop lingually if extractions are undertaken in the presence of mild-to-moderate crowding. In addition, as the lower labial segment is constricted by the upper labial segment, some stable expansion of the lower intercanine width and proclination of the lower incisors may be feasible, thereby providing space for relief of mild-to-moderate crowding. Where extractions are necessary, a lower fixed appliance should be used to close residual spacing and prevent retroclination of the lower labial segment. In these cases, consideration should be given also to upper arch extractions and correction of the incisor relationship.
The lower lip level
Where the lower lip level is at the gingival third of the upper incisor crowns or higher, correction of the incisor relationship without recourse to indefinite retention is unlikely.
The depth of overbite and inclination of the upper incisors
The depth of overbite and the inclination of the upper incisors determine the two approaches to treatment: either acceptance or correction of the incisor relationship.
Overbite reduction may be achieved by various means, including:
In addition, proclination of the upper incisors, followed by a functional appliance to correct the overjet created, will reduce the overbite.
In a growing patien/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 are calcifying (aged approximately 8.5–9.5 years) and moderate premolar crowding is present.
are calcifying (aged approximately 8.5–9.5 years) and moderate premolar crowding is present. s erupt.
s erupt.