10
Oral Anatomy and Physiology
- the gross anatomy of the tissues and structures of the oral cavity
- the microscopic anatomy of teeth and their supporting structures
- the functions of the tissues and structures of the oral cavity
- the morphology and functions of teeth
- the salivary glands
The oral cavity contains many anatomical structures besides the teeth, and to gain a full understanding of the topics of oral health and disease, the dental nurse must have knowledge of all these structures. The bones, muscles, nerves and blood supply to this region are discussed in Chapter 9; this chapter will focus on the following specific anatomical structures and their physiology.
- Oral soft tissues and soft palate.
- Tongue.
- Teeth.
- Supporting structures of the periodontium.
- Salivary glands.
Soft tissues of the mouth
Epithelial membrane
The whole of the mouth is lined with epithelial mucosal tissue as a type of mucous membrane, which is continuous with that lining the digestive tract. Throughout the oral cavity there are three types of this membrane, each with its own particular features.
- Lining membrane.
- Masticatory membrane.
- Specialised membrane.
Their details are shown in Table 10.1. The first row identifies the area of the oral cavity where each type of epithelial membrane is normally found, while the second row describes its appearance in each case. The final row explains the function(s) of the membrane in relation to its appearance – so the ridged nature of the masticatory membrane, for example, and its firm underlying attachment are explained by its function of providing a hard-wearing surface that can withstand the regular abrasive contact it has with food.
Within the oral cavity, the space between the posterior teeth and the mucous membrane lining the cheeks is called the buccal sulcus whilst that between the anterior teeth and lips is the labial sulcus. The upper lip is attached to the centre of the gingiva above the central incisors by a band of fibrous tissue called a frenum, and when this attachment is thicker than usual, there is often a space created between the two incisor teeth, called a median diastema.
Table 10.1 Oral mucous membranes
| Lining membrane | Masticatory membrane | Specialised membrane |
| Covers inner surfaces of the cheeks and lips, floor of the mouth, underside of the tongue, soft palate | Covers gingivae, topside and edges of the tongue, hard palate | Interspersed throughout the masticatory membrane covering of the topside and edges of the tongue |
| Appears as red, smooth and moist membrane, which can be squashed and stretched Contains minor salivary glands |
Appears as red, moist membrane, often ridged or stippled, firmly attached to underlying structures – forms the mucoperiosteum where it lies over the alveolar processes | Appear as discrete papillary structures of the taste buds, in a visible pattern over the tongue |
| Provides a physical barrier between anything entering the mouth and the deep structures of the oral cavity, acts as a cushion, provides lubrication and cleansing | Provides a hard-wearing surface that prevents traumatic damage from food, chemicals, oral hygiene products, etc. | Provides taste sensation |
Figure 10.1 Tonsils and oropharynx.

Soft palate
The soft palate is a flap of soft tissue attached to the back of the hard palate. Its function is to seal off the oral cavity from the nasal cavity during swallowing, in order to prevent food passing up into the nose. The free edge of the soft palate has a central prolongation called the uvula. You can see this for yourself by looking in a mirror with your mouth wide open. To either side of this area at the back of the mouth, called the oropharynx, lie the tonsils which appear as small ball-like structures with a pitted surface (Figure 10.1). They are most noticeable when inflamed during a throat infection, such as tonsillitis.
Tongue
The floor of the mouth lies within the arch of the mandible and is occupied by the tongue, which is a muscular organ situated in the oral cavity and also the throat. The posterior one-third section, the base of the tongue, lies in the throat and attaches to the floor of the mouth. It is relatively firmly attached and is mainly concerned with swallowing movements. The correct term for swallowing is deglutition.
The remaining anterior two-thirds of the tongue, the body, lie within the oral cavity and this section is relatively moveable, being able to perform numerous convoluted movements, as it is composed of many bands of muscle lying in various directions. It is attached to the floor of the mouth by a thin band of fibrous tissue called the lingual frenum. Where excess of this fibrous tissue occurs, the tongue is held more rigidly than normal so that its movements are restricted, and the person affected is often described as ‘short-tongued’ or ‘tongue-tied’, due to the lisp created as they speak.
The body of the tongue is concerned with taste, chewing activities and speech.
All the muscles of the tongue are innervated by the hypoglossal nerve (12th cranial nerve).
The functions of the tongue are as follows.
- Speech – by allowing certain sounds to be created by touching the tongue to the upper anterior teeth or the palate (such as ‘s’, ‘t’, ‘n’, ‘the’).
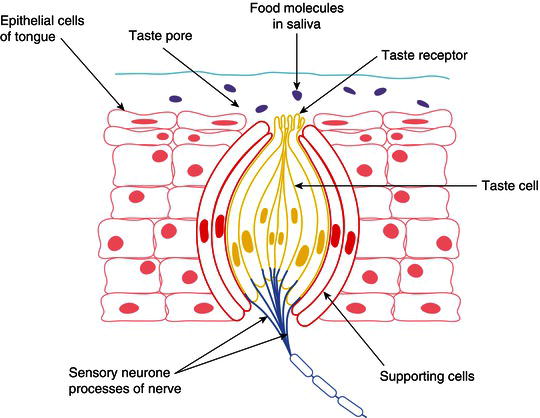
- Taste – the tongue is covered by various different types of taste buds (including filiform papillae, fungiform papillae and vallate papillae – Figure 10.2) that allow recognition of the four basic tastes – sweet, sour, salt and bitter.
- Aids mastication – by assisting the buccinator muscles to package ingested food into a parcel, or bolus, for easier chewing before swallowing.
- Aids swallowing – by guiding the bolus to the back of the mouth, the oropharynx.
- Cleansing – by moving around the oral cavity and the smooth surfaces of the teeth to dislodge food particles.
Figure 10.2 Taste bud.
The lining epithelium of mucous membrane covering the underside of the tongue is so thin that it allows the very rapid absorption of drugs placed here into the underlying capillaries of the tongue. Patients given glyceryl trinitrate (GTN) tablets or spray for the treatment of angina pectoris use their medications in this way.
Swallowing
Swallowing is a complex muscular action which aims to direct the food bolus into the oesophagus while also preventing it from entering the nasal cavity or the larynx. The bolus is mixed with saliva to lubricate it, and then propelled by the tongue from the mouth to the oropharynx, and then into the oesophagus. The sequence of events in the swallowing process is as follows (see Figure 5.11).
- The lubricated ball of food is propelled backwards to the oropharynx by the actions of the body of the tongue.
- The soft palate rises up and seals off the nasopharynx from the oropharynx, to prevent the bolus from passing upwards into the nose.
- At the same time, the larynx lifts up and is sealed by the epiglottis to prevent the bolus passing into the trachea and being inhaled into the lungs.
- The bolus is propelled downwards from the oropharynx by the base of the tongue, and to the oesophagus by the throat muscles.
- Oesophageal muscles then move the bolus downwards by peristalsis into the stomach.
Disorders of the tongue
Glossitis
This is soreness and inflammation of the tongue, and can occur in conditions such as anaemia, vitamin B deficiency and hormonal disturbances (including pregnancy). It is associated with a thin, smooth glazed appearance of the normally thick layer of mucous membrane on its upper surface.
Dysphagia
This is the condition of having difficulty in swallowing, which occurs relatively frequently and has several causes.
- Psychological – an inability to swallow (usually) medication in tablet form, although food and drink can be swallowed normally by the patient.
- Xerostomia – dry mouth syndrome, where reduced salivary flow prevents adequate bolus lubrication.
- Oesophagitis – inflammation of the oesophagus, often due to acid reflux.
- Other conditions affecting pharyngeal or oesophageal function, including cancers.
- Central nervous system disorders preventing correct muscle innervation, such as stroke and multiple sclerosis.
Teeth
The teeth are the anatomical structures within the oral cavity that are of the greatest relevance to the dental team, as their development, health, disease and restoration are the fundamentals of dentistry. The teeth have the following functions.
- To cut up and masticate food into suitable sized portions before swallowing.
- To expose the food surfaces to enzymes and allow digestion to begin.
- To support the oral soft tissues of the cheeks and tongue, and therefore enable clear speech.
Humans have two sets of teeth – the primary (deciduous) teeth of childhood and the secondary (permanent) teeth of adulthood. The number and type of teeth in each set differ, although the shape of the common ones is the same.
The detailed anatomical shape of each tooth, and its function, is called tooth morphology.
The four types present in the secondary dentition, from the midline of the mouth posteriorly, are as follows.
- Central and lateral incisors
- Canine
- First and second premolars
- First, second and third molars
The primary dentition has just two molars and is made up of just three different types of teeth – there are no premolars present.
Figure 10.3 Structure of a tooth.
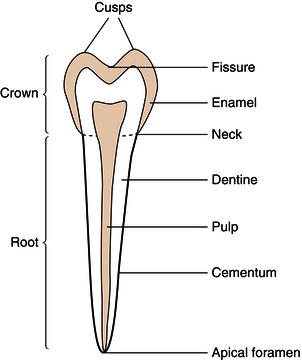
Each tooth of all types, and in both sets, has three sections – the crown, the neck and the root(s). The crown is the section of the tooth visible in the oral cavity, following its eruption from the underlying alveolar bone. The neck is the section where the tooth and the gingival tissues are in contact with each other at the point where the tooth emerges through the gums, and the root is the (usually) non-visible section that holds the tooth in its bony socket.
All teeth are composed of the same four tissues.
- Enamel – a highly calcified tissue covering the whole crown of the tooth.
- Dentine – a less calcified tissue than enamel, which forms the inner bulk of the crown and root.
- Cementum – a thin calcified covering of the root dentine only.
- Pulp – the inner neurovascular tissue of the tooth, within the central pulp chamber.
The structure of a typical tooth is shown in Figure 10.3.
Microscopic structure of the teeth
The differences in the microscopic structure of the four layers of the teeth are what determine how they function, how they develop disease, how they are treated for that disease, and how they are restored or extracted by the dental team.
Enamel
This is the highly calcified, protective outer covering of the crown and is the hardest substance in the body. Its properties and microscopic structure are as follows.
- It is made up of 96% mineral crystals (inorganic) arranged as prisms in an organic matrix called the interprismatic substance.
- The main mineral crystals are calcium hydroxyapatite.
- The prisms lie at right angles to the junction with the next tooth , the dentine.
- The junction between these two layers is called the amelodentinal junction (ADJ).
- Enamel is formed before tooth eruption by the ameloblast cells, which lie at the ADJ.
- It contains no nerves nor blood vessels and therefore cannot experience any sensation.
- It is a non-living tissue which cannot grow and repair itself, so progressive damage caused by injury or tooth decay is permanent.
- It can, however, remineralise its surface after an acid attack, by taking in minerals from saliva and from oral health products such as toothpaste and mouthwash.
- The crystal structure can also be altered without undergoing acid attack, by the exchange of hydroxyl ions in the hydroxyapatite with fluoride, to form fluorapatite crystals – these make the enamel surface harder and more resistant to acid attack.
- The enamel layer is thickest over the biting surface of the tooth (the occlusal surface or the incisal edge) and thinnest at the neck of the tooth (the cervical margin).
- It is translucent, so the shade of a tooth is determined by the colour of the underlying dentine.
Dentine
This tissue forms the main bulk of a tooth and occupies the interior of the crown and root. It is also mineralised, but to a lesser extent than enamel, and is covered by enamel in the crown of the tooth and by cementum in the root of the tooth. Its properties and microscopic structure are as follows.
- It consists of up to 80% inorganic tissue, mainly calcium hydroxyapatite crystals.
- It is composed of hollow tubes which originally surrounded the cells within the dentine structure as it was first being formed.
- In a fully formed tooth, these odontoblast cells lie along the inner edge of the pulp chamber only, but are present throughout life and can lay down more dentine as required.
- In this way, it can repair itself by laying down secondary dentine.
- This type of dentine is also formed as part of the natural ageing process, and its formation gradually narrows the pulp chamber.
- The hollow tubes contain sensory nerve endings called fibrils, which run from the nerve tissue within the pulp chamber.
- Dentine is therefore a living tissue and can transmit sensations of pain and thermal changes to the brain.
- Its hollow structure allows it a degree of elasticity so that it can absorb normal chewing forces without breaking.
- However, it also allows tooth decay (caries) to spread more rapidly through its hollow structure.
- Dentine is a yellowish colour, and gives teeth their individual shade.
Cementum
This is the calcified protective outer covering of the root and is similar in structure to bone. Cementum meets enamel at the neck of the tooth, and normally lies beneath the gingivae. Its properties and microscopic structure are as follows.
- Around 65% mineralised, with calcium hydroxyapatite crystals.
- The crystals lie within a matrix of fibrous tissue, with the ends of collagen fibres from the periodontal ligament inserted into the outer layer of the cementum.
- This allows the attachment of the root to the periodontal ligament, and therefore to the walls of the tooth socket.
- The cementum is formed by cells called cementoblasts and they can continue laying down more tissue layers when required.
- The thickness of cementum may vary at different parts of the root, and changes throughout life, depending on the forces exerted on individual teeth.
- The cementum contains no nerves nor blood vessels itself, so it receives nutrients from the periodontal ligament.
Pulp
Unlike enamel, dentine and cementum, the pulp contains no mineral crystals and is composed purely of soft tissue. It lies within the very centre of every tooth, from the crown as the coronal pulp and into each root as the radicular pulp. The radicular pulp is often referred to as the ‘root canal’ of the tooth. The properties and microscopic structure of the pulp are as follows.
- The pulp contains sensory nerves and blood vessels.
- The sensory nerves are end sections of the trigeminal nerve (fifth cranial nerve), either as the inferior dental nerve for the lower teeth or one of the superior dental nerves for the upper teeth.
- They allow the tooth to feel hot, cold, touch and pain by the stimulation of its sensory nerve endings which run as fibrils in the hollow dentine tubules.
- These pulp tissues enter the tooth through the apical foramen, lying at the root apex of every tooth.
- The pulp chamber itself is lined by the odontoblast cells which form dentine.
- The chamber gradually narrows with age, so that it can become completely obliterated in older patients, making endodontic treatment very difficult.
- It can also become blocked by pulp stones which are formed by lumps of calcium-containing crystals.
- The point where the cementum and the root dentine are in contact with each other is called the dentinocemental junction.
- Some teeth have additional contact between the pulp and the surrounding periodontal ligament via accessory canals, whose presence can make successful endodontic treatment of the tooth very difficult to achieve.
Tooth morphology
All people have two sets of teeth: the first or deciduous teeth, and the second or permanent teeth. All have different appearances or morphology, which depends on the set and the individual teeth themselves. Their morphology enables each tooth to be individually identified by any trained/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


