10
Molar Uprighting and Space Regaining
Introduction
The dentist who removes either a primary or a permanent tooth or observes a patient shortly after the loss of a tooth has an obligation to inform the patient or parent of the likelihood that teeth adjacent to an extraction site will move in an unfavorable manner. Most of the unfavorable tooth movement occurs in the arch from which the tooth is removed; however, teeth in the opposing arch can also overerupt into the extraction site. In many patients who lose primary molars or permanent teeth, the unfavorable movement of teeth adjacent to the extraction site will require orthodontic treatment to restore good occlusion and prepare the patient for prosthesis. After the adjacent teeth have moved in an undesirable manner, the orthodontic recapture of lost arch length may not fully restore the original arch length. In summary, the time and expense of orthodontic treatment will far exceed the time and expense to prevent undesirable tooth movement adjacent to an extraction site. Space maintenance appliances include the lingual holding arch, a palatal holding arch, and the Hawley retainer.
Ectopic Eruption of Permanent First Molars
In 3% to 4% of the American population, permanent first molars erupt ectopically (Kimmel, Gellin, Bohannan, and Kaplan 1982). Ectopic eruption has a familial tendency, occurring more frequently (19%) in siblings (Kurol and Bjerklin 1982). The phenomenon occurs more frequently (25%) in children with cleft lip and palate (Carr and Mink 1965). Maxillary molars are more frequently affected by ectopic eruption than are mandibular molars (Young 1957). In a study of 315 children, the frequency of ectopic eruption was 8% of the sample for maxillary molars and less than 1% for mandibular molars (O’Meara 1962) One-half of the patients present with unilateral ectopic eruption, and one-half, bilaterally (Young 1957). Ectopic eruption of first molars does not differ by gender or race (Kimmel et al. 1982).
Ectopically erupting molars fall into two types: reversible (self correcting) and irreversible. The frequency of the reversible type was reported as 66% in an American sample of 1,619 children (Young 1957) and as 59% in a sample of 2,903 Swedish children (Kurol and Bjerklin 1986). Only a few of the ectopic permanent first molars seen at age 7 and older became reversible (Bjerklin and Kurol 1981). Based on this evidence, we conclude that after the age of 7, the vast majority of patients will experience irreversible ectopic eruption and treatment can proceed to correct the problem. Self-correction and eruption are considerably less frequent in cleft lip and palate patients (Carr and Mink 1965). Non–cleft children under the age of 7 with ectopic molars should be observed to allow time for the molar to self-correct.
Two studies found that patients with ectopically erupting maxillary molars often lack adequate arch length and have a retropositioned and smaller-than-normal maxilla (Canut and Raga 1983; Pulver 1968). One study found that three factors differentiated the irreversible ectopic eruption patients from those with normal eruption: the ectopic group had (1) a steeper angle of eruption, (2) a larger permanent first molar width, and (3) a tendency for a shorter maxilla (Bjerklin and Kurol 1983). Two early review articles summarize ectopic eruption and discuss clinical management of the problem (Kennedy and Turley 1987; Kurol and Bjerklin 1986).
The distal surface of the primary molar may be resorbed in varying degrees by the ectopically erupting permanent molar crown. In some instances, the ectopic permanent first molar resorbs most of the primary molar’s roots, causing premature exfoliation of the primary second molar and eruption of the first molar into the arch space needed by the second premolar. Barberia-Leache, Suarez-Clua, and Saavedra-Ontiveros (2005) described four grades of magnitude for lesions in maxillary primary second molars caused by an ectopically erupting permanent first molar: (1) Grade I [mild] involved limited resorption of cementum and dentin; (2) Grade II [ moderate] involved resorption of the dentin without pulp exposure; (3) Grade III [severe] involved resorption of the distal root leading to pulp exposure; Grade IV [very severe] involved resorption that affects the mesial root of the primary second molar. The grades are illustrated in Figure 10.1.
Figure 10.1. Grades for the magnitude of lesions in maxillary primary second molars caused by ectopically erupting first molars.
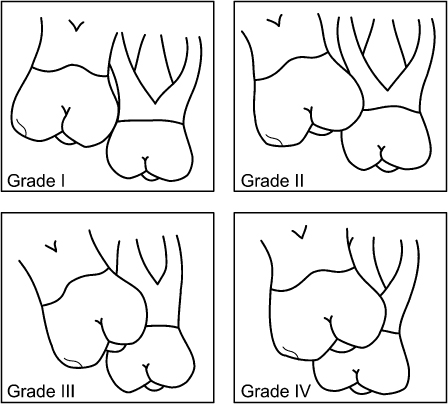
Barberia-Leache et al. (2005) reported that 4.3% of 509 consecutive Spanish patients between 6 and 9 years old experienced ectopic eruption of maxillary first molars. No gender difference was found. Ectopic eruption occurred unilaterally in 36.4% and bilaterally in 63.6% of the patients, which are not significantly different occurrences. In the unilateral occurrence patients, significantly more ectopic molars were found on the right side than on the left side. Of the 36 ectopic molars in 22 children, 69% were reversible and 31% were irreversible. The majority of Grade I and II molars were reversible and the majority of Grade III and IV molars were irreversible. Some Grade III molars were reversible and some Grade I molars were irreversible.
Early detection of the ectopic eruption of a maxillary permanent first molar and radiographic examination of the problem will help determine the best approach to the problem. Periodic observation is appropriate in younger patients, while patients older than 7 years require treatment.
Uprighting Molars in the Mixed Dentition
The premature loss of a primary second molar because of ectopic eruption of the permanent first molar or because of caries is usually accompanied by the mesial tipping of the adjacent permanent first molar. The erupted first molar then impacts the adjacent nonerupted second premolar. When the problem occurs with an upper permanent first molar, the molar occlusion becomes Class II, and when the problem occurs with a lower first molar, the molar occlusion becomes Class III. In both cases, an asymmetric malocclusion develops unless the problem occurs bilaterally. If these problems are not treated in the mixed dentition, they will probably require orthodontic treatment in the permanent dentition. A panoramic radiograph of a 10-year 4-month-old male patient is shown in Chapter 5, Figure 5.6; in which a lower right permanent first molar is tipped forward over an ankylosed primary second molar that in turn has prevented the eruption of a developing second premolar. In Chapter 5, Figure 5.9, the loss of a primary second molar in an 8-year-old girl has allowed the upper first molar to move forward and impact her upper right second premolar. In Chapter 5, Figure 5.10, a 9-year 7-month-old girl has prematurely lost a lower left primary second molar that allowed the first molar to move forward and impact the lower left second premolar.
Ectopic Eruption of Upper First Molars
A boy aged 9 years 2 months presented with the premature loss of his upper right primary second molar (Figs. 10.2 and 10.3). He had a Class II subdivision right malocclusion with his upper right permanent first molar in a Class II relationship with his lower right permanent first molar. The mesial shifting of his upper first molar impacted his nonerupted upper right second premolar (Figs. 10.3 and 10.4). After the eruption of his upper right first premolar, a removable appliance was constructed with a helical finger spring to move the upper molar distally into a Class I relationship (Fig. 10.5). The patient lost his removable appliance after wearing it for 2 months. An edgewise fixed appliance was made to complete the distal movement of the first molar. After receiving the fixed appliance, the patient said that he wished he had not lost his removable appliance! A Nance palatal holding arch retained the regained arch length. At age 10 years 2 months his occlusion is seen after the eruption of his upper second premolar (Figs. 10.6 and 10.7).
Figure 10.2. Patient with premature loss of his upper right primary second molar.

Figure 10.3. Bite wing radiograph showing the impacted upper right second premolar.

Figure 10.4. Occlusal view of the upper arch with the mesially displaced right permanent first molar.

Figure 10.5. Shamy removable appliance was made to move the right first molar distally.

Figure 10.6. The occlusion on the right side is shown after the eruption of the upper right second premolar.

Figure 10.7. Occlusal view of the erupted upper right second premolar is shown.

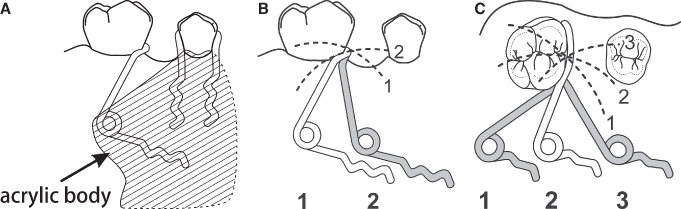
The prescription for making the removable appliance is shown in Figure 10.8. The helical coil finger spring for this patient was made from 21 × 28 mil rectangular wire after the design of Shamy (1972). The helix of the spring has a diameter of 2 to 3 mm, is located 8 mm above the lingual gingival margin, and is centered above the middle of the molar crown (Fig. 10.9A). The Shamy appliance was stabilized with Adams clasps on the upper first premolars and the upper left first molar (Adams 1984). The arrowheads of the clasps are adjusted to grip the anchor teeth very tightly, to hold the anchor teeth together and resist the force exerted by the finger spring. An anterior bite plate on the appliance opens the bite 1 to 2 mm to facilitate the movement of the upper molar. The spring is activated by opening the helix with No. 139 bird beak pliers. The arm of the finger spring is activated distally to about the middle of the occlusal surface of the first molar. The arm of the spring is kept as close as possible to the gingival tissues adjacent to the mesial surface of the tooth so the force exerted by the spring is near the center of resistance of the first molar. During activation, the correctly positioned spring arm (Fig. 10.9B, 1) moves occlusally along an arc determined by the helical coil spring (Fig. 10.9B). This movement requires periodic adjustment of the clasp arm to keep it in contact with the gingival part of the crown. The spring must engage the mesiolingual surface of the molar to guide the tooth distally and buccally along the arch without moving it lingually into crossbite (Fig. 10.9C). The correct position of the uprighting spring is illustrated in Figure 10.9C, 2. Treatment time to move a molar distally 4 mm is about 4 months, assuming 1 mm per month of tooth movement (Iwasaki, Crouch, Reinhardt, and Nickel 2004).
Figure 10.8. Laboratory prescription for an upper Shamy molar uprighting appliance.
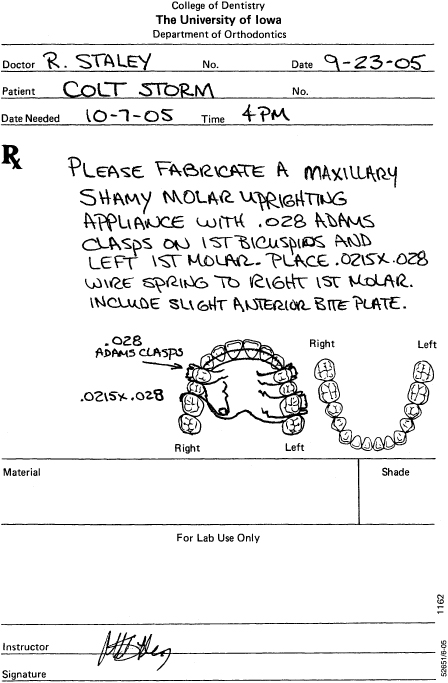
Figure 10.9. Shamy molar distalizing spring: palatal view (A), effect of anteroposterior position of the helix on vertical movement of the spring (B), and effect of the anteroposterior position of the helix on buccolingual movement of the spring (C).
Another boy aged 5 years 10 months presented with both upper permanent first molars erupting ectopically (Figs. 10.10 through 10.15). A panoramic radiograph (Fig. 10.11) shows his right molar is a Grade IV impaction and his left molar (Fig. 10.13) is a Grade III impaction (Barberia-Leache et al. 2005). The upper primary second molars were extracted to allow eruption of the permanent first molars after considering the great degree of resorption of the roots of the upper primary second molars. After the permanent first molars were sufficiently erupted, a fixed appliance was placed on the upper teeth to move the first molars distally with trapped coil springs delivering moderate forces (Figs. 10.16 and 10.17). After the upper molars were moved to a Class I occlusion, the molars were retained with a Nance palatal holding arch (Figs. 10.18 and 10.19). The patient is shown at 10 years of age after his second premolars had erupted (Figs. 10.20 and 10.21).
Figure 10.10. Front view of the occlusion.

Figure 10.11. Pretreatment panoramic radiograph showing the ectopic eruption of the upper permanent first molars.
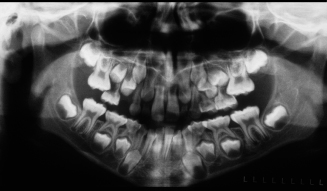
Figure 10.12. View of the teeth on the right side.

Figure 10.13. Grade III impaction of the upper permanent first molar is shown in this radiograph.

Figure 10.14. Occlusal view of the teeth in this patient.

Figure 10.15. Occlusal view of the patient’s upper cast illustrates the impaction of both permanent first molars.
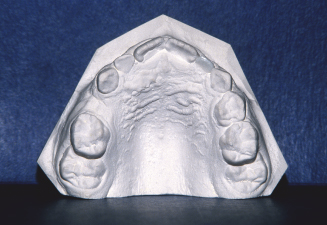
Figure 10.16. Front view of the fixed appliance used to move the upper first molars distally.
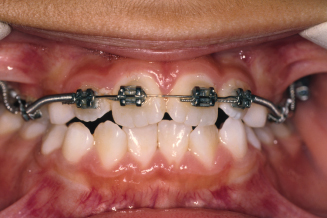
Figure 10.17. Occlusal view of the fixed appliance showing the coil springs that pushed the first molars distally.

Figure 10.18. Front view of the teeth after the fixed appliance was removed.

Figure 10.19. Occlusal view showing the palatal holding arch retainer.
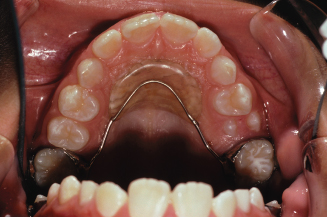
Figure 10.20. Front view of the teeth after the premolars were erupted.

Figure 10.21. Occlusal view of the upper arch showing the erupted premolars and palatal holding arch.

Ectopic Eruption and Tipping of Lower First Molars
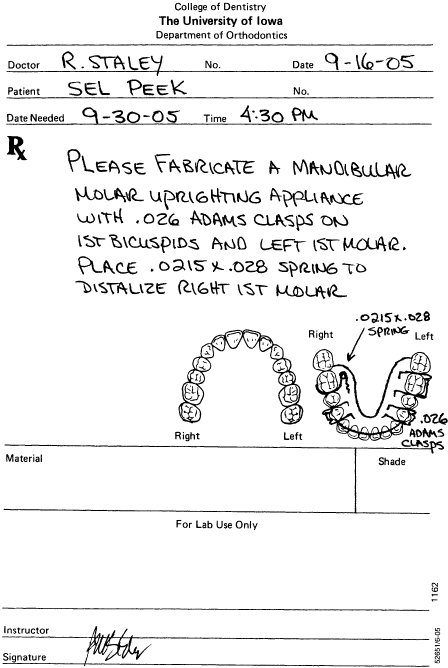
An 8-year 6-month-old girl lost her lower primary second molars, and presented soon after the loss of her lower left primary second molar. The left permanent first molar was in good position; however, the lower right first molar had drifted forward (Fig. 10.22). A mandibular removable Shamy (1972) appliance was given to the patient (Fig. 10.23). The mandibular spring was made from 21 × 28 mil rectangular wire. The spring is shown in Figures 10.24 and 10.25. The spring would operate as described earlier for the maxillary Shamy appliance. A laboratory prescription for the appliance is shown in Figure 10.26. The patient would not wear the appliance and stopped coming for orthodontic appointments. Had this appliance regained arch length, it would have been replaced with a lower lingual holding arch to maintain arch length for the eruption of the premolars and canines.
Figure 10.22. The lower arch of a patient with a mesially displaced lower right permanent first molar.

Figure 10.23. Removable Shamy appliance was made to regain arch length.
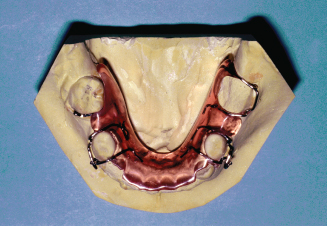
Figure 10.24. Adams clasps and helical finger spring of the appliance are shown.
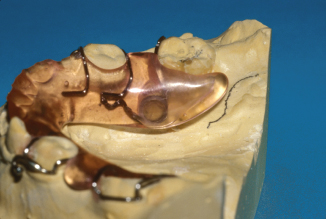
Figure 10.25. Helical spring is shown from the lingual side of the appliance.

Figure 10.26. Laboratory prescription for a lower Shamy molar uprighting appliance.
A 9-year 11-month-old girl presented with the early loss of a lower left primary second molar resulting in the impaction of her lower left second premolar and a Class III subdivision left malocclusion (Figs. 10.27 through 10.30). In Figure 10.27, the deviation of the lower dental midline to the left side can be seen. The periapical film in Figure 10.30 shows the impaction of the lower left second premolar and a favorable space between the lower left first and second molars that can be used to move the lower first molar distally. The patient’s pretreatment panoramic radiograph is shown in Chapter 5, Figure 5.10. A fixed edgewise appliance was used to move the lower left first molar distally (Figs. 10.31 through 10.34). The appliance used a trapped coil spring to move the lower left first premolar mesially and the lower left first molar distally (Figs.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


