Oral and Maxillofacial Radiology
• Multilocular Radiolucent Lesion in the Pericoronal Region (Keratocystic Odontogenic Tumor [Odontogenic Keratocyst])
• Unilocular Radiolucent Lesion of the Mandible
• Multilocular Radiolucent Lesion in the Periapical Region (Ameloblastoma)
• Unilocular Radiolucent Lesion in a Periapical Region (Periapical Cyst)
Figure 1-1 shows the most common location of several radiographically detectable maxillofacial pathologic processes.
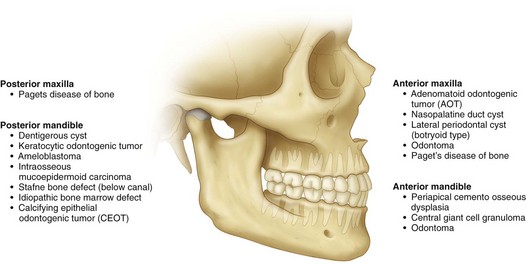
Figure 1-1 The most common location of several radiographically detectable maxillofacial pathologic processes.
Multilocular Radiolucent Lesion in the Pericoronal Region (Keratocystic Odontogenic Tumor [Odontogenic Keratocyst])
CC
A 20-year-old man is referred for evaluation of a swelling on his right mandible.
MHX/PDHX/Medications/Allergies/SH/FH
Noncontributory. There is no family history of similar presentations.
Nevoid basal cell carcinoma syndrome (NBCCS) is an autosomal dominant inherited condition with features that can include multiple basal cell carcinomas of the skin, multiple KCOTs, intracranial calcifications, and rib and vertebral anomalies. Many other anomalies have been reported with this syndrome (Box 1-1). The prevalence of NBCCS is estimated to be 1 in 57,000 to 1 in 164,000 persons.
Examination
Thorax-abdomen-extremity. The patient has no findings suggestive of NBCCS (e.g., pectus excavatum, rib abnormalities, palmar or plantar pitting, and skin lesions; see Box 1-1).
Imaging
In this patient, the panoramic radiograph reveals a large, multilocular radiolucent lesion with possible displacement of the right mandibular third molar (Figure 1-2). There are also several carious teeth and a retained root tip of the right mandibular second bicuspid (tooth #29). (In a patient with a radiolucent lesion of the mandible presumed to be an odontogenic cystic lesion, a multilocular appearance is associated with a 12-fold increased risk for the diagnosis of KCOT; however, the presence of a unilocular lesion does not exclude the possibility of a KCOT diagnosis.)
Differential Diagnosis
The differential diagnosis of multilocular radiolucent lesions can be divided into lesions of cystic pathogenesis, neoplastic (benign or malignant) lesions, and vascular anomalies (least common). The differential diagnosis of multilocular radiolucent lesions is presented in Box 1-2 and can be further narrowed by the clinical presentation. Special consideration should be given to radiolucent lesions with poorly defined or ragged borders, which have a separate differential.
Treatment
Options that have been used to treat KCOTs include the following:
• Decompression by marsupialization
• Marsupialization followed by enucleation (surgical decompression of the cyst, followed by several months of daily irrigation with chlorhexidine via stents secured in the cystic cavity, followed by cystectomy)
• Enucleation with curettage alone
• Enucleation followed by chemoablation or cryotherapy
• Enucleation with peripheral ostectomy
• Enucleation with peripheral ostectomy and chemoablation or cryotherapy
Discussion
Identification of individuals who may have NBCCS allows the clinician to arrange for appropriate referrals. NBCCS should be suspected when multiple lesions exist. The diagnosis is confirmed upon finding any two of the major criteria, or one major criterion plus two minor criteria (see Box 1-1). Some abnormalities are pertinent only to the diagnosis and do not require any specific therapy. Other abnormalities may pose further risk to the patient and require the input of other specialists. Spina bifida and central nervous system tumors require referral to a neurosurgeon. In addition, genetic counseling for all patients afflicted with NBCCS is recommended. KCOTs associated with this syndrome are treated in the same manner as an isolated KCOT; however, these lesions have a higher rate of recurrence when associated with NBCCS (which may represent new lesions). KCOTs are often associated with the follicle of a potentially functional tooth and, when possible, marsupialization with orthodontic guidance should be considered.
August, M, Caruso, PA, Faquin, WC. Report of a case: an 18-year-old man with a one-month history of nontender left mandibular swelling. N Engl J Med. 2005; 353:2798–2805.
August, M, Faquin, WC, Troulis, M, et al. Differentiation of odontogenic keratocysts from nonkeratinizing cysts by use of fine-needle aspiration biopsy and cytokeratin-10 staining. J Oral Maxillofac Surg. 2000; 58:935–940.
Barnes L, Eveson JW, Reichart P, et al, eds. Pathology and genetics: head and neck tumours (IARC World Health Organization classification of tumors). Lyon, France: IARC Press, 2005.
Buckley, P, Seldin, E, Dodson, T, et al. Multilocularity as a radiographic marker of the keratocystic odontogenic tumor. J Oral Maxillofac Surg. 2012; 70:320.
Crowley, T, Kaugras, GE, Gunsolley, JC. Odontogenic keratocysts: a clinical and histologic comparison of the parakeratin and orthokeratin variants. J Oral Maxillofac Surg. 1992; 50:22–26.
Evans, DG, Ladusans, EJ, Rimmer, S, et al. Complications of the naevoid basal cell carcinoma syndrome: results of a population based study. J Med Genet. 1993; 30:460–464.
Kolokythas, A. OKC: to decompress or not to decompress—a comparative study between decompression and enucleation vs resection/peripheral ostectomy. J Oral Maxillofac Surg. 2007; 65(4):640–644.
Madras, J. Keratocystic odontogenic tumor: reclassification of the odontogenic keratocyst from cyst to tumor. J Can Dent Assoc. 2008; 74:2.
Marx, RE, Stern, D. Oral and maxillofacial pathology: a rationale for diagnosis and treatment. Chicago: Quintessence; 2003.
Pindborg, JJ, Hansen, J. Studies on odontogenic cyst epithelium: clinical and roentgenographic aspects of odontogenic keratocysts. Acta Pathol Microbial Scand. 1963; 58:283.
Pogrel, MA. Keratocystic odontogenic tumor. In: Bagheri S, ed. Current therapy in oral and maxillofacial surgery. St Louis: Mosby, 2012.
Pogrel, MA, Jordan, RC. Marsupialization as a definitive treatment for the odontogenic keratocyst. J Oral Maxillofac Surg. 2004; 62:651–655.
Pogrel, MA, Schmidt, BL. The odontogenic keratocyst. Oral Maxillofacial Surg Clin N Am. 15(3): xi, 2003.
Shear, M. Primordial cysts. J Dent Assoc S Afr. 1960; 152:1.
Tolstunov, L, Treasure, T. Surgical treatment algorithm for odontogenic keratocyst: combined treatment of odontogenic keratocyst and mandibular defect with marsupialization, enucleation, iliac crest bone graft and dental implants. J Oral Maxillofac Surg. 2008; 66:1025.
Quereshy, F, Barnum, G, Demko, C, et al. Applications of cone beam computed tomography in the practice of oral and maxillofacial surgery. J Oral Maxillofac Surg. 2008; 66:791.
Unilocular Radiolucent Lesion of the Mandible
Imaging
In this patient, a panoramic radiograph (Figure 1-3, A) demonstrates a well-corticated unilocular radiolucent lesion of the right posterior mandible extending from the area of tooth #31 up to the sigmoid notch and coronoid process. The right mandibular third molar (tooth #32) is displaced inferiorly, and the lesion involves the roots of tooth #31, with some resorption and superior displacement of the tooth. After aspiration and incisional biopsy, teeth #31 and teeth #32 were extracted and the cyst was enucleated and curettaged (Figure 1-3, B to E). Six- and 16-week postoperative orthopantograms demonstrate good progressive bony fill of the defect (Figure 1-3, F and G).
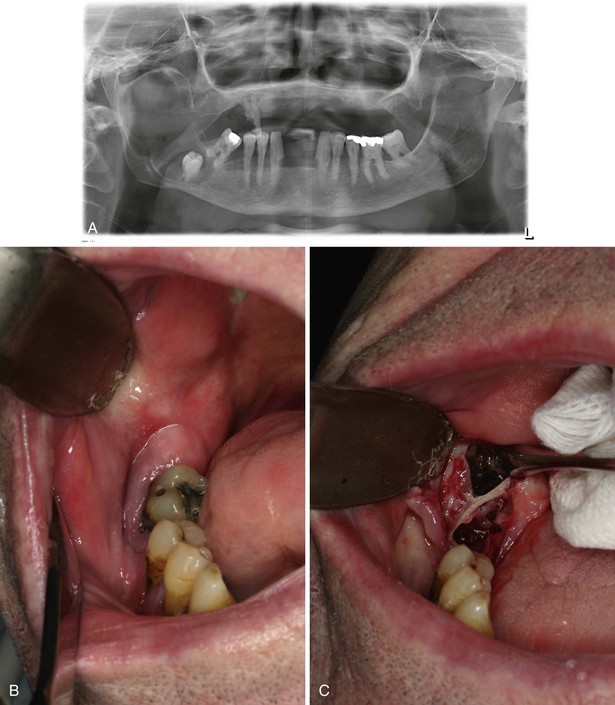
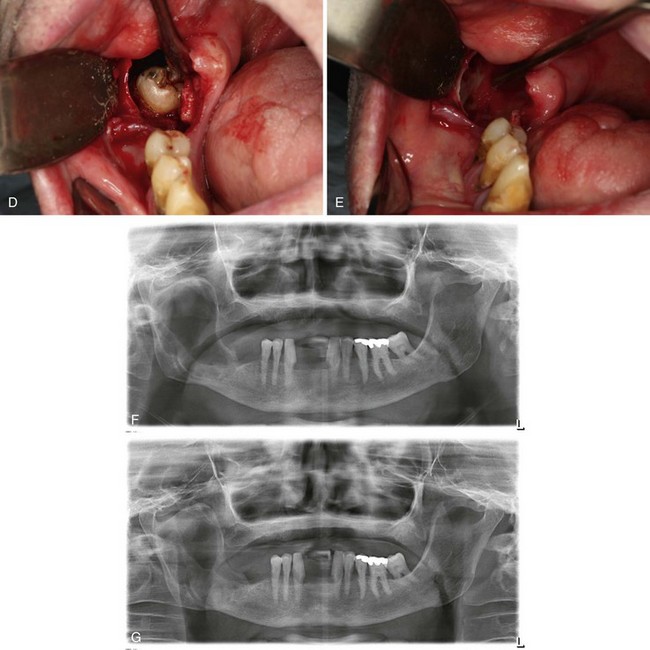
Figure 1-3 A, Unilocular radiolucency from posterior mandibular body to sigmoid notch. B, Preoperative photograph demonstrating absence of tooth #32. C, Initial exposure of the lesion. D, Unroofing of the lesion and exposure of tooth #32. E, Surgical defect after enucleation and curettage of the lesion. F, Orthopantogram 6 weeks after enucleation and curettage of the lesion. G, Orthopantogram 16 weeks after enucleation and curettage of the lesion.
Differential Diagnosis
The differential diagnosis can be divided into lesions of cystic pathogenesis, neoplastic (benign or malignant) lesions, and vascular anomalies (least common). Well-defined borders and the lack of a multilocular appearance are more suggestive of a cystic process, but this distinction is not predictable. The differentials presented in Box 1-3 should be considered; the first three are the most likely.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses