Chapter 1
Introduction to Implant Dentistry
INTRODUCTION
The successful long-term clinical use of dental endosseous implants requires some type of biologic attachment of implants to bone. In 1969, Brånemark et al. defined this process as osseointegration (Branemark et al. 1977). This process has been subsequently studied by numerous researchers around the world and has come to identify the functional stability of the endosseous implant/bone connection (Davies 1998). The histology and biomechanics of osseointegration are beyond the scope of this text; the reader is referred to other sources for further information and increased understanding relative to osseointegration.
Treatment of edentulous or partially edentulous patients with endosseous implants requires a multidisciplinary team approach. This team generally consists of an implant surgeon, a restorative dentist, and a dental laboratory technician. Implant dentistry is a restorative-driven service, and the ultimate success of implant treatment will be measured, at least in part, by the aesthetic and functional results as perceived by patients. Prosthesis design, whether a single implant-retained crown or full-arch prosthesis, will have a major impact on the number, size, and position of the implant(s) that will be used in a particular treatment plan. Treatment planning for implant dentistry must therefore begin with the restorative phase prior to considering the surgical phases of treatment.
Brånemark and coworkers introduced a two-stage surgical protocol into North America in 1982 (Zarb 1993). Numerous, long-term clinical studies have proven the efficacy of titanium endosseous implants (Adell 1981; Friberg et al. 1991; Sullivan et al. 2002; Testori et al. 2002; Ostman et al. 2012). Most clinicians consider osseointegration of dental implants to be predictable and highly effective in solving clinical problems associated with missing teeth (Davarpanah et al. 2002).
PURPOSE OF TEXTBOOK
The purpose of this textbook is to provide clinicians and dental laboratory technicians with a step-by-step approach to the treatment of certain types of edentulous and partially edentulous patients with dental implants. Eight types of patient treatments will be featured. The treatments will be illustrated with emphasis on diagnosis and treatment planning, restorative dentist/implant surgeon communication, and restorative treatments, on an appointment-by-appointment basis. The requisite implant components (restorative and laboratory) will be identified for each specific appointment. Laboratory procedures and work orders will also be included. Implant loading protocols will be discussed for each particular case presentation.
The biologic and theoretical aspects of osseointegration will not be reviewed. Osseointegration will be defined as clinically immobile implants, absence of peri-implant radiolucencies as assessed by an undistorted radiograph, mean vertical bone loss less than 0.2 mm annually after the first year of occlusal function, and absence of pain, discomfort, and infection (Smith & Zarb 1989). Clinical verification of osseointegration can sometimes be difficult. Some implants that have been considered successful at the second surgical or impression appointments have subsequently failed prior to or after completion of the prosthetic portion of treatment. Zarb and Schmitt (1990) reported that late failures occurred 3.3% of the time in patients with mostly edentulous mandibles. Naert et al. (1992) published a report that contained data from partially edentulous patients’ maxillae and mandibles. They reported that late failures occurred in 2.5% of the cases studied. Late failures are important to clinicians and patients because of the additional expenses and treatments that patients may elect to undergo in replacing prostheses on failed implants.
This text will concentrate on how clinicians may successfully incorporate implant restorative dentistry into their practices. A team approach will be emphasized among members of the implant team: restorative dentists, implant surgeons, dental laboratory technicians, dental assistants, office staff, and treatment coordinators. Appointment sequencing, laboratory work orders, and fee determination for restorative dentists will also be discussed including the identification of costs associated with fixed overhead, implant components, laboratory services, and profit margins.
Clinicians have multiple implant systems to choose from. There are similarities and differences among systems including but not limited to macroscopic surface morphology, implant/abutment connections, diameters, thread pitch, and screw hex/morphology. The author and coauthors purchased all of the components that were used in this textbook. The principles described in this textbook should be applicable to multiple implant manufacturers.
Economics of Implant Dentistry
One of the major reasons cited by general dentists relative to including or excluding implant dentistry in their practices is the costs involved in dental implant treatment. Levin reported that more than 35% of patients referred from general dentists to oral surgeons or periodontists for implant dentistry never actually make the appointment (Levin 2004). He has recommended that financing should be offered to every implant patient because it is not known which patients will require financing for treatment and which ones will not. Levin considered that financing was no longer an option; it should be considered a necessity. He reported that clients of the Levin Group significantly increased their levels of case acceptance by making financing options available to patients.
Levin (2005) described a comprehensive approach to dentistry that included four significant parts:
Levin identified implant dentistry for his general practitioner clients as an enormous growth opportunity and also stated that more than half of general dentists do not restore a single implant in any given year. Implant dentistry not only improves the lives of patients, it also can be a significant profit center for dental practices. Since implant dentistry generally is not covered by dental insurance, Levin stated that implants should be viewed as an opportunity to increase the elective portions of dental practices.
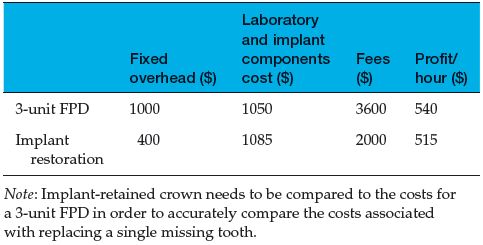
Implant treatment may be divided into treatment of partially edentulous and edentulous patients. Partially edentulous patients may warrant treatment involving the replacement of one tooth, or they may require replacement of multiple teeth. Periodontal disease may also factor into dental implant treatment planning. It has been the author’s personal experience that patients will frequently call for comparison shopping. A common question is, “How much will implants cost?” Patients may also request the costs of a single crown for comparison purposes. It is the responsibility of the dental staff to make sure patients know that in order to make fair comparisons, patients must compare the costs associated with a 3-unit fixed partial denture (FPD) or similar prosthesis to the costs of an implant-retained restoration replacing one tooth. This may sometimes be difficult to explain/inquire of patients during the initial phone conversation (Tables 1.1–1.3).
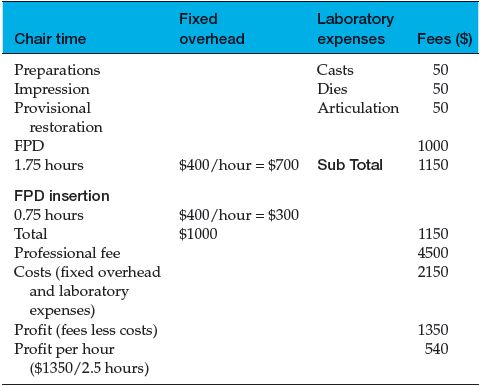
Table 1.1 Costs/fees/profits associated with a 3-unit porcelain-fused-to-metal (PFM) FPD.
Implant dentistry should also be profitable for clinicians and dental laboratory technicians. Initially, as with other new technologies that require the acquisition of learned, skilled behaviors, implant restorative dentistry may not be as profitable as other aspects of restorative dentistry. Restorative dentists should expect a learning curve relative to diagnosing, treatment planning, and treatment in implant restorative dentistry. With practice and reasonable efforts on behalf of the dentist and staff, implant dentistry may become one of the most profitable aspects of general practice.
Predictability of Fixed Prosthodontics
There are numerous goals of prosthodontic treatment, among them are to provide aesthetic and functional replacements for missing teeth on a long-term basis. Clinicians would like to attain these goals with restorations that have a predictable prognosis, minimal biologic trauma, and reasonable cost. For a significant number of restorative dentists, there are multiple advantages associated with conventional fixed prosthodontic therapy: familiarity with protocols, techniques, and materials. There are also multiple limitations associated with conventional fixed prosthodontics: tooth preparation and soft tissue retraction, potential pulpal involvement, recurrent caries, and periodontal disease. Missing teeth have been predictably replaced with FPDs for many years. However, there are increased stresses and demands placed on the abutment teeth, as well as limitations associated with ectopic tooth positions.
Table 1.2 Costs/fees/profits associated with an implant-retained crown (premachined abutment/PFM crown).
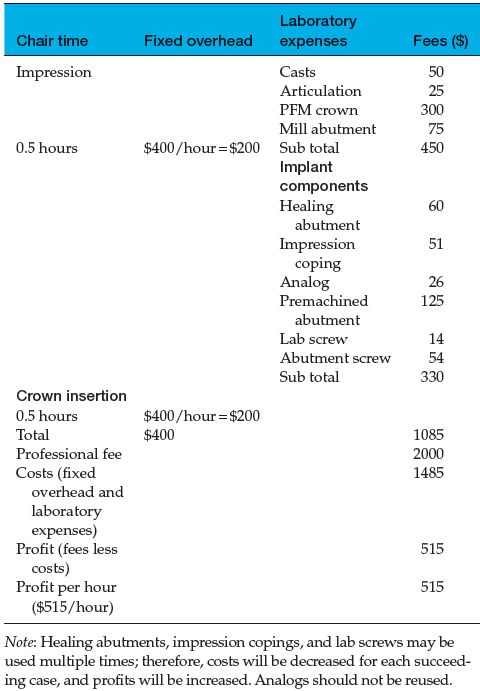
Table 1.3 Comparisons of costs, fees, and profits per hour for 3-unit FPD versus single-unit implant-retained crown.
In 1990, more than four million FPDs were placed in the United States (ADA Survey 1994). It may be surprising to note that there is little long-term research on the longevity of these restorations; comparisons between studies cannot be easily accomplished due to the lack of established parameters (Mazurat 1992). The authors have reported on the failure rates of FPDs over time, but the definitions of failures have been inconsistent: recurrent caries, fractured porcelain, broken rigid connectors, and loss of periodontal attachment (Schwartz et al. 1970; Reuter & Brose 1984; Randow et al. 1986; Walton et al. 1986; Foster 1990).
FPDs have documented long-term success. Scurria et al. (1998) performed a meta-analysis of multiple published studies and documented success rates as high as 92% at 10 years and 75% at 15 years. Other authors have recorded failure rates of 30% or more for FPDs at 15–20 years (Lindquist & Karlsson 1998). Cenci et al. (2010) reported the results of a clinical study with 8 years of follow-up that posterior fiber-reinforced FPDs exhibited acceptable clinical performances after a period of up to 8 years. The cumulative survival rate (CSR) was 81.8%. A key point that should be recognized from these reports is that it is important for clinicians to realize that for younger patients, FPDs may need to be replaced two to three times during their lifetimes.
Ioannidis et al. (2010) investigated the possible influence patients’ ages may have on the longevity of tooth supported fixed prosthetic restorations. Assessment and selection of studies were conducted in a two-phase procedure by two independent reviewers utilizing specific inclusion and exclusion criteria. The minimum mean follow-up time was set at 5 years. The results of the review demonstrated that increased age of patients should not be considered as a risk factor relative to the survival of fixed prostheses. Although the majority of studies showed no effect of age on survival of fixed prostheses, the authors concluded that there was some evidence that middle-aged patients may present with higher failure rates.
Miyamoto et al. (2007) reported the results of a long-term clinical study where data were collected from 3071 restored teeth from 1448 compliant patients from a single private practice in Yamagata, Japan. Follow-up times ranged from 15 to 23 years, with a mean follow-up of 19.2 years. Every tooth and restoration placed during this time frame was evaluated by one of the authors at each recare visit. Miyamoto and others reported that during this clinical study, multisurface restorations had the highest incidence of failures (P < 0.001) Abutment teeth for removable partial dentures (RPDs) had the highest individual failure rates that resulted in extractions. They concluded that restored teeth experienced a higher incidence of failure compared with unrestored teeth. Full crowns and abutments for fixed partial dental prostheses had fewer restorative failures when compared with teeth with complex multisurface restorations. RPD abutments experienced the highest failure rate.
In a literature review, Priest (1996) reviewed multiple papers to compare the efficacy of implant-retained crowns and conventional FPDs over time. He found that although FPDs were assumed to demonstrate predictable longevity, failure rates have been reported from 3% failure rates over 23 years to 20% failure rates over 3 years. Implant longevity, on the other hand, appears to be more promising and generally displays narrower ranges of failures: 9% over 3 years to 0% over 6.6 years. Priest cautioned that failure rates for FPDs and implant-retained crowns cannot be easily compared among studies since parameters had not been established and that replacing missing teeth is a complex issue. There are sufficient data for single-tooth implant-retained restorations to be used as functional and biologic methods for long-term tooth replacement.
DEVELOPMENT OF PROGNOSIS FOR TEETH: EXTRACT OR MAINTAIN
A question often asked by clinicians and patients relates to the viability and prognosis of maintaining compromised teeth. Even with the advances in implant dentistry since the 1970s, the predictability of implants is still not 100%. Therefore, it may still be difficult to recommend the extraction of a tooth with a compromised prognosis and replace it with a dental implant. The American Academy of Periodontology’s position paper on dental implants stated that all patients should be informed as to the risks and benefits of implant and alternative treatment prior to implant placement and restoration (American Academy of Periodontology 2000).
O’Neal and Butler (2002) discussed the clinical and economic factors that clinicians should consider in making decisions relative to extraction and implant placement versus retention of compromised teeth (O’Neal & Butler 2002). They divided the clinical issues into four basic categories:
The Heavily Restored Tooth
This type of tooth may have been damaged as a result of blunt trauma, dental caries, or multiple dental restorations (Figure 1.1). In Figure 1.1, this mandibular molar had been treated endodontically and had moderate horizontal bone loss and recurrent dental caries. The author considered the long-term prognosis for this tooth to be poor if used as the distal abutment for a new 3-unit FPD. The treatment choices for this patient included hemisection and mesial root amputation, osseous surgery, and a new 3-unit FPD. Or, the tooth could be extracted, the socket grafted with bone or a bone substitute, and the extraction site allowed to heal prior to placing an implant and implant restoration (Figure 1.2). Based on the reports of Miyamoto and Priest, the prognosis for the latter choice is much better and may be more conservative long term than the first treatment option.
Figure 1.1 Radiograph of mandibular molar that may be considered for use as the distal abutment for a 3-unit FPD. It had been treated endodontically and restored with a crown. There are recurrent caries beneath the mesial margin.
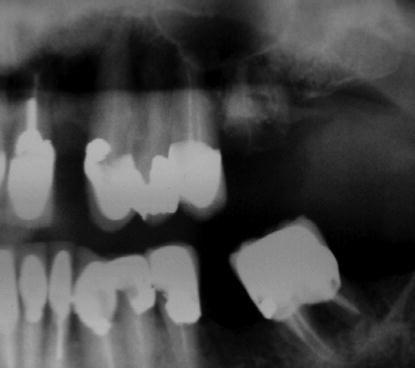
Figure 1.2 Clinical view of implant-retained crowns that replaced the mandibular right second premolar and first molar.

Figure 1.3 Radiograph of a maxillary lateral incisor with previous endodontic therapy. There was an incomplete horizontal root fracture; the post retained the crown.

The clinical condition exemplified by Figure 1.3 is also frequently encountered in clinical practice: an incompletely fractured tooth with previous endodontic therapy where the crown was held in place by a post. Numerous authors have suggested that the axial walls of tooth preparations for endodontically treated teeth should include at least 1 mm of dentin in order to provide the requisite ferrule effect needed for predictable retention for the crown (Sorenson & Engelman 1990; Fan et al. 1995; Libman & Nicholls 1995). Crown lengthening procedures can be accomplished in order to obtain greater access to dentin for increased retention of the crown, but the surgery is associated with moderate to significant surgical morbidity and accomplished at the expense of the supporting bone.
The Furcation-Involved Tooth
Posterior teeth with advanced bone loss are the most commonly lost teeth. Hirschfeld studied natural teeth over a 22-year period and found that 31.4% of molars and 4.9% of single-rooted teeth were lost (Hirschfeld & Wasserman 1978). Therefore, decisions to retain or extract posterior teeth generally involve multirooted molars. Both maxillary and mandibular molar teeth exhibit concavities associated with multiple roots. The anatomy may also be compromised with recurrent caries and lateral canals. In Figure 1.4, the mandibular right first molar had previous endodontic therapy, advanced bone loss around both roots and in the furcation, and mobility and was uncomfortable for the patient. The patient’s chief complaint was related to the discomfort that she was feeling anytime she attempted to chew on the right side. Yet she did not want to have this tooth extracted. Even with a root resection, this tooth had a poor prognosis as an abutment for an FPD. A more appropriate choice would be extraction, grafting, and placement of one implant to replace the missing molar.
Figure 1.4 Radiograph of mandibular right posterior segment that demonstrates advanced bone loss around the first molar. This tooth was a poor candidate for root resection and future use as an abutment for a 3-unit FPD.

Figure 1.5 Radiograph after endodontic therapy for the mandibular right first and second molars prior to resection of the second molar’s mesial root.

The most common causes of failure in posterior, furcation-involved teeth have been reported to be recurrent caries and endodontic failure (Buhler 1994). When clinical success is likely, root resection procedures can be clinically acceptable with a reasonable long-term prognosis. In Figures 1.5–1.7, compromised mandibular molars were treated with endodontic therapy, posts, root resections, and a fixed periodon/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


