Information Gathering and Diagnosis Development
Accurate diagnostic information forms the foundation of any treatment plan. This information comes from several sources: the patient history, radiographs, and the clinical examination. The dentist must critically analyze the information before recommending treatment options to the patient. The goal of this chapter is to discuss both the types of data that the dentist in general practice typically collects and the ways in which the dentist evaluates and documents this information in preparation for creating a treatment plan.
OVERVIEW OF THE DIAGNOSTIC PROCESS
The diagnostic process is begun by gathering information about the patient and creating a patient database from which all future decisions will be made. Although the components of each patient’s database vary, each includes pieces of information, or findings, that come from asking questions, reviewing information on forms, observing and examining structures, performing diagnostic tests, and consulting with physicians and other dentists.
Findings fall into several categories. Signs are findings discovered by the dentist during an examination. For instance, the practitioner may observe that a patient has swollen ankles and difficulty in breathing when reclined, signs suggestive of congestive heart failure. Findings revealed by the patients themselves, usually because they are causing problems, are referred to as symptoms. Patients may report such common symptoms as pain, swelling, broken teeth, loose teeth, bleeding gums, and esthetic concerns. When a symptom becomes the motivating factor for a patient to seek dental treatment, it is referred to as the chief complaint or chief concern. Patients who are new to a practice often have one or more chief complaints (Figure 1-1).

Figure 1-1 This patient reported symptoms of tooth pain and bleeding gums. Many signs dark teeth, receding gingival tissue, and poor oral hygiene suggest serious dental problems.
The clinician must evaluate findings individually and in conjunction with other findings to determine whether or not the finding is significant. For example, the finding that a patient is being treated for hypertension may be not be significant alone, but when accompanied by another finding of blood pressure measuring 180/110 mm Hg, the level of importance of the first finding increases. Questions arise as to whether the patient’s hypertension is being managed appropriately or whether the patient is even taking the prescribed medication regularly. Obviously, further questioning of the patient is in order, generating even more findings to evaluate for significance. The process of differentiating significant from insignificant findings can be challenging for dental students and recent graduates. For example, a student may believe a dark spot on the occlusal surface of a tooth to be significant, while a faculty member might discard the finding as simply stained fissure, not requiring treatment. Thankfully, this differentiation and selection process becomes easier as the dentist gains experience from treating more and more patients.
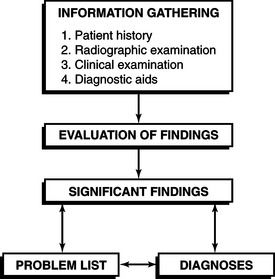
The process of discovering significant findings leads to a list of diagnoses or patient problems that ultimately forms the basis for creating a treatment plan (Figure 1-2). Experienced practitioners may not always evaluate patients in a linear, sequential fashion. Instead, they move back and forth between discovering findings, evaluating for significance, and making a diagnosis, and they may begin to think about treatment options before gathering all the data. Despite this normal process, the novice practitioner (and even the experienced one) is highly advised against giving treatment recommendations to patients before creating and analyzing the entire patient database. Typically, the patient initiates the discussion during the examination process. For example, examination of a sensitive tooth may elicit a query from the patient as to whether it can be saved and at what cost. Saying “yes” and “in two appointments” may prove embarrassing when subsequent radiographs reveal extensive decay and the need to extract the tooth. To prevent such errors, the inquisitive patient should be gently reminded that the examination is not yet complete and that more information will enable questions to be answered more completely.
INFORMATION GATHERING
Gathering information about the patient often requires more time and attention than any other aspect of treatment planning. To prevent missing important findings, the dentist should gather data in an organized, systematic manner. Each practitioner must develop a consistent and standardized mechanism for gathering historical information about the patient, obtaining radiographs, and performing the clinical examination. It is essential that any data gathered be both complete and accurate. If deficiencies occur in either completeness or accuracy, the validity of the final treatment may be suspect.
The sheer number of findings that arise when evaluating a patient with a complicated health history or many dental problems can overwhelm the beginning practitioner. Staying focused on each stage of information gathering and being careful to record information in an organized fashion for later analysis help prevent confusion. This section covers the four major categories of information required to begin developing a treatment plan: the patient history, clinical examination, radiographic examination, and other diagnostic aids.
Patient History
The distinguished Canadian physician Sir William Ostler wrote, “Never treat a stranger.” His words underscore the need for a thorough patient history; experienced dentists learn everything they can about their patients before beginning treatment. Obtaining a complete and accurate patient history is part of the art of being a doctor. It takes considerable practice and self-study to become a talented investigator. No set amount of historical information is required for each patient. The volume of information collected and the complexity of the data collection process naturally depend on the severity of the patient’s problems. As more information comes to light, additional diagnostic techniques may need to be employed.
In dental offices, persons other than the dentist have access to patient information. The entire office staff should be aware of the confidential nature of patient information and cautioned about discussing any patient’s general or oral health history other than for treatment purposes. The author is reminded of one example of a lapse in confidentiality. When updating the health history, a staff member learned that a patient had recently become pregnant. Later in the day, the patient’s mother was in the office, and another staff member congratulated her on her daughter’s pregnancy. At first the mother was elated, but later was hurt that her daughter had not told her herself. The incident provided an uncomfortable reminder of the importance of keeping patient information confidential both inside and outside the office.
In the United States, the Health Insurance Portability and Accountability Act of 1996, HIPAA, requires practitioners and health care organizations to prevent unnecessary use and release of protected health information (PHI). Patient PHI includes medical findings, diagnoses and treatment notes, and any demographic data that could identify the patient, such as an address, phone number, or personal identification number. HIPAA permits the use of a patient’s PHI for treatment purposes, obtaining payment for services, and other organizational requirements, such as quality assurance activities or assisting legal authorities. Patients must be given, and sign, an acknowledgment that they have received information about how the practitioner or organization will use the PHI and who they can contact if they believe their health information has been inappropriately used or released. Under HIPAA, a patient also has the right to inspect his or her medical records.
Techniques for Obtaining a Patient History
The two primary methods for obtaining the patient history are (1) questionnaires and forms and (2) patient interviews. A secondary method involves requesting information from another health care practitioner.
Questionnaires and Forms
The use of questionnaires and forms during the examination process offers several advantages. Questionnaires save time, do not require any special skills to administer, and provide a standardized method for obtaining information from a variety of patients. Many types of forms are avail-able commercially, or the practitioner can create his or her own.
Unfortunately, using a form to gather information has several disadvantages. The dentist only gets answers to the questions asked on the form, and important findings can be missed. The severity of a condition may not be reflected in a simple positive response. Patients may misinterpret questions, resulting in incorrect answers. It may be necessary to have the forms printed in other languages to facilitate information gathering. The more comprehensive the questionnaire is, the longer it must be, which can be frustrating to patients. Finally, patients can more easily falsify information on a questionnaire or form than when confronted directly in an interview.
Patient Interviews
A major advantage of interviewing patients is that the practitioner can tailor questions to the individual patient. The patient interview serves a problem-solving function and functions quite differently from a personal conversation. There is a level of formality to the discussion, which centers on the patient’s health and oral care needs, problems, and desires. To obtain accurate information and not influence the responses, the dentist must be a systematic and unbiased information gatherer. Being a good listener is key to facilitating information flow from the patient. The desired outcome of the interviewing process is to develop a good rapport with the patient by establishing a cooperative and harmonious interaction. If the interviewer does not speak the patient’s language, it may be necessary to have a translator available. A sign language translator may be also required if the patient is hearing impaired.
The dentist can ask two general types of questions when interviewing: open and closed. Open questions cannot be answered with a simple response, such as “yes” or “no.” Instead, open questions get the patient involved and generate reflection by asking for opinions, past experiences, feelings, or desires. Open questions usually begin with “what” or “how” and should avoid leading the patient to a specific answer.
What do you think is your biggest dental problem?
Tell me about your past dental care.
Tell me more about your heart problems.
Closed questions, on the other hand, are usually simple to answer with one or two words. They permit specific facts to be obtained or clarified but do not give insight into patient beliefs, attitudes, or feelings.
Which tooth is sensitive to cold?
How long has it been since your teeth were last examined?
In general, the examiner should use open questions when beginning to inquire about a problem. Later, closed questions can be asked to obtain answers to specific questions. The skilled clinician knows when to use each type of question during the interview. Examples are presented in the following sections. The In Clinical Practice box features tips on how to be an effective interviewer.
COMPONENTS OF A PATIENT HISTORY
Demographic Data
Demographic data include basic information, such as the patient’s name, address, phone number, physician’s name and phone, third party (insurance) information, social security number, and so on. Demographic data, like any other historical information, must be accurate, complete, and current. Errors in recording insurance information, such as an incorrect policy number or failure to clarify who is responsible for payment, can be costly to a dental practice.
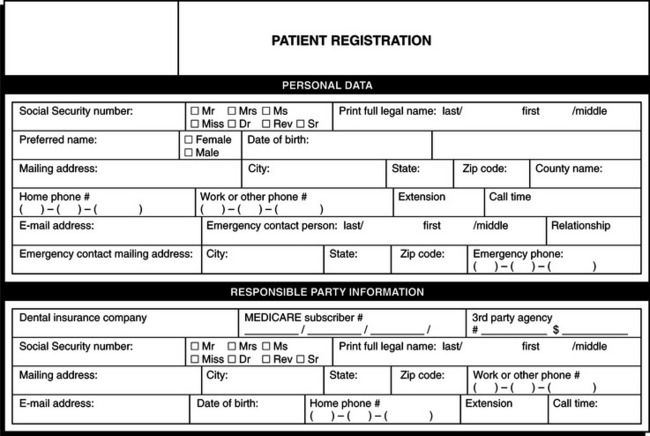
Useful additional information includes work, cell, and evening telephone numbers, and seasonal and electronic mail addresses. The patient reports most of this information on demographic questionnaires and forms at the first visit (Figure 1-3). The office staff may also interview the patient if additional information is required or if information requires updating. Although commercial forms can be used to record and organize demographic information, many practices have designed their own. Some dental practices that use an electronic health record (EHR) instead of a paper record may scan paper forms or have the patient enter information into a computer or hand held device that is linked directly to the clinic information system.
Chief Complaint and History
The chief complaint or chief concern is the primary reason, or reasons, that the patient has first presented for treatment. For most patients, the chief complaint is usually a symptom or a request. Any complaints are best obtained by asking the patient an open-ended question such as, “What brought you to see me today?” or “Is there anything you’re hoping I can do for you?” This is more effective than limiting the patient’s response by asking a closed question such as, “Is anything bothering you right now?” or “Has it been a long time since you’ve seen a dentist?” Record chief complaints in quotes to signify that the patient’s own words are used. Careful attention to the chief complaint should alert the practitioner to important diagnoses and provide an appreciation for the patient’s perception of his or her problems, including level of knowledge about dentistry.
The history of present illness (HPI) is the history of the chief complaint, which the patient usually supplies with a little prompting. When possible, the dentist should keep the questioning open, although specific (closed) questions help clarify details.
HPI
The patient has had a dull ache in the lower right quadrant that has been increasing in intensity for the past 4 days. The pain is worse with hot stimuli and chewing and is not relieved by aspirin.
“I lost a filling and need my teeth checked.” (a symptom and a request)
HPI
The patient lost a restoration from an upper right molar 2 days ago. The tooth is asymptomatic. Her last dental examination and prophylaxis was 2 years ago.
Resolving the patient’s chief complaint as soon as possible represents a “golden rule” of treatment planning. When a new patient presents in pain, the dentist may need to suspend the comprehensive examination process and instead focus on the specific problem, make a diagnosis, and quite possibly begin treatment.
At times, the chief complaint may be very general, such as, “I need to chew better,” or “I don’t like the appearance of my teeth.” In such instances, the practitioner must carefully dissect what issues concern the patient. Often, what initially appears to be the problem may be a more complex issue that will be difficult to manage until later in the treatment plan. During the course of treatment, the dentist should advise the patient as to what progress is being made toward resolving the initial chief complaint.
General Health History
The dentist must obtain a health history from each patient and regularly update this information in the record. A comprehensive health history contains a review of all of the patient’s past and present illnesses. Information about a patient’s health history can prevent or help manage an emergency. Some systemic diseases may affect the oral cavity and the patient’s response to dental treatment, including delaying healing or increasing the chance for infection. Conversely, some oral diseases can affect the patient’s general health. Because many patients see their dentist more frequently than they see their physician, the dentist should use the patient’s general health history and physical examination to screen for significant systemic diseases, such as hypertension, diabetes, and cancer.
Most dental practices screen for potential health problems by asking all new patients to complete a health questionnaire (Figure 1-4, A and B). When reviewing the health questionnaire, the dentist must look for conditions that may affect treatment, patient management, or treatment outcomes. Interviewing the patient, first with open-ended questions about the problem and later with closed questions, usually clarifies positive responses to the questionnaire. Although it is beyond the scope of this book to present all the systemic conditions that can impact dental treatment, several are discussed in Chapter 5, including guidelines for consulting with the patient’s physician when the dentist has detected significant findings.
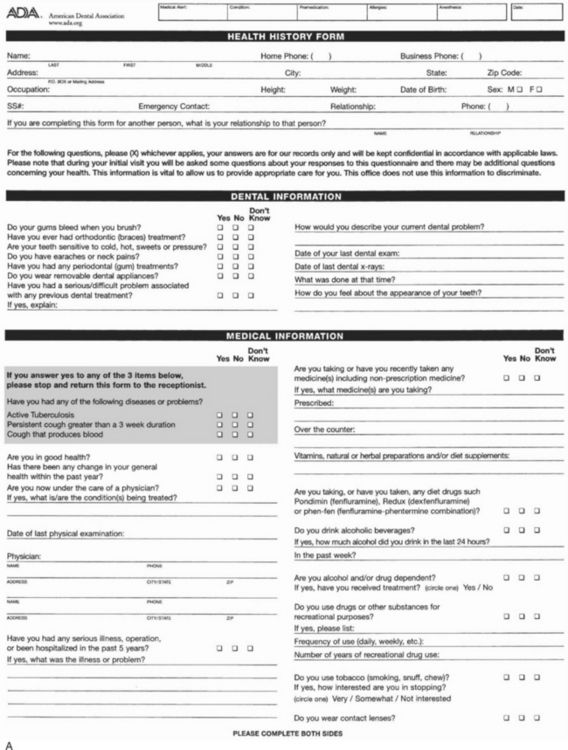
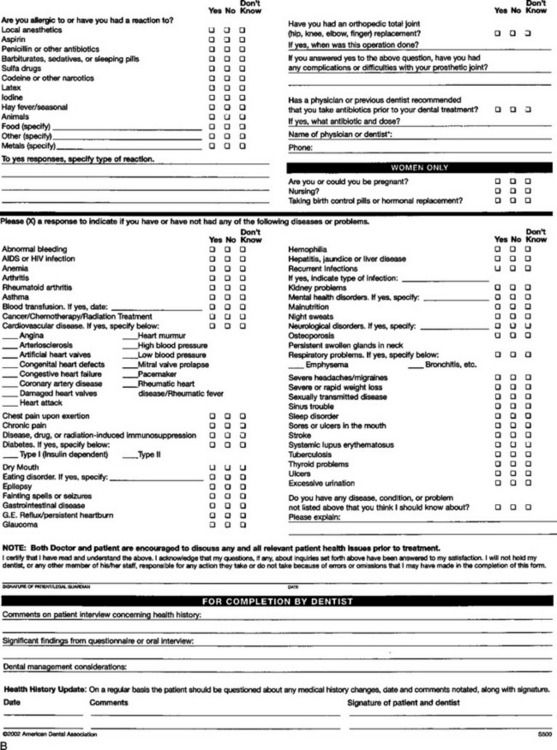
Figure 1-4 A Health history form, front side. B Health history form, back side. (Courtesy the American Dental Association, Chicago, Illinois.)
Whether using a preprinted questionnaire or an interview technique, the general health history should include a review of systems. Commonly reviewed systems include the cardiovascular, respiratory, central nervous, gastrointestinal, genitourinary, musculoskeletal, endocrine, and integumentary (including eyes and ears). The information gained through the review of systems enables the dentist (1) to recognize significant health problems that may affect dental treatment and (2) to elicit information suggestive of new health problems that were previously unrecognized, undiagnosed, or untreated.
Including both prescription and nonprescription medications in the medication history also provides valuable insight into the patient’s overall health. Any over-the-counter medications, herbal remedies, vitamins, or nutritional supplements used also should be included. The medication history can corroborate findings from the health history or may suggest new diseases or conditions that need further investigation. Some medications are, in themselves, cause for limiting, delaying, or modifying dental treatment. The dentist may consult one of several reference publications to help determine the indications and potential problems that may arise from the use of various drugs. Several references, available on electronic media or on the Internet, provide rapid access to information. Any potentially life threatening condition or medical problem that has a significant impact on the dental treatment should be displayed in a prominent place in the record.
Oral Health History
The oral health history incorporates such areas as the date of last dental examination, frequency of dental visits, types of treatment received, and the history of any problems that have emerged when receiving dental care. Common problems include syncope (fainting), general anxiety, and reactions to drugs used in dentistry. Patients should also be questioned about their oral hygiene practices. Experienced dentists spend whatever time is necessary to investigate the oral health history of the patient because of the strong influence it can have on future treatment.
While obtaining the oral health history, the dentist should first determine the general nature of the patient’s past care. Has the patient seen a dentist regularly or been treated only on an episodic basis? What kind of oral health care did the patient receive as a child? The frequency of oral health care can be an important predictor of how effectively the patient will comply with new treatment recommendations. If the patient has visited the dentist regularly, what types of treatment were provided? Was the patient satisfied with the treatment received? Did the dentist do anything in particular to make treatment more comfortable? It also is important to establish whether the patient has had any specialty treatment, such as orthodontic, endodontic, or periodontal care, in the event additional treatment is required in the future.
Investigation into the patient’s dental history supplements the clinical examination during which new findings may be identified. The dentist should establish the reason for any missing teeth, including when they were removed. Knowing the age of suspect restorations may yield important perspectives on the quality of previous work, the patient’s oral hygiene, how well previous treatment has held up, and the prognosis for new work. The age of tooth replacements may also have a bearing on whether the patient’s dental insurance will cover any necessary replacement.
Psychosocial History
The patient’s social, emotional, and behavioral history represents one of the most important and difficult areas to investigate. The patient’s occupation, habits, financial resources, and general lifestyle can significantly influence attitudes about dentistry. It is important to investigate the patient’s attitudes about the profession, including priorities, expectations, and motivations for seeking treatment. The psychosocial history is also a prime source of information about the patient’s financial status, time availability for treatment, mode of transportation to dental visits any or all of which may have a bearing on how dental treatment is planned or executed. Much of the psychosocial history will overlap with the oral health history, especially concerns regarding fear of dental treatment (covered in depth in Chapter 13) and concerns about the cost of treatment (discussed in Chapter 17).
The health questionnaire can be used to screen for information about habits such as smoking, alcohol, and drug use. Often, however, these questions are best pursued verbally during the patient interview. A patient’s behavior or medication profile may suggest the presence of some type of mental disease, a topic discussed further in Chapter 14.
CLINICAL EXAMINATION
Developing an accurate and comprehensive treatment plan depends on a thorough analysis of all the general and oral health conditions that exist when the patient presents for evaluation. A comprehensive clinical examination involves assembling significant findings from the following five areas:
Physical Examination
Unlike the physician who examines many areas of the body for signs of disease, the dentist in general practice usually performs only a limited overall physical examination that includes evaluation of:
With careful observation and findings from the health history, the dentist can detect many signs of systemic diseases that could have treatment implications and may suggest referral to a physician. For example, a patient who has difficulty walking may be afflicted with osteoarthritis or have a neurologic problem, such as Parkinson’s disease or a stroke. The appearance of the skin, hair, and eyes may suggest such diseases as anemia, hypothyroidism, or hepatitis.
Measuring vital signs provides an easy and objective measure for physical evaluation. Heart rate, rhythm, and blood pressure should be measured for every new patient and reevaluated at each periodic examination. The vital signs should also be taken before administering any local anesthetic or sedation and at the beginning of all visits for patients under treatment for high blood pressure, thyroid disease, or cardiac disease. Automated blood pressure devices have greatly simplified the process of obtaining these measurements. The normal pulse rate for adults is 60 to 90 beats per minute at rest, with a regular and strong rhythm. Blood pressure measurements can vary considerably between individuals, but ideally should be lower than 120/80 mm Hg. Information about how to evaluate a patient’s blood pressure can be found in Chapter 5.
Although not regularly recorded, measuring vital signs such as respiration rate and temperature may be indicated for patients with respiratory problems or signs of infection. Some practitioners record height and weight measurements for children, with the latter being especially useful for calculating medication dosages.
Intraoral and Extraoral Examination
Evaluation of head and neck structures for evidence of tissue abnormalities or lesions constitutes an important part of a comprehensive examination. This is typically accomplished by looking for variations from normal and by palpating the tissues to detect abnormalities. The following extraoral structures of the head and neck sh/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses