1 HISTORY TAKING AND CLINICAL EXAMINATION
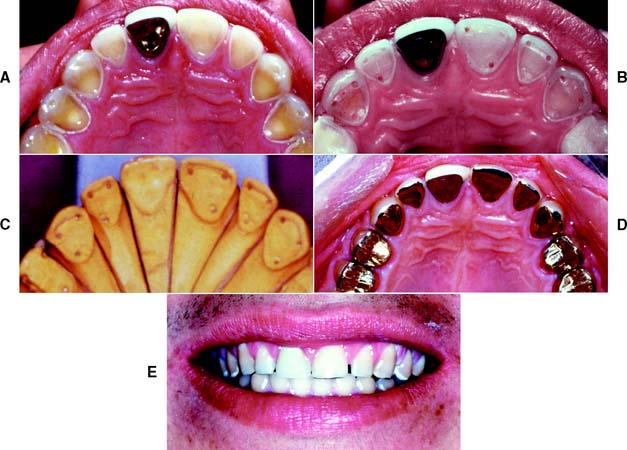
Fixed prosthodontic treatment involves the replacement and restoration of teeth by artificial substitutes that are not readily removable from the mouth. Its focus is to restore function, esthetics, and comfort. Fixed prosthodontics can offer exceptional satisfaction for both patient and dentist. It can transform an unhealthy, unattractive dentition with poor function into a comfortable, healthy occlusion capable of years of further service and greatly enhance esthetics (Fig. 1-1A and B). Treatment can range from the fairly straightforward restoration of a single tooth with a cast crown (Fig. 1-1C) or replacement of one or more missing teeth with a fixed dental prosthesis (Fig. 1-1D) or implant-supported restoration to a highly complex restoration involving all the teeth in an entire arch or the entire dentition.
HISTORY
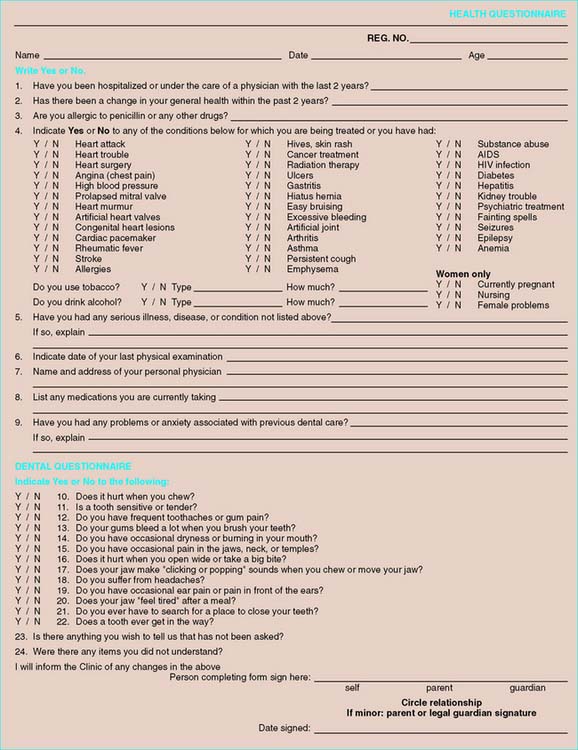
A patient’s history should include all pertinent information concerning the reasons for seeking treatment, along with any personal information, including relevant previous medical and dental experiences. The chief complaint should be recorded, preferably in the patient’s own words. A screening questionnaire (Fig. 1-2) is useful for history taking; it should be reviewed in the patient’s presence to correct any mistakes and to clarify inconclusive entries. If the patient is mentally impaired or a minor, the guardian or responsible parent must be present.
Chief Complaint
Chief complaints usually belong to one of the following four categories:
Comfort
If pain is present, its location, character, severity, and frequency should be noted, as well as the first time it occurred, what factors precipitate it (e.g., hot, cold, or sweet things), and any changes in its character. Is it localized or more diffuse in nature? It is often helpful to have the patient point at the area while the dentist pays close attention.
Appearance
Compromised appearance is a strong motivating factor for patients to seek advice as to whether improvement is possible (Fig. 1-3). Such patients may have missing or crowded teeth, or a tooth or restoration may be fractured. Their teeth may be unattractively shaped, malpositioned, or discolored, or there may be a developmental defect.
Medical History

Fig. 1-4 Severe gingival hyperplasia associated with anticonvulsant drug use.
(Courtesy of Dr. P. B. Robinson.)
Dental offices practice “universal precautions” to ensure appropriate infection control. This means that full infection control is practiced for every patient; no additional measures are needed when dentists treat known disease carriers.6
Dental History
Endodontic history
Patients often forget which teeth have been endodontically treated. These can be readily identified with radiographs. The findings should be reviewed periodically so that periapical health can be monitored and any recurring lesions promptly detected (Fig. 1-6).
Orthodontic history
Occlusal analysis should be an integral part of the assessment of a postorthodontic dentition. If restorative treatment needs are anticipated, they should be undertaken by the restorative dentist. Occlusal adjustment (reshaping of the occlusal surfaces of the teeth) may be needed to promote long-term positional stability of the teeth and reduce or eliminate parafunctional activity. On occasion, root resorption (detected on radiographs) (Fig. 1-7) may be attributable to previous orthodontic treatment. As the crown/root ratio is affected, future prosthodontic treatment and its prognosis may also be affected. Restorative treatment can often be simplified by minor tooth movement. When a patient is contemplating orthodontic treatment, considerable time can be saved if minor tooth movement (for restorative reasons) is incorporated from the start. Thus, good communication between the restorative dentist and the orthodontist may prove very helpful.
EXAMINATION
Thorough examination and data collection are needed for the prospective fixed prosthodontic patient, and the protocol for this effort can be obtained from various textbooks of oral diagnosis.7,8
General Examination
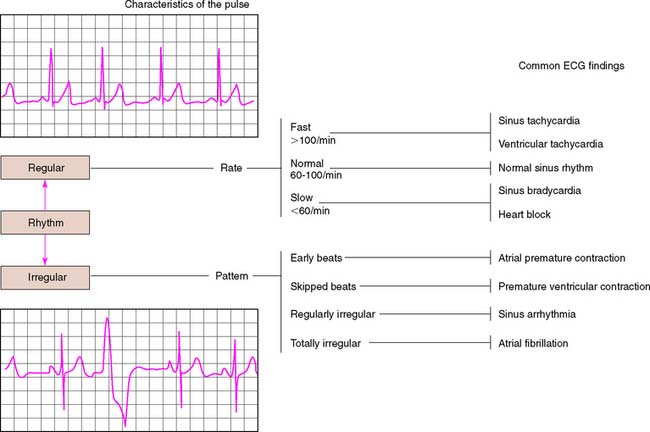
The patient’s general appearance, gait, and weight are assessed. Skin color is noted for signs of anemia or jaundice. Vital signs, such as respiration, pulse, temperature, and blood pressure, are measured and recorded. Fixed prosthodontic treatment is often indicated in middle-aged or older patients, who can be at higher risk for cardiovascular disease. Relatively inexpensive cardiac monitoring units are available for in-office use (Fig. 1-8). Patients with vital sign measurements outside normal ranges should be referred for a comprehensive medical evaluation before definitive treatment is initiated.
Extraoral Examination
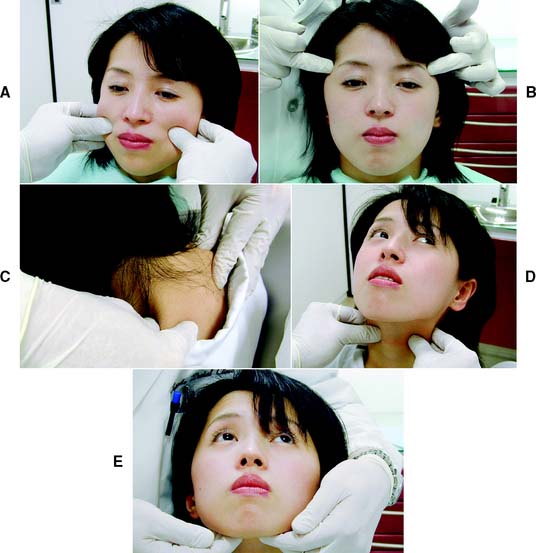
Temporomandibular joints
The clinician locates the TMJs by palpating bilaterally just anterior to the auricular tragi while the patient opens and closes the mouth. This permits a comparison between the relative timing of left and right condylar movements during the opening stroke. Asynchronous movement may indicate an anterior disk displacement that prevents one of the condyles from making a normal translatory movement (see Chapter 4). Auricular palpation (Fig. 1-9) with light anterior pressure helps identify potential disorders in the posterior attachment of the disk. Tenderness or pain on movement is noted and can be indicative of inflammatory changes in the retrodiscal tissues, which are highly vascular and innervated. Clicking in the TMJ is often noticeable through auricular palpation but may be difficult to detect in palpation directly over the lateral pole of the condylar process, because the overlying tissues can muffle the click. Placement of the fingertips on the angles of the mandible helps identify even a minimal click, because very little soft tissue lies between the fingertips and the mandibular bone.
A maximum mandibular opening resulting in less than 35 mm of interincisal movement is considered restricted, because the average opening is greater than 50 mm.9,10 Such restricted movement on opening can be indicative of intracapsular changes in the joints. Similarly, any midline deviation on opening and/or closing is recorded. The maximum lateral movements of the patient can be measured (normal is about 12 mm) (Fig. 1-10).
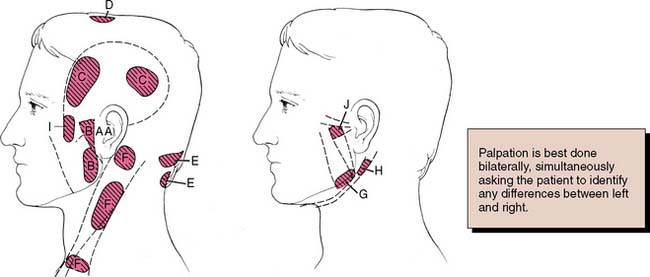
Muscles of mastication
Next, the masseter and temporal muscles, as well as other relevant postural muscles, are palpated for signs of tenderness (Fig. 1-11). Palpation is best accomplished bilaterally and simultaneously. This allows the patient to compare and report any differences between the left and right sides. Light pressure should be used (the amount of pressure one can tolerate when gently pushing on one’s closed eyelid without feeling discomfort is a good comparative measure), and if any difference is reported between the left and right sides, the patient is asked to classify the discomfort as mild, moderate, or severe. If there is evidence of significant asynchronous movement or TMJ dysfunction, a systematic sequence for comprehensive muscle palpation should be followed as described by Solberg9 and Krogh-Poulsen and Olsson.11 Each palpation site is given a numerical score based on the patient’s response. If neuromuscular or TMJ treatment is initiated, the examiner can then repalpate the same sites periodically to assess the response to treatment (Fig. 1-12).
Lips
The patient is observed for tooth visibility during normal and exaggerated smiling. This can be critical in fixed prosthodontic treatment planning,12 especially for margin placement of certain metal-ceramic crowns. Some patients show only their maxillary teeth during smiling. More than 25% do not show the gingival third of the maxillary central incisors during an exaggerated smile13 (Fig. 1-13). The extent of the smile depends on the length and mobility of the upper lip and the length of the alveolar process. When the patient laughs, the jaws open slightly and a dark space is often visible between the maxillary and mandibular teeth (Fig. 1-14). This has been called the negative space.14 Missing teeth, diastemas, and fractured or poorly restored teeth disrupt the harmony of the negative space and often require correction.15
Periodontal Examination
A periodontal examination16 should provide information regarding the status of bacterial accumulation, the response of the host tissues, and the degree of reversible and irreversible damage. Because long-term periodontal health is essential for successful fixed prosthodontics (see Chapter 5), existing periodontal disease must be corrected before any definitive prosthodontic treatment is undertaken.
Gingiva
Healthy gingiva (Fig. 1-15A) is pink, stippled, and firmly bound to the underlying connective tissue. The free margin of the gingiva is knife-edged, and sharply pointed papillae fill the interproximal spaces. Any deviation from these findings should be noted. With the development of chronic marginal gingivitis (Fig. 1-15B), the gingiva becomes enlarged and bulbous, loss of stippling occurs, the margins and papillae are blunted, and bleeding and exudate are observed.
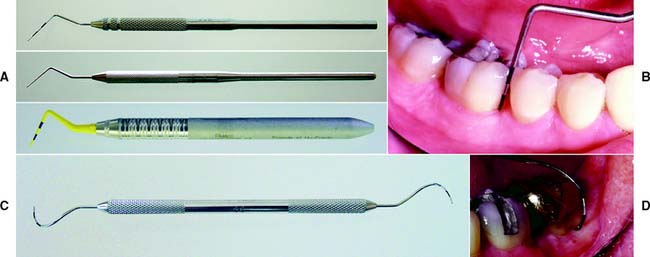
Periodontium
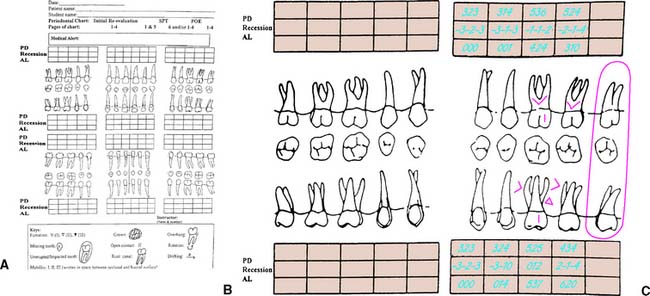
The periodontal probe (Fig. 1-16A) is one of the most reliable and useful diagnostic tools available for examining the periodontium. It provides a measurement (in millimeters) of the depth of periodontal pockets and healthy gingival sulci on all surfaces of each tooth. In this examination, the probe is inserted essentially parallel to the tooth and is “walked” circumferentially through the sulcus in firm but gentle steps; the examiner determines the measurement when the probe is in contact with the apical portion of the sulcus (Fig. 1-16B). Thus, any sudden change in the attachment level can be detected. The probe may also be angled slightly (5 to 10 degrees) in the interproximal areas to reveal the topography of an existing lesion. Probing depths (usually six per tooth) are recorded on a periodontal chart (Fig. 1-17), which also contains other data pertinent to the periodontal examination (e.g., tooth mobility or malposition, open or deficient contact areas, inconsistent marginal ridge heights, missing or impacted teeth, areas of inadequate attached keratinized gingiva, gingival recession, furcation involvements, and malpositioned frenum attachments).
Clinical Attachment Level
Documenting the level of attachment helps the clinician determine the amount of periodontal destruction that has occurred and is essential in rendering a diagnosis of periodontitis (loss of connective tissue attachment).17,18 This measurement also provides the clinician with more detailed and accurate information regarding the prognosis of an individual tooth. The clinical attachment level is determined by measuring the distance between the apical extent of the probing depth and a fixed reference point on the tooth, most commonly either the apical extent of a restoration and/or the cementoenamel junction (CEJ). This measurement can be documented on modified periodontal charts (Fig. 1-18) and incorporated with the standard periodontal documentation (see Fig. 1-17) to complete the clinical periodontal examination. When the free margin of the gingiva is located on the clinical crown and the level of the epithelial attachment is at the CEJ, there is no loss of attachment, and recession is noted as a negative number. When the level of the epithelial attachment is on root structure and the free margin of the gingiva is at the CEJ, the attachment loss equals the probing depth, and the recession is 0. In a situation in which there is increased periodontal destruction and recession, the loss of attachment measurement equals the probing depth plus the measurement of recession19 (see Fig. 1-18B and C). Clinical attachment loss is a measure of periodontal destruction at a site, rather than current disease activity, and it may be considered the diagnostic “gold standard” for periodontitis.20 It should be documented in the initial periodontal examination.21 It is an important consideration in the devel opment of the overall diagnosis, treatment plan, and prognosis of the dentition and can be an effective research tool.
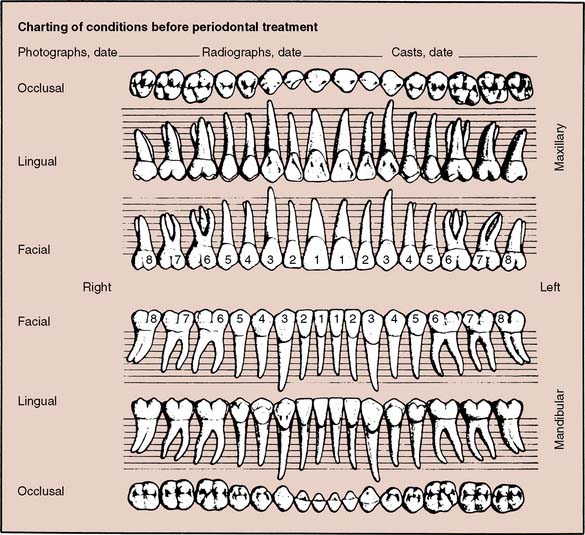
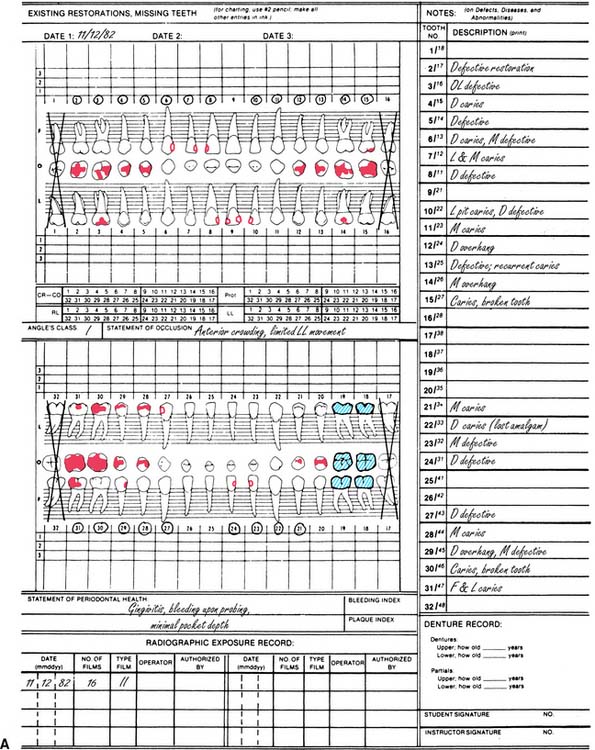
Dental Charting
An accurate charting of the state of the dentition reveals important information about the condition of the teeth and facilitates treatment planning. Adequate charting (Fig. 1-19), in addition to all periodontal information, must show the presence or absence of teeth, dental caries, restorations, wear faceting and abrasions, fractures, malformations, and erosions. Missing teeth often have an effect on the position of adjacent teeth (see also the section on arch integrity in Chapter 3). Similarly, the presence of dental caries on one interproximal surface should alert the examiner to carefully inspect the adjacent proximal wall, even if caries is not apparent radiographically. The degree and extent of caries development over time can have a considerable effect on the eventual outcome of fixed prosthodontic treatment. The condition and type of the existing restorations are noted (e.g., amalgam, cast gold, composite resin, all-ceramic). Open contacts and areas where food impaction occurs must also be identified. The presence of wear facets is indicative of sliding contact sustained over time and thus may indicate parafunctional activity (see Chapter 4). Wear facets are often easier to see on diagnostic casts, however (see Chapter 2); during the clinical examination, the location of any observed facet is recorded. Fracture lines in teeth may necessitate fixed prosthodontic intervention, although minor hairline cracks in walls that are not subject to excessive loading can often go untreated and simply be observed at recall appointments (see Chapter 32). The location of fractures should be indicated on the chart, as should any other abnormalities.
Occlusal examination
The initial clinical examination starts with the clinician’s asking the patient to make a few simple opening and closing movements while the clinician carefully observes the opening and closing strokes. The objective is to determine to what extent the patient’s occlusion differs from the ideal (see Chapter 4) and how well the patient has adapted to this difference. Special attention is given to initial contact, tooth alignment, eccentric contacts, and jaw maneuverability.
Initial tooth contact
The relationship of teeth in both centric relation (see Chapter 4) and the maximum intercuspation should be assessed. If all teeth come together simultaneously at the end of terminal hinge closure, the centric relation (CR) position of the patient is said to coincide with the maximum intercuspation (MI) (see Chapters 2 and 4). The patient is guided into a terminal hinge closure to detect where initial tooth contact occurs (see the sections on bimanual manipulation and terminal hinge closure in Chapters 2 and 4). The clinician should ask the patient to “close feather-light” until any of the teeth touch and to have the patient help identify where that initial contact occurs by asking him or her to point at the location. If initial contact occurs between two posterior teeth (usually molars), the subsequent movement from the initial contact to the MI position is carefully observed and its direction noted. This is referred to as a slide from CR to MI. The presence, direction, and estimated magnitude of the slide are recorded, and the teeth on which initial contact occurs are identified. Any such discrepancy between CR and MI should be evaluated in the context of other signs and symptoms that may be present (e.g., elevated muscle tone previously observed during the extraoral examination, mobility on the teeth where initial contact occurs, wear facets on the teeth involved in the slide).
General alignment
The teeth are evaluated for crowding, rotation, supra-eruption, spacing, malocclusion, and vertical and horizontal overlap (Fig. 1-20). Teeth adjacent to edentulous spaces often have shifted position slightly. Small amounts of tooth movement can significantly affect fixed prosthodontic treatment. Tipped teeth affect tooth preparation design or, in severe cases, may result in a need for minor tooth movement before restorative treatment. Supra-erupted teeth are often overlooked clinically but frequently complicate fixed dental prosthesis design and fabrication.
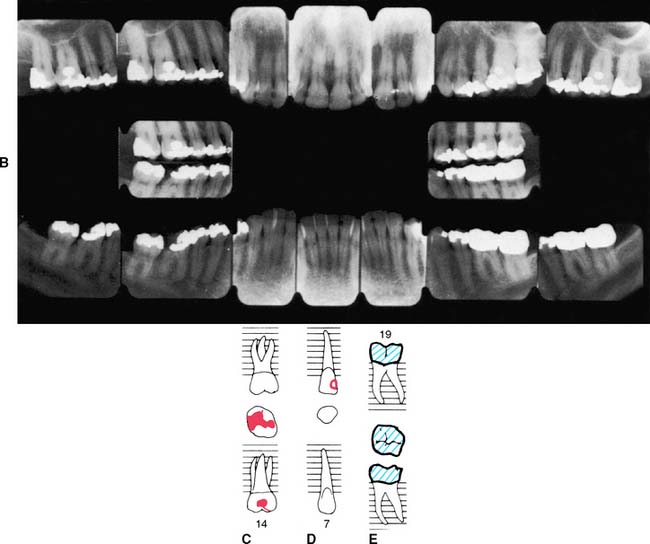
Lateral and protrusive contacts
Excursive contacts on posterior teeth may be undesirable under certain circumstances (see Chapter 4).
The patient is then guided into lateral excursive movements, and the presence or absence of contacts on the nonworking side and then the working side is noted. Such tooth contact in eccentric movements can be verified with a thin Mylar strip (shim stock). Any posterior cusps that hold the shim stock are evident (Fig. 1-21). Teeth that are subject to excessive loading may develop varying degrees of mobility. Tooth movement (fremitus) should be identified by palpation (Fig. 1-22). If a heavy contact is suspected, a finger placed against the buccal or labial surface while the patient lightly taps the teeth together helps locate fremitus in MI.
Jaw maneuverability
The ease with which the patient moves the jaw and the way it can be guided through hinge closure and excursive movements should be assessed, because these factors are a good guide to neuromuscular and masticatory function. If the patient has developed a pattern of protective reflexes, manipulating the jaw is difficult. The patient’s restricted maneuverability is recorded.
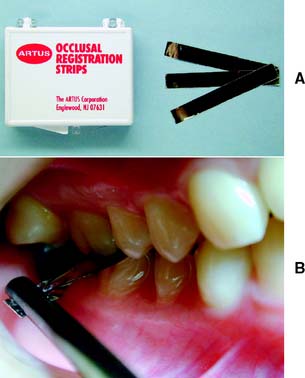
Radiographic Examination
Radiographs provide essential information to supplement the clinical examination. Detailed knowledge of the extent of bone support and the root structure of each standing tooth is essential for establishing a comprehensive fixed prosthodontic treatment plan. Although radiation exposure guidelines recommend limiting the number of radiographs to only those that will result in potential changes in treatment decisions, a full periapical series (Fig. 1-23) is normally required for new patients so that a comprehensive fixed prosthodontic treatment plan can be developed. Patient exposure can be minimized by using a technique that provides the most information with a minimal need for repeat films and by using appropriate protection. The use of digital radiography can further help reduce radiation exposure.
Panoramic films (Fig. 1-24) provide useful information about the presence or absence of teeth. They are especially helpful in assessing third molars and impactions, evaluating the bone before implant placement (see Chapter 13), and screening edentulous arches for buried root tips. However, they do not provide a sufficiently detailed view for assessing bone support, root structure, caries, or periapical disease.
Special radiographs may be needed for the assessment of TMJ disorders and a wide variety of pathologies ranging from bone and mineral disorders to metabolic disorders, genetic abnormalities, and soft tissue calcifications such as carotid artery calcification.21 For assessment of the TMJs, a transcranial exposure (Fig. 1-25), with the help of a positioning device, reveals the lateral third of the mandibular condyle and can be used to detect structural and positional changes. However, interpretation may be difficult,22 and more information may be obtained from other images23 (Fig. 1-26).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses