CHAPTER 1
Craniofacial Growth and Development
Clinicians require a basic understanding of growth and development in order to properly plan treatments and evaluate treatment outcomes. As determined by the World Health Organization, growth and development provides one of the best measures available of individuals’ health and well-being. Knowledgeable clinicians understand that general somatic growth provides important information about their patients’ overall size, maturity status, and growth patterns. Because the timing of maturity events, such as the initiation of adolescent or attainment of peak growth velocity, is coordinated throughout the body, information derived from stature or weight can be applied to the craniofacial complex. In other words, the timing of peak height velocity (PHV)—a noninvasive and relatively easily obtained measure—can be used to determine the timing of peak mandibular growth velocity. Knowledge of general somatic growth is also useful when evaluating the sizes of patients’ craniofacial dimensions. An individual’s height and weight percentiles provide a measure of overall body size, against which craniofacial measures can be compared. For example, excessively small individuals (i.e., below the 5th percentiles in body size) might also be expected to exhibit a small craniofacial complex. Finally, the reference data available for somatic growth and maturation are based on large representative samples, making them more generally applicable and more precise at the extreme percentiles than available craniofacial reference data.
Postnatal craniofacial growth is a complex, but coordinated, ongoing process. The cranial structures are the most mature and exhibit the smallest relative growth rates, followed by the cranial base, and then the maxillary and mandibular structures, which are the least mature and exhibit the greatest growth potential. Knowledge about a structure’s relative growth is important because it serves, along with heritability, as an indicator of its response potential to treatment and other environmental influences. It is essential that clinicians understand that the maxilla and mandible, the two most important skeletal determinants of malocclusion, follow similar growth patterns. Both are displaced anteriorly and, especially, inferiorly; both tend to rotate forward or anteriorly; both rotate transversely; and both respond to displacement and rotation by characteristic patterns of growth and cortical drift. It is also useful to understand that patients should be expected to adapt skeletally to orthodontic, orthopedic, and surgical interventions and that the adaptations mimic growth patterns exhibited by untreated patients. Perhaps most importantly, clinicians must understand the tremendous therapeutic potential that the eruption and drift of teeth provide. The maxillary molars and incisors, for example, undergo more eruption than inferior displacement of the maxilla, making them ideally suited for controlling vertical and AP growth.
Clinicians also often do not appreciate that adults show many of the same growth patterns exhibited by children and adolescents, simply in less exaggerated forms. It has been well established that craniofacial growth continues though the 20s and 30s, and perhaps beyond. Skeletal growth of adults appears to be predominately vertical in nature, with forward mandible rotation in males and backward rotation in females. The teeth continue to erupt and compensate depending on the individual’s growth patterns. Adults also exhibit important soft tissue changes; the nose grows disproportionately and the lips flatten. Vertical relationships between the incisors and lips should also be expected to change with increasing age.
Finally, malocclusion must be considered as a multifactorial developmental process. Although genes have been linked with the development of Class III and perhaps Class II division 2 malocclusions, the most prevalent forms of malocclusions are largely environmentally determined. Equilibrium theory and the notion of dentoalveolar compensations provide the conceptual basis for understanding how closely linked tooth positions are with the surrounding soft tissues. They also make it possible to predict the type of compensations that should be expected. For example, they explain why the development of malocclusion is associated with various habits, assuming the habits occur regularly and are of long enough duration. In fact, anything that alters mandibular posture might be expected to elicit skeletal and dentoalveolar compensations. This explains why individuals with chronic airway obstructions develop skeletal and dental malocclusions that are phenotypically similar to malocclusions associated with weak craniofacial musculature; both populations of patients posture their mandibles similarly and undergo similar dentoalveolar and skeletal compensations. Based on the foregoing, the following questions are intended to provide a basic—although only partial—understanding of growth and development and its application to clinical practice.
1 At what ages do most children enter adolescence, and when do they attain PHV?
The adolescence growth spurt starts when decelerating childhood growth rates change to accelerating rates. During the first part of the growth spurt, statural growth velocities increase steadily until peak height velocity (PHV) is attained. Longitudinal assessments provide the best indicators of when adolescence is initiated and PHV is attained. Longitudinal studies pertaining to North American and European children< ?xml:namespace prefix = "mbp" />
2 What is the mid-growth spurt, and how does it apply to craniofacial growth?
The mid-growth spurt refers to the increase in growth velocity that occurs in some, but not all, children several years before the initiation of the adolescent growth spurt. Mid-growth spurts in stature and weight have been reported to occur between 6.5 and 8.5 years of age; they tend to occur more frequently in boys than girls.
3 Which skeletal indicators are most closely associated with PHV?
According to Grave and Brown,
4 What is the equilibrium theory of tooth position?
Although Brodie
Proffit,
He further noted that extrinsic pressures, such as habits and orthodontic forces, can alter equilibrium, provided that they are sustained for at least 6 hours each day. Proffit
5 What is the prevalence of Class II dental malocclusion among adolescents and young adults living in the United States?
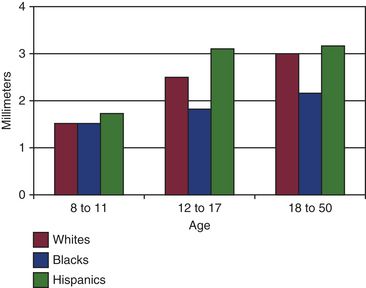
The best direct epidemiologic evidence comes from the National Health Survey,
6 What is the prevalence of incisor crowding among individuals living in the United States, and how does it change with age?
According to the initial NHANES III data,
7 Do the third molars play a role in determining crowding?
Although third molars have been related with crowding,
8 How does horizontal and vertical mandibular growth affect crowding?
Vertical growth makes the maintenance of lower incisor alignment after orthodontic treatment more problematic. Based on the notion that the lower incisors are carried into the lower lip as the mandibula grows anteriorly or rotates downwards, late mandibular growth has been suggested as a major contributor to post-retention crowding.
9 How much should the mandibular incisors and molars be expected to erupt during adolescence?
Based on natural structure superimpositions of the mandible performed between 10 and 15 years of age, McWhorter
10 How does untreated arch perimeter change between the late primary dentition and the permanent dentition?
Computed based on a centenary curve extending from the mesial of the first molar to mesial of first molar,
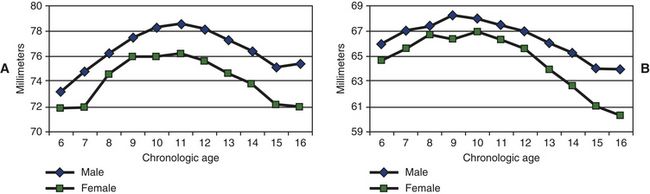
FIG 1-3 Maxillary (A) and mandibular (B) arch perimeters between 6 and 16 years of age.
(Adapted from Moyers RE, van der Linden FPGM, Riolo ML, McNamara JA Jr. Standards of human occlusal development. Monograph #5, Craniofacial Growth Series, Center for Human Growth and Development, University of Michigan, Ann Arbor, Michigan, 1976.)
11 How do untreated maxillary and mandibular intermolar widths change during childhood and adolescence?
Bishara and colleagues
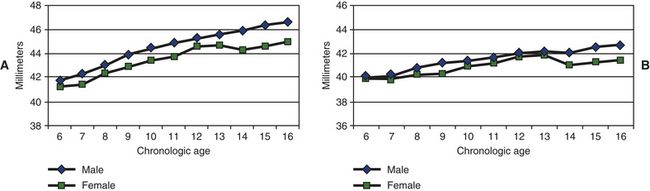
FIG 1-4 Maxillary (A) and mandibular (B) intermolar widths between 6 and 16 years of age.
(Adapted from Moyers RE, van der Linden FPGM, Riolo ML, McNamara JA Jr. Standards of human occlusal development. Monograph #5, Craniofacial Growth Series, Center for Human Growth and Development, University of Michigan, Ann Arbor, Michigan, 1976.)
12 Without treatment, how do maxillary and mandibular arch depths change during childhood and adolescence?
Maxillary and mandibular arch depths, midline distances between a line tangent to the incisors, and a line drawn tangent to the distal crown of the deciduous second molars or their permanent successors show different patterns of growth changes. Maxillary arch depth increases 1.4 and 0.9 mm in males and females, respectively, during the eruption of the permanent incisors.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses