1
Corticotomy-facilitated orthodontics: Clarion call or siren song
Neal C. Murphy,1,2 M. Thomas Wilcko,2 Nabil F. Bissada,2 Ze’ev Davidovitch,1,3 Donald H. Enlow,1 and Jesse Dashe4
1 Department of Orthodontics, Case Western Reserve University School of Dental Medicine, Cleveland, OH, USA
2 Department of Periodontics, Case Western Reserve University School of Dental Medicine, Cleveland, OH, USA
3 Department of Orthodontics, Harvard University School of Dental Medicine, Cambridge, MA, USA
4 Department of Orthopedic Surgery, Boston University Medical Center, Boston, MA, USA
Preface
All Men by nature desire knowledge.
Aristotle
This chapter attempts to create an intellectual matrix within which other contributors writing about orthodontically driven corticotomies – also known as surgically facilitated orthodontic therapy (SFOT) – find both justification and inspiration with a modicum of practicality. The corticotomy, a selective alveolus decortication (SAD) of the alveolus bone, is but one in a family of related procedures encompassed by the inchoate field of SFOT. This treatise, by the very nature of the subject, focuses more on science than orthodontic art. And that science is orthodontic (bone) tissue engineering (OTE).
Yet, the emphasis on bone engineering during orthodontic tooth movement (OTM) promises much more than an alternative protocol or new clinical gadgetry. This chapter, in the context of an historical review, presents an evolution (and a clash) of ideas to reveal universal biologic principles. It is these principles, these transcendent truths, that should be applied to particular clinical events in a meaningful and rewarding manner. The student of SFOT should not indulge in mindless dedication to one technical recipe without understanding the specific biologic mechanisms and therapeutic objectives that define it.
The ideas and procedures of SFOT herein are increasingly being employed with great success worldwide despite the natural impediments of healthy skepticism and unintentional misrepresentation. Importantly, this global popularity is forging a new identity for those who wish to embrace it. Twenty-first-century orthodontists, periodontists and other surgeons are becoming international citizens endowed with skills and intellects of global scientists, forming a mastermind that is liberated from “brick and mortar”, national, or even regional biases. We comment on that emergent event as doctors who have participated in a nascent science; we witnessed its birth, watched it develop, and remain ever fascinated by it. The contents of this book lend credence to that new identity and the authors personify the spirit of free inquiry that sustains it. Yet, in our zeal to share knowledge, we posit most humbly that we are merely the messengers.
Introduction
Conceptual issues
The title of this chapter is not a question; it is an existential choice. Because the history of the corticotomy presents thematic questions much more profound than where one should make surgical cuts, some explanation of this chapter’s syntactical style is in order. The historical journey of the orthodontic specialty reflects a similar kind of thematic development replete with controversy. Throughout that rocky sojourn, two contentious themes have always emerged. The first is whether the essence of orthodontic practice is art or science. The resolution of this dichotomy is that orthodontics is neither and both. Art and science are merely two different but complementary perspectives of the world. So conflict between these two worldviews is actually quite illusory. It is resolved only by realizing that arts and sciences are merely tools, intellectual instruments with which we achieve a nobler mission: our humanitarian endeavor of caring for others. Still, the two classic perspectives always prevail and must be constantly rebalanced: humanistic art as the ends, science as the means.
The second theme, a perennial conflict between extraction and non-extraction protocols, is more philosophically relevant to our topic. One of the great advantages of SFOT is that alveolar bone can be reshaped to accommodate an idealized dental arch rather than modifying a dentition to “inferior bone.” An historical drag on this progressive trajectory is the assumption that the alveolus bone is immutable. It is not; the alveolus bone is remarkably malleable.
So, in a way, the new realization that the alveolus bone is malleable and the ability to “build a better bone” renders the extraction–expansion debate somewhat moot. With a “new biology” of orthodontics this historical debate has been rendered simplistic and false, just as epigenetics has rendered the nature–nurture debate an anachronistic dichotomy in the face of evolutionary sciences.
Our historical review cannot dictate where art ends and science begins in the mind of each orthodontist, for as every flower is beautiful, yet every flower is unique. And the sensitive orthodontist takes each individually unique “flower” to full bloom in its own season using both art and science. Likewise, one cannot dictate to every orthodontist exactly when extractions in particular should or should not be prescribed. One can only disclose a wider scope of therapeutic options, to achieve high-quality care. And, to many, quality is an event; namely, the coincidence of doctor talent with patient expectations in a universe of humanistic but rational achievement. This is the tacit mission of this textbook and its selfless contributors.
When dealing with facial esthetics the artistic imperative is undeniable and the decision to extract or not to extract reflects individual interpretations of timeless principles. Most art is intuitive. Yet even art – namely, impressions, culturally influenced in the aggregate and subjectively sensed in the individual – is not totally beyond the reach of scientific scrutiny. And, for better or worse, scientific scrutiny must always be the abiding companion of the 21st-century doctor. This is because contemporary practice, whether engaged with biological principles or indulged in psychosocial imperatives, operates in a postmodern world that demands demonstrable scientific proofs where we find them or (at least) compelling biological rationales where we can divine them. History reveals the former and justifies the latter.
In this chapter, our methods are innovative, and admittedly somewhat polemical. We do not merely report a litany of events and experimental results. We cleave existing basic science to pertinent clinical data and synthesize them with traditional protocols. This hopefully will fortify what is done right by explaining it and provide alternatives to what can go wrong by explicating errors from their historical context.
When innovative science is seen through the lens of historical context, two important revelations occur. First, sophisticated insights of nuance are clarified (e.g., bony block movement versus enhanced physiology); and second, some new ideas are revealed simply as “old wine in new bottles” (normal healing, the regional acceleratory phenomenon – see 1983: Frost and his regional acceleratory phenomenon). This chapter will undoubtedly serve some old wine, but that insight does not diminish its worth. The historical context merely legitimizes the insights as more salient and timeless.
Through the gauntlets of criticism and the civil internecine bickering that often characterizes our specialties, it is curious indeed how truth emerges. Yet it is important to note that an assiduous intellectual analysis, emancipated from the strictures of dogma, and inspired by intrepid pioneers who have preceded us, is what sets the tone for this chapter and perhaps even the textbook itself. Query: is it nobler to suffer the indignities of dogmatic tradition or bear the yoke of exciting innovation? The former is safe, but the latter is tantalizing since it unravels the nettlesome enigmas of biology.
We must choose the latter despite the fact that unraveling mysteries is politically and philosophically risky when it exposes hues of uncomfortable truth. But the explication of truth is our deontological duty, because we have the power to control the welfare of other human beings, and that duty imposes a fiduciary standard more exalted than the “treatment to the norm (average).” Axiomatic to all clinical endeavors is the view that treating patients is a privilege, not a right, and a privileged position demands excellence, not mediocrity.
Dedication
John Donne reminds us that “no man is an island, entire of itself,” and this chapter is a collaborative exemplar of that reality. Yet, the exciting frontiers of oral tissue engineering herein belong to neither our venerable teachers alone nor the seasoned clinicians who wrote this chapter. Rather, the future and our efforts are dedicated to those who will enjoy a longer tenure of equity in the specialty than we. This chapter is dedicated to them: the young idealists still seeking a place in the pantheon of clinical science.
Arete
The nature of the phenomenon: intuited early, defined late
Diction and definitions
For the purposes of expediency and ease of reading, certain terms will depart their strict scientific definitions to be used in a liberal sense. The terms “corticotomy” and “SAD” will be used synonymously, and “mobilization” will be interchangeable with “luxation,” meaning the physical jarring, fracturing, or cracking of bone. Surgically facilitated orthodontic therapy means any cutting of tissue that makes orthodontic treatment work better or faster. Other terms will submit to strict definition.
From osteotomy to corticotomy to tissue engineering
When reviewing the history of corticotomies one discovers that it originated in attempts to minimize the harsh side effects and risks of segmental osteotomy. And this history is complicated by the fact that early writers used the terms osteotomy and corticotomy synonymously. So much of the early literature is vague and prone to misinterpretation. An osteotomy starts with a linear decortication of bone and ends with a physical movement of a section of bone the way one might break a twig from the branch of a tree. Thus, “mobilization” is a kind of purposeful fracturing of bone, sometimes literally done with a mallet and chisel to move physical parts, whereas a corticotomy is limited to the initial incision to modify physiology without luxation or fracture. When studying SFOT one must keep in mind the fundamental effects and esoteric mechanisms that facilitate the phenomena.
These effects, “observed” in the mind of the surgeon during the operation, occur subclinically at the tissue and cell levels. They are less clearly defined than clinic-level gross anatomy, a level to which most orthodontists are accustomed. Therefore, new modes of thinking must occur that could not have been appreciated by the specialty’s earlier advocates. However, these histological mechanisms may have been singularly intuited by John Nutting Farrer (1839–1913) as early as 1888. He was referring to orthodontic tissue effects from a “whole alveolus bone” perspective when he wrote (emphasis added):
The softening of the socket breaks the fixedness or rigidity of the tooth leaving it comparatively easy to move, either by resorption of the tissues or by bending of the alveolar process or both.
Histophysiology of orthodontic-driven corticotomy
The “whole-bone perspective” is a new way of looking at alveolar bone reactions to orthodontic forces that goes beyond the narrow perspective of the periodontal ligament or a focus on the midpalatal sutures. This “NewThink” attempts to preclude retruded profile risks of extraction therapy. Williams and Murphy (2008) documented, with unequivocal biopsy images, that lingual forces can stimulate labial subperiosteal (compensatory) osteogenesis by showing samples of labial woven bone where the alveolus was expanded slowly from the lingual aspect. It should be noted, however, that any claim of permanent bone alteration with Williams and Murphy’s appliances or surgical phenotype re-engineering cannot be made before 3–4 years into the retention stage when the calcification is complete to an osseous “steady state” (dynamic equilibrium). Inherent in Williams and Murphy’s philosophy is the assumption that emerging esthetic standards are shifting toward “full facial” esthetics quite different from the classic retruded profile of Apollo Belvedere (Angle’s esthetic standard). This philosophy is not only compelling because of his biopsy evidence of alveolus development, but also because of its natural appeal to good common sense.1
The osteogenic effects demonstrated by Williams and Murphy (2008) in the alveolar subperiosteal cortices in nonsurgical cases capture exactly the histophysiology of corticotomy surgeries. Surgery simply elicits the phenomenon more dramatically and faster. The theoretical concept had been alluded to previously and was most recently expanded in the excellent textbook by Melsen (2012), where it refers to a “…change in surface curvature of the alveolar walls.” All contemporary orthodontists should read this most enlightened summary of basic alveolar osteology to fully understand bone strain in all patients (Verna and Melsen, 2012). This “whole-bone” perspective posits the alveolus bone, cf. alveolar “process,” as a separate operative organ independent of its subjacent corpus. As the whole bone is orthodontically bent, each osteon is deformed. The “peri-orthodontic hypothesis” (Murphy, 2006) contends that this bends protein molecules and DNA, opening obscure binding sites on important molecules to elicit an epigenetic perturbation and redesigning the morphogenesis to a novel phenotype unique in alveolus in shape, mass, and volume. The value of this new perspective is that it conforms well with contemporary basic biological sciences, particularly molecular biology and epigenetics.
In this regard, alveolar subperiosteal tissue and periodontal ligament act no differently than the periosteum and endosteum respectively in any long bone (Figure 1.1).
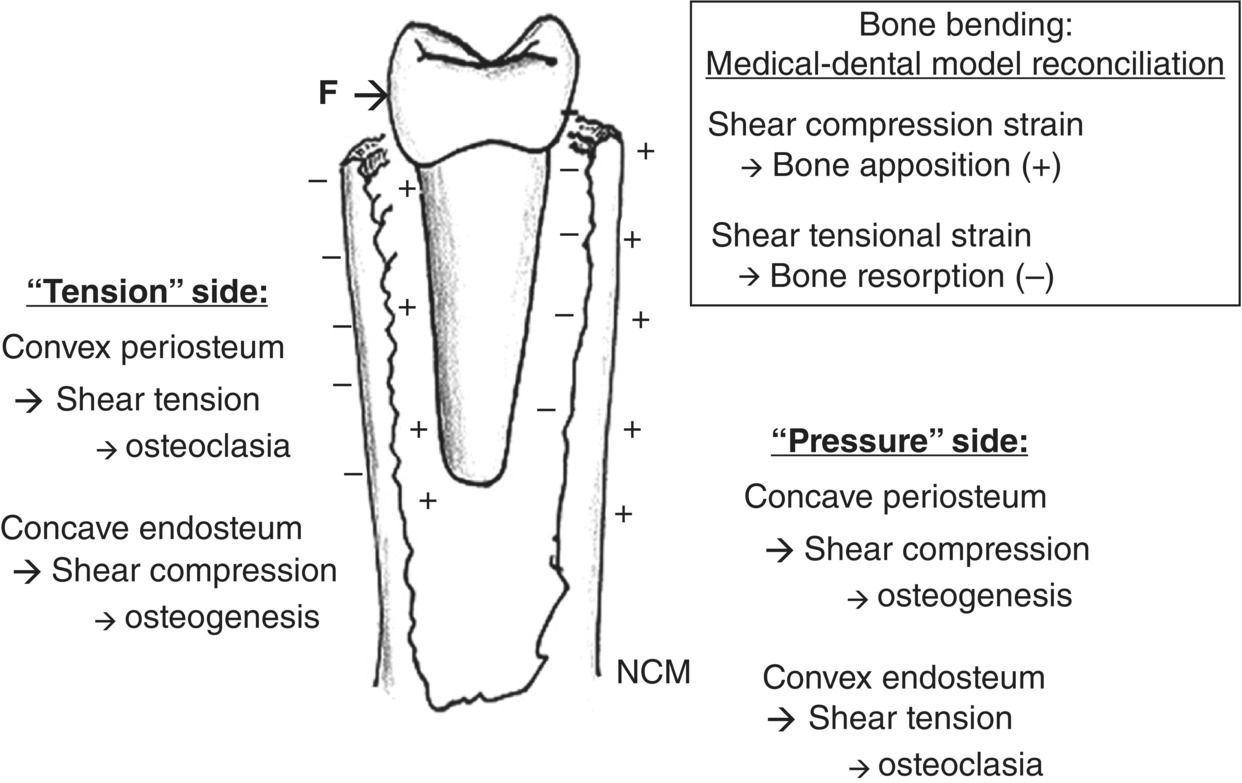
Figure 1.1 It is important to realize that SAD and particularly PAOO/AOO can change the configuration of the alveolus bone regardless of the form of the underlying maxillary or mandibular corpus. This apparently occurs by subperiosteal appositional osteogenesis stimulated by shear compression and shear tension on the facial and lingual cortices. In this respect, the periodontal ligament acts like endosteum in long bones. This realization resolves the ostensible conflict with the medical orthopedic claims that pressure is osteogenic and tension has osteoclastic effects, in contrast to the traditional orthodontic pressure–tension hypothesis that has been criticized so much in recent literature. This perspective does not deny that ischemic necrosis occurs in the periodontal ligament, but merely expands the biological concept of orthodontic histology beyond the ligament. This resorption on the so-called “pressure” side may be more related to osteogenic shear tension (–) in the cribriform plate similar to long bone homologues. On the so-called “tension” side, an increase in concavity of the cribriform plate is evident causing shear compression (+), which is osteoclastic in long bones.
Therefore, a lot of recent medical and basic orthopedic science can be transferred to and from alveolus bone science. This phenomenon, facilitated by corticotomy protocols, we believe may be employed to reduce the degree of clinical relapse that still plagues orthodontics after 100 years of clinical trial and error. Standard orthodontic protocols, without surgery, cannot overcome the natural tissue “canalization” that resists phenotype change (Waddington, 1957; Siegal and Bergman, 2002; Slack, 2002; Stearns, 2002).
Cell-level orthodontics
Bone cells, and homologues in other tissues as well, sense changes in their mechanical environments, internally throughout the cytoskeleton and externally through focal adhesions to the extracellular matrix (Benjamin and Hillen, 2003; Murphy 2006; Verna and Melsen, 2012). This area of cell-level biomechanics was essentially beyond the control of most orthodontists, who relied instead on gross anatomical and clinical events to intuit cellular activity. With the introduction of tissue engineering concepts and a revival of corticotomy-facilitated orthodontics, a new interest in cell- and tissue-level phenomena has appeared in the dawn of the 21st century.
Induced mechanical stimuli not only change the internal cytoskeleton but – by epigenetic perturbations – can determine internal stereo-biochemistry and ultimate morphogenesis. To the extent that wound healing recapitulates regional ontogeny, orthodontic modulation of the healing bone wound can engineer a new phenotype ideally suited for an ideal dental alignment and dental arch juxtaposition even to the point of modifying the need for orthognathic surgery. The alveolus bone, which lives, thrives and dies by virtue of its functional matrix (Moss, 1997), the dental roots, are especially responsive to therapeutic intervention in this regard because of behavioral imperatives identified by Wolff’s law and Frost’s “mechanostat” model (Frost, 1983).
What skeletal muscle can do to bone morphogenesis at the gross anatomical level is similar to the effects of microstrain at the cell/tissue, whether that be hypertrophy, hyperplasia, or atrophy, thus demonstrating that engineering bone morphogenesis is a threshold phenomenon; that is, too much or too little is dysfunctional. It should be remembered that the influences of mechanical stimuli at the cell and tissue levels, mechanobiology, lie not only the domain of bone alone. Indeed, the even pathoses of atherosclerotic cardiovascular disease are directly related to mechanobiological changes in vessel walls. With modern analytic methodologies and a burgeoning body of science, too extensive for the scope of this writing,2 responses to all tissue can now be studied and actually modulated, be they integumental or neuronal, mucosal or bony. This is the essence of tissue engineering science. Thus, orthodontic scientists have a legitimate equity claim in mechanobiological fathoms as well. So, there is no reason they should not be involved considering the critical importance of their domain, the face of a human child.
The study of cell/tissue-level orthodontic therapy, especially the nature of genetic expression evident in healing bone wounds, suggests that orthodontic relapse can be seen as a simple reversion to original phenotype, regardless of the method used. That is why some SFOT has been proven to be a popular – in some cases manifestly superior (Dosanjh et al., 2006a,b; Nazarov et al., 2006; Walker et al., 2006a,b) – and professionally acceptable adjunct to traditional orthodontic therapy. The evidence of efficacy that this innovation enjoys lends both clinical quality and stability to OTM, justifying it as a reasonable therapeutic enhancement. There are advantages and disadvantages with both conventional OTM and SFOT, and it is only fair to patients that they be made aware of all treatment alternatives. At the clinical level, SAD is termed the Periodontally Accelerated Osteogenic Orthodontics™ (PAOO) technique or the Accelerated Osteogenic Orthodontics™ (AOO)3 technique only when a bone graft is added, and these two terms can be used interchangeably. The lead author prefers to use PAOO when there is periodontal involvement and AOO when the periodontium is healthy.
Experience suggests that, in most cases, demineralized human bone graft or viable stem cell (allograft) therapy (SCT) should provide a predictable outcome. A non-surgical derivative, trans-mucosal perforation (TMP), (Murphy, 2006) can be employed when flap surgery is not indicated in small areas with excess bony support.
A history of the orthodontic-driven corticotomy (overview)
Origin of the concept
Cano et al. (2012), as with other authors, generally attribute the first published surgical method to facilitate orthodontic therapy to Cunningham (around 1894) after his lecture in Chicago the previous year. While having some rudimentary characteristics in common with modern corticotomies, close scrutiny of Cunningham’s SFOT procedure suggests it was really a luxated segmental osteotomy. Cunningham’s singular goal of making teeth move faster has since evolved to more global objectives, and variations on the corticotomy theme have spawned interesting incarnations throughout the 20th and 21st centuries in many different countries and cultures.
These variants evolved in a progression of surgical refinements designed to (a) accelerate OTM, (b) limit the quantity and pathologic potential of the inevitable bacterial load, (c) enhance stability, and (d) reduce the morbidity of orthognathic alternatives. As Cunningham’s crude luxating osteotomy evolved, the term “corticotomy” emerged in the clinical lexicon with its approximate and more disciplined synonym, SAD. So both terms may be used as roughly synonymous for practical purposes.
But it should be noted that SAD with OTM will not grow new bone mass. In fact, in an adult, steady-state alveolus treatment may ostensibly slightly reduce alveolar bone mass. This is described in the non-surgical orthodontic literature as “moving bone out of the alveolar housing.” So applying Cunningham’s derivatives indiscriminately may indeed result in a net loss of supporting bone. This dilemma was solved by altering phenotype and creating additional bone de novo (Figure 1.2). Developing bone de novo has graced orthodontics exclusively through the prodigious efforts of many doctors in the Wilckodontics research groups, which are represented academically at Case Western Reserve University (Cleveland, OH, USA) by the second author. When grafted demineralized bone matrix (DBM)4 (circa 1998) and viable cell allografts entered the SAD protocol, the thresholds of bone tissue engineering (Murphy, 2006) and SCT (Murphy et al., 2012) were breached. This subsequently defined the dentoalveolar surgeon and orthodontist as partners in surgical dentoalveolar orthopedics and alveolar osteology.
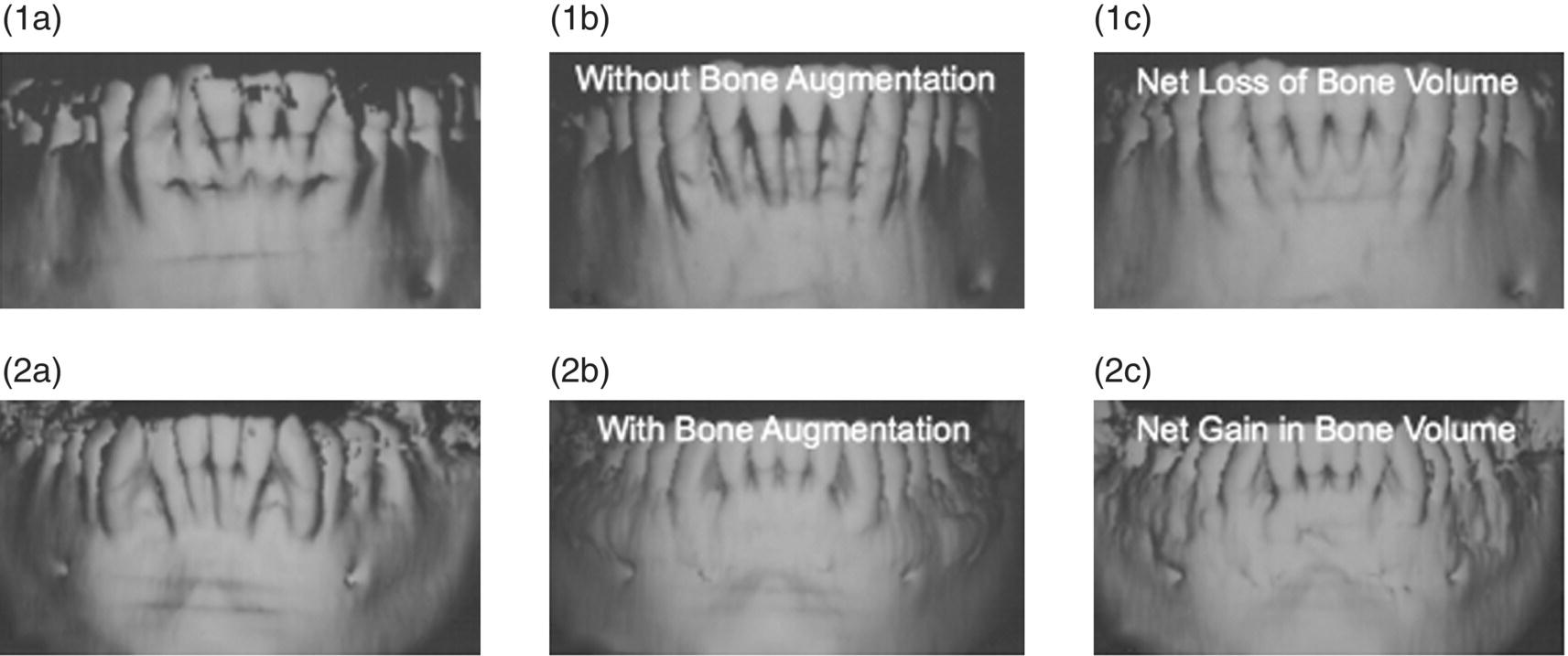
Figure 1.2 (1a) Comparison of SAD with (PAOO/AOO) and without a bone graft demonstrating the necessity for grafting when insufficient bony support is evident in adults. The figure shows the pre-treatment high-resolution computerized tomography (CT) scan (accurate to 0.2 mm) of the lower arch of a female, age 39, prior to having circumscribing corticotomy cuts performed both labially and lingually around the six lower anterior teeth. Note the arch length deficiency (overlap crowding), the pronounced crestal glabella, and the distance between the crest of the alveolus and the corresponding cemento-enamel junctions (CEJs). Clinically, the circumscribing corticotomy cuts resulted in the appearance of outlined “blocks of bone” connected by medullary bone. The total treatment time for this case was 4 months and 2 weeks with eight adjustments appointments. (1b) At 1 month retention the integrity of the outlined “blocks” of bone appears to have been completely lost and the layer of bone over the labial root surfaces appears to have vanished. In reality, this layer of bone has undergone demineralization as the result of a normal osteopenic state (RAP); the soft tissue matrix of the bone remains but is not visible radiographically. This is why radiographic assessments of expansion cases before 3–4 years in retention, while interesting in the short term, are premature for final policy conclusions. This demineralized matrix was carried into position with the root surfaces (bone matrix transportation). (1c) This shows the high-resolution CT scan at 2years and 8 months retention. Note that the layer of bone over the root surfaces has only partially reappeared due to the remineralization of the soft tissue matrix. This suggests that there may have been a net loss of bone volume in this adult. In adolescents this is not seen. Owing to a greater regenerative potential there seems to be a complete regeneration of bone after SAD. (2a) This shows a high-resolution CT scan of the lower arch of a male, age 23, prior to circumscribing corticotomy cuts being performed both buccally and lingually around all of the lower teeth with a large bone graft placed over the corticotomized bone. Note the paucity of bone over the buccal root surfaces. The total treatment time was 6 months and 2 weeks with 12 adjustment appointments. (2b) At 3 months retention the labial root surfaces are now covered with an intact layer of newly engineered phenotype appropriate for the new position of tooth roots (the functional matrix of the bone).The pre-existing paucity of bone over the lingual root surfaces has been corrected in the same manner so that the roots of the teeth are now “sandwiched” between intact layers of bone both buccally and lingually. There has been a net increase in bone volume. (2c) At 2 years and 8 months retention the increase in the alveolar volume has been maintained. These data argue for PAOO/AOO in non-growing orthodontic patients where dental arch expansion is considered.
New ideas often do not fit easily into old paradigms (Kuhn, 2012), so a new Weltanschauung,5 (Freud, 1990) coined “NewThink”, must be embraced to mark a clear distinction between the philosophy behind new orthodontic-driven corticotomy protocols (Pirsig’s dynamic quality) and traditional orthodontic art of wire and plastic bending (Persig’s static quality6).
The SFOT we describe here purposely executes OTM through a healing bone wound or bone graft eliciting a purposely delayed wound maturation. This occurs by perpetuating a natural bone “callus” or osteopenia until all the teeth are ideally aligned, coordinated, and detailed. This kind of surgery is decidedly not merely a variation of a basic surgical theme of the manner in “rearranging anatomical parts” like so many Lego® children’s toys. Parts rearrangement is the stuff of orthognathic osteotomies. In stark contrast, the corticotomy-facilitated therapy does not create anatomical fragments or separate “parts.” Corticotomies re-engineer physiology. Specifically SFOT, SAD, PAOO/AOO and TMP seek to re-engineer epigenetic potential in both the basic physiology of healing and ultimate morphogenesis at the molecular level of DNA and (endogenous and grafted) stem cells.
Early concepts: German pioneers
While Cunningham’s procedure seemed bold to many American orthodontists, it soon became popular in the German scientific community. Cohn-Stock (1921), citing “Angle’s method,” removed the palatal bone near the maxillary teeth to facilitate retrusion of single or multiple teeth, and a host of German Zahnartzen followed his lead. Later, Skogsborg (1926) divided the interdental bone, with a procedure he called “septotomy,” and a decade later Ascher (1947) published a similar procedure, claiming that it reduced treatment duration by 20–25%.
As good as it may appear, the scientific literature of the 20th century seems to have missed the central purpose of SFOT, SAD and PAOO/AOO, and TMP. This illustrates a social phenomenon where older, more experienced but doctrinaire, clinicians see innovation not in the context it promises, but rather in the context of the status quo. This is an unfortunate but common event seen best in retrospect. This bias and the lack of modern biological standards is the reason why some literature of this period is merely anecdotal, dismissive and often patently incorrect. Yet, ironically, this body of data is still cited as authoritative and used to justify specious criticisms of 21st-century dentoalveolar surgery.
1931: Bichlmayr’s breakthrough – A wedge resection
After Cunningham’s osteotomy publication, a series of German papers sustained the notion that outpatient surgery could be beneficial to orthodontic patients. Ironically, the original presentations of rudimentary SFOT at the turn of the 20th century languished in dusty journals and were not widely discussed in America for over half a century. However, the concepts blossomed in Europe.
Then, just before World War II, Bichlmayr (1931) described a very practical surgical procedure for patients older than 16 years to accelerate tooth movement and reduce relapse of maxillary protrusion. This was employed with canine retraction and first bicuspid extraction, by “excoriating” cortical plates of the palatal and crestal alveolus, and cortices of the extraction sites. Later, Neumann (1955), who divided the inter-radicular bone and ablated a wedge of bone palatal to the incisors meant to be retracted, would be most laudatory of Bichlmayr’s work. But this praise was to be proven faint.
Important to note is that Bichlmayr probably excised significant amounts of medullary bone with his procedure. He redefined orthognathic surgery by reclassifying it into two categories: “major” (total or segmental maxillary and mandibular correction) or “minor” (interdental osteotomy or corticotomy), and was the first to described the corticotomy procedure to close diastemata (Figure 1.3). Bichlmayr’s extensive wedge-shaped bone resection (Keilfoermige Resektion) was more extensive than the punctate and linear patterns presently employed. The latter seem more discrete and somewhat sophisticated, but the fundamentals of induced osteopenia and recalcification in retention are the same. If protracted decalcification is desired or if the degree of tooth movement is onerous (e.g., mass posterior bodily vectors), then Bichlmayr’s extensive decortication is appropriate.
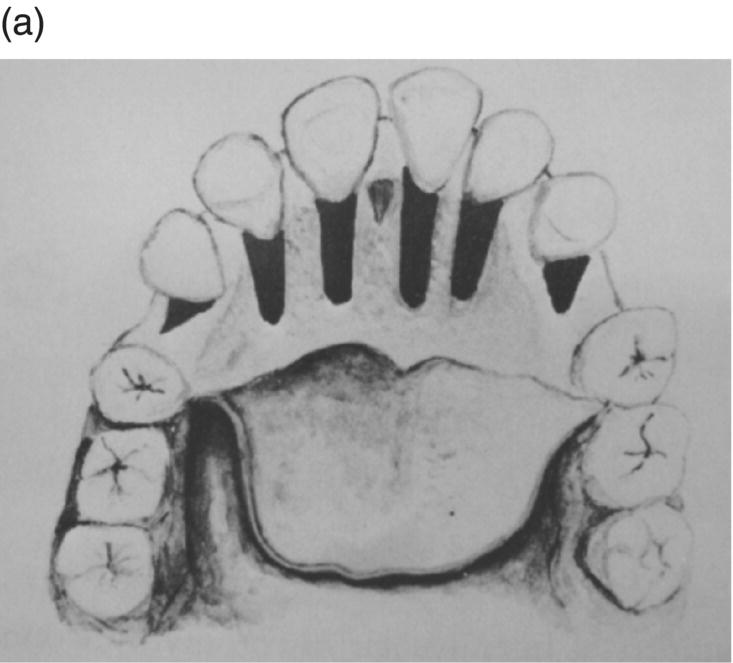

Figure 1.3 (a) Bichlmayr’s representation of palatal and distal decortication. Shaded wedge-shaped areas diagram a wedge-resection (Keilfoermige Resektion) of alveolar cortices and probably significant medullary bone. (b) Buccal areas subjected to posterior alveolus expansion. In view of more modern revelations about the physiology of SAD it seems that Bichlmayr’s aggressiveness, though done with clinical impunity, may have been somewhat superfluous. Considering the concern for buccal dehiscence and gingival recession associated with posterior dental arch expansion, a bone graft buccal to Bichlmayr’s posterior corticotomies (b) may be prudent for nongrowing patients.
However, in the context of movement alone, if a simple labial tipping of mandibular incisors is desired, then a more conservative procedure, even as minor as TMPs, may work where sufficient alveolar bone is present. However, this should not be done where there is a question of bony support. Bone paucity dictates that PAOO/AOO is clearly indicated. This is why Bichlmayr’s procedure is limited; not every oral site has the abundant bone of the maxillary palate. It is this wide spectrum of procedures that are presently defining the nascent clinical subspecialty of OTE.
The discerning principle of orthodontic-driven corticotomy procedures is this: the degree and duration of the necessary osteopenia is directly commensurate with the degree of induced surgical trauma, and proportional to the amount of bone density through which the teeth are moved; that is, a lot of denser bone means more decortication is needed for long tooth movement distance. It takes just as long for five 2 mm linear decortications to heal as it does two 5 mm linear decortications. Given that the comparative healing time is the same, where the sufficiency of SAD is in doubt there is little justification for timid decortication. Later, near mid-century, one can better appreciate Bichlmayr’s contribution to 20th-century orthodontics with the publication of Köle (1959), who derived his work from many previous German publications, but particularly that of Bichlmayr.
1959: Köle’s American debut
The seminal American work belongs to Köle because he wrote the first English-language paper describing a practical decortication of the alveolus bone to facilitate OTM. With some notable refinements, this is the basic technique that is employed today by those who promote the integration of orthodontic therapy and periodontal surgery. The Köle surgery was limited to the cortex of the dental alveolus, but subapical decortication was embellished by extending buccal and lingual cuts into the spongiosa until they communicated through the subapical medullary bone. Bucco-lingual communication is now considered unnecessarily morbid and eschewed by later SAD and PAOO/AOO protocols.
When Köle popularized corticotomy in the English literature he also promoted the so-called “bony block” hypothesis, an explanation later abandoned as the underlying physiology of SFOT became more clearly defined. He also reported buccal corticotomy in posterior inferior sectors to correct molar linguo-version and facilitate orthodontic expansion. Here, we see an emergence of physiology engineering theory as a conceptual replacement for the mechanical rearrangement models. He relied on the reduction of cortical resistance and tried to preserve the vascular supply from the trabecular bone to the teeth. Some years later this vascular issue was the focus of criticism by Bell and Levy (Verna and Melsen, 2012).
Special consideration should be made when studying this milestone contribution of Dr Köle in 1959. Where Bichlmayr indicated that he was essentially just making room for the roots by removing a physical impediment, Köle emphasized a subtle but key element. He left a thin layer of bone over the root surface in the direction of the intended tooth movement. This aspect of the root, the surface exposed to the resistance of tissue or bone, is called the root “enface” (Murphy et al., 1982). This is the area of microanatomy that we think travels with the root as a kind of “demineralized root–bone matrix transportation” tissue complex.
Köle’s methods were less ablative than Bichlmayr’s except for through-and-through osteotomies (cuts) made apical to the root tips of the teeth and next to the extraction sites. Köle’s observations led him to surmise that the roots of the teeth were not moving through the bone, but rather the bone was moving with the roots of the teeth. With his technique Köle claimed to be able to complete most major movements in adults in 6–12 weeks. To illustrate how far Köle’s concept has traveled, the modern incarnation of this idea can tip lower incisor teeth labially out of crowding in 4 days (Figure 1.4).
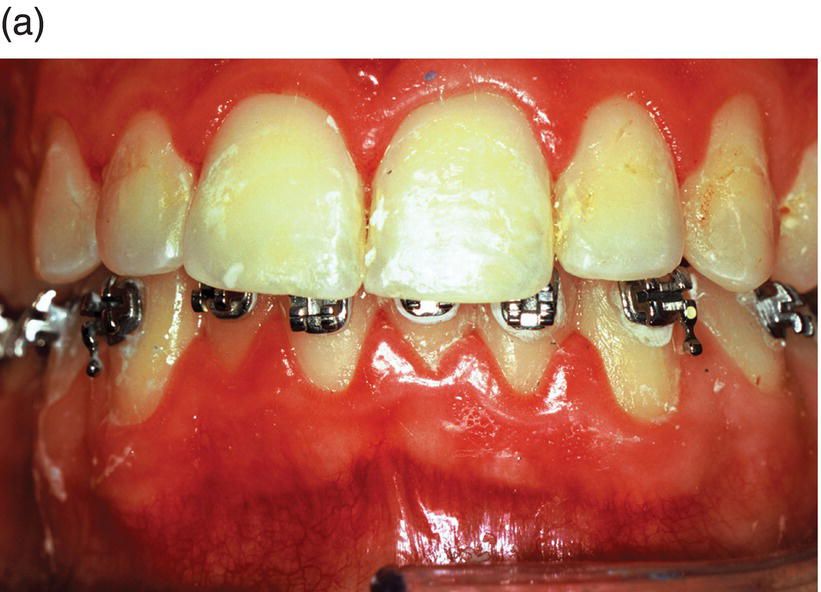

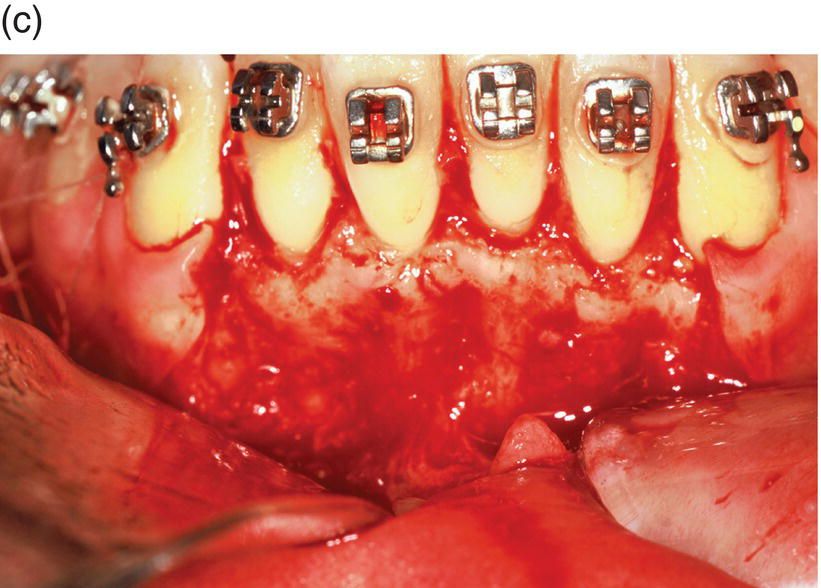
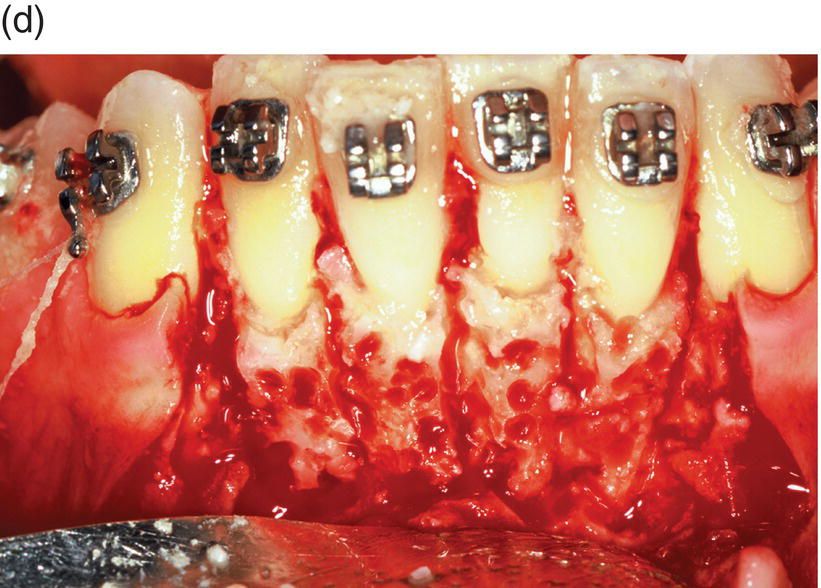



Figure 1.4 The contemporary method of SAD is represented in this 23-year-old Caucasian male college student. (a) His clinical appearance, where his orthodontic treatment relapsed after losing his retainer. He presented with a chief complaint of “crooked teeth.” Oral examination revealed an Angle’s class I occlusion with ostensible lower incisor arch length deficiency. This is a misinterpretation, because the so-called “crowding” is actually “pseudo-crowding” due to a return of the deep bite and the restriction of space for lower incisors as they approach the maxillary incisors’ cervical lingual surface. Note the relapsing dental deep bite, a musculo-skeletal phenomenon.
The patient needed treatment to be completed within a month. A full-thickness mucoperiosteal flap (c) was reflected and linear and punctate decortications (d) on the abundant labial cortex were combined with lingual TMP (trans-mucosal perforations) (e) to elicit a regional acceleratory phenomenon (RAP). A lingual hemi-circumferential fiberotomy (CSF) completed the surgical treatment. Minor interproximal enamel reduction was performed and a week later the patient presented with lower incisors well aligned (f). The treatment was maintained with a vacuum-formed plastic retainer (g). The patient reported that, “The teeth were straight in 4 days but I had to wait a week for an appointment.” Such rapid tooth movement is not uncommon when simple labial tipping is facilitated by interproximal enamel reduction (stripping) and a corticotomy.
This case illustrates how a panoply of SAD procedures (PAOO/AOO, TMP, CSF, etc.) can be employed according to each individual’s needs and desires. Corticotomies cannot be legitimately rendered without specific characterization of each patient’s needs and preferences, an individual imperative often lost among policy-level autocrats, doctrinaire ideologues, and corporate utilization review committees who are unduly enamored by Gaussian means.
Unfortunately, Köle’s interpretation of the mineralized medullary (spongiosa) bone moving with the roots of the teeth was incorrect. But in 1959 the correct scientific explanation for what was occurring subsequent to surgery did not yet exist. Unfortunately, this dissociation between Köle’s clinical perspective and scientific reality led to confusion and contradictory rationales for over three decades. As a result of this misconception, corticotomy-based surgeries evolved mostly into buccal and lingual cuts circumscribing the entire root with little regard for the facilitating physiology. Although Köle removed the buccal and lingual plates of bone at extraction sites, there was little evidence he fathomed the principle element in altering OTM. What is critical is this: bone volume must be reduced adjacent to the root surface at the root enface; that is, in the direction the tooth is moving. This was not emphasized for many decades, and thus stigmatized SFOT until this misconception was cleared up by the computerized tomography (CT) research by Professor Wilcko. Additionally, research at Loma Linda University began to bring into question the long-held notion of “bony block” movement (Anholm et al., 1986; Hoff, 1986; Tetz, 1986; Ryenarson, 1987; Gantes et al., 1990; Khng, 1993).
Compared with the more aggressive osteotomy protocols at the time, there was relatively little morbidity in Bichlmayr’s and Köle’s surgeries because luxation was not employed and the blood supply was not jeopardized. For those who subscribed to “mobilization by luxation,” their patients will generally suffer more, with little or no added value. Although it would certainly be preferable to have thicker layers of bone encasing the roots of the teeth in retention, this comes later when bone grafts (PAOO/AOO) were added to corticotomy protocols. Eventually, advances in the basic sciences would help to explain the lingering confusion and give more credence to the work of both Köle and Bichlmayr. But that would not occur until 1983 and did not reach most of the American dental profession until 2001.
1931–1965: moving parts or modulating physiology?
Kretz (1931), a contemporary of Bichlmayr, described a procedure similar to Cunningham’s, creating, in effect, a therapeutic fracture of the anterior alveolus. His aggressive manipulation of bone and preoccupation with the mechanical movement of “parts” continued the kind of “Newtonian bias” orthodontics as a pure mechanical art that still haunts SFOT today and eclipses any appreciation of how physiologic alterations may be modulated. The naiveté of the surgeons using these procedures belies the insights into wound-healing sciences. And this bias, to fracture bone and then rearrange it, is evident even in Reichenbach’s (1965) contribution over three decades later, which also expressed concern for iatrogenic periodontal damage.
Regarding this concern, one must certainly be adroit with a scalpel to avoid any ancillary periodontal damage. However, the benefits of SAD, PAOO/AOO, and TMP, for anyone who understands the pathogenesis of periodontitis, far outweigh any perceived risks. A number of cases over the last two decades have demonstrated that, aside from occult endodontic infection, periodontitis is not an absolute contraindication to SFOT. After flap reflection and SAD, a debrided lesion at the grafting site is no more unhealthy than that of a young child. In fact, the tissue surrounding such a debrided lesion is surfeit with a regenerative physiology and growth factors that actually facilitate phenotype changes and stem cell osteogenesis. Therefore, no resective periodontal surgery or initial therapy needs to be performed as a separate procedure before SFOT because the latter subsumes the former as long as the roots of the teeth are fully debrided and general principles of periodontal therapy are respected.
Although seemingly naive in periodontal science, Reichenbach was very wise in concern for alveolar blood supply, because the aggressive surgery described in the article certainly poses risks. In contrast, the very purpose of a refined SAD technique is to minimize that risk and maintain as much bone vitality as possible. This is done by limiting the surgical intervention to the cortex only; this enhances vascularity from the spongiosa. These simple caveats will ensure that Reichenbach’s concerns are honored. Unfortunately, without an empirical basis derived from controlled clinical studies, laboratory data, or conceptual sophistication (epigenetics) available, Reichenbach’s misapprehensions tend to be perpetuated.
1983: Frost and his regional acceleratory phenomenon
In the late 20th-century medical orthopedic literature a new concept was emerging that would ultimately be wed to the corticotomy rationale. Frost (1983) began to educate clinicians about two biological events seen with long bone fractures, which he called the systemic phenomenon and (what concerns us) the Regional Acceleratory Phenomena, RAP. This localized trauma-induced essentially a localized trauma-induced transient osteopenia was touted as an original insight and the definitive operational entity in bone fracture healing. The concept is largely attributed to Frost, despite the fact that Kolǎѓ et al. (1965) introduced many RAP effects as early as 1965.
Frost elaborated on the concept as an acceleration of the multiple stages of natural wound healing in the long bones. He explained that RAP begins within a couple of days of the fracture (osseous wounding), usually peaks at 1–2 months, and may take 6–24 months to subside. In SFOT, OTM and TMPs can perpetuate the osteopenic state beyond 2 months. RAP provides for a dramatic acceleration in bone turnover and, in earlier stages, an increase in the number of osteoclasts that produce a significant, but transient, osteopenia, a sort of benign osteoporosis. This is a condition similar to what would be observed in hyper-parathyroidism or a simple fracture, but in the case of selective decortication (SAD) no abnormal metabolism is involved and the effect is both transient and therapeutic.
Late modern perspectives (1959–2000): constructive controversy
1972: Bell and Levy
Bell and Levy (1972), in keeping with the Volkgeist of the times, published a more cynical interpretation of SFOT. Their iconoclastic approach to certain salient issues is the kind of controversy that vexes the neophyte surgeon and orthodontic students but ultimately, by intellectual conflict, results in synthesis and clarity in scientific thought. Theirs was one of many articles in about one decade that provide depth to the subject but also muddied the water by conflating simple corticotomies with osteotomy-like protocols.
This conflation obscured the important distinction between superficial cuts into the cortex of bone and deep cuts further into the spongiosa. Deep cuts indeed pose a greater risk of compromising blood supply according to animal studies, but luxated alveolar segments pose a more serious threat to the patient. In the later half of the 20th century it was unclear how deep the cuts needed to be in order to facilitate OTM and whether luxation (mobilization) was really necessary. Mobilization is a vague and variable term used as a synonym of luxation, the forcible loosening of the dentoalveolar unit by controlled fracture of the bone. The question mobilization begs is this: is mobilization necessary to facilitate tooth movement? As we will see, the answer is probably not.
The Bell and Levy work was the first experimental animal study of 4 Macaca mulatta monkeys, but they used the term corticotomy as a misnomer. They described a model of simultaneous mucoperiosteal flap reflection, and interdental corticotomies with mobilization of all “dento-osseous segments” which, they claimed, markedly compromised the blood supply to the anterior teeth. Specifically, they described “… immediate repositioning of one- and two-tooth dento-osseous segments.” They ablated excessive interradicular bone with a fissure bur, noting (emphasis added) that it should be done “…after the dental-osseous segments have been made freely movable with an osteotome” and warn that “Great care must be exercised to maintain a palatal soft tissue pedicle to the mobilized segments…”
Their histological study showed the risk of this type of procedure (full mucoperiosteal detachment plus deep cutting of medullar bone) to the vascularity of a dental pulp and surrounding medullar bone. They demonstrated distinct avascular zones that progressively recovered 3 weeks after surgery, except for the central incisor.
Referencing Köle, the authors reiterated that “…dentoalveolar segments can be readily moved bodily…” It is important to note that this “bony block” perspective is exactly the kind of misinterpretation that confuses sophisticated corticotomy with luxated osteotomies. The prejudice is noted further in the Bell and Levy article when the authors claim the rationale for “corticotomy” is vague and th/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


