. The condition is more common in individuals with a history of snoring, and has an association with obesity. Patients experience a repetitive obstruction of the upper airway during sleep, during which time arterial oxygen saturation usually (but does not always) fall. This may lead to sleep fragmentation and result in daytime sleepiness.
Diagnostic criteria require an apnoea/hypopnoea index of >5 events per hour of sleep. There is mounting evidence that significant OSA is associated with metabolic syndrome. Metabolic syndrome comprises hypertension and type 2 diabetes, with associated disturbances of lipid metabolism, and central obesity that predisposes to cardiovascular disease, including MI and stroke. Survival data demonstrates clear evidence that patients who are not compliant with treatment for OSA survive less long than those who are either compliant or those who do not have the condition. Sleep disruption causes excessive daytime sleepiness and patients may be a danger to themselves or others, especially when driving. Patients may present for ENT or maxillofacial surgery as part of the management of the condition, but the group at greatest risk comprises those who are unrecognized and therefore untreated, who present for surgery for an unrelated condition.
Screening questionnaires have been developed to help identify at-risk patients. The Epworth Sleepiness Scale (ESS) is the most popular and is used for assessing the level of daytime sleepiness that such patients experience and, whilst being rather unsophisticated, it has worldwide acceptance as a rough and ready guide to impaired daytime function. Other tools used to identify patients include the Karolinska, Berlin, and Pittsburgh sleep questionnaires. More recently, the ‘STOPBang’ questionnaire has been developed to screen patients at risk of OSA, and is proving to be useful in general practice.
Although simple clinical observation of the patient during sleep is often enough to make a diagnosis, investigations usually include overnight respiratory or full polysomnography, encompassing the multichannel monitoring of a number of parameters that assess breathing and physiological arousal from sleep.
Treatment includes submitting the patient either to continuous positive airway pressure, use of a mandibular advancement device, or to surgical osteotomy of the jaws (Fig. 5.1).
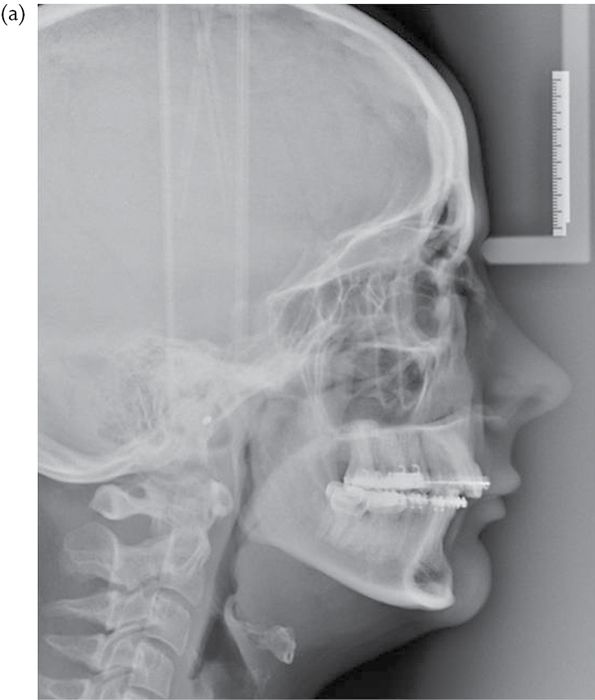

Fig. 5.1 (a) Pre- and (b) post-operative lateral cephalogram showing the change in the dimensions of the airway in a patient who has undergone bimaxillary surgery for sleep apnoea.
History
Medical history of particular relevance in orthognathic surgery
• Co-existing medical conditions may contribute to facial deformity, e.g. chronic juvenile arthritis (severe Class II) or acromegaly (Class III).
• Medical conditions that impact on suitability for treatment and the likelihood for developing complications.
• Oral contraceptive pill—should be discontinued 4 weeks before elective surgery.
Dental history
• Consider caries, periodontal disease, and TMJ disorders.
• Pattern of orthodontic extractions may be influenced by the prognosis of carious or restored teeth.
• Orthodontic and orthognathic surgery contraindicated in the presence of active or advanced periodontal disease.
• Pre-existing TMJ conditions may predispose to condylar resorption and relapse.
Growth and timing of treatment
• Surgical correction is usually deferred until growth has ceased. Most importantly in cases of asymmetry and Class III and open bite cases.
• Assess at what age the deformity first become apparent. Development of a class III malocclusion in adulthood may, for example, point to systemic disease such as acromegaly.
• Childhood TMJ trauma may result in abnormal growth.
• Developing an anterior open bite after the cessation of growth points to condylar resorption or sometimes periodontal disease.
• In asymmetric cases establish whether or not the condition is progressive, e.g. in unilateral condylar hyperplasia interventional surgery may be indicated at an early stage to reduce later secondary changes in the occlusal plane.
• Most asymmetries become apparent during the adolescent growth spurt.
• In general, treatment is deferred until a stable situation is reached, often best assessed with serial records.
Clinical examination
The patient is best assessed sitting upright in good light with the head in the natural head position and the Frankfort horizontal parallel to the floor. Patients, particularly those with asymmetric deformities, may present with an abnormal head position habitually developed for either functional reasons or to mask their deformity. It is important to compensate for such abnormal head posture if a true assessment is to be carried out.
Facial proportions
Profile view
See Fig. 5.2.

Fig. 5.2 Profile view of the face showing division into upper, middle, and lower thirds.
Maxilla
• Either normal, over-projected, or hypoplastic (suggested by para-nasal hollowing).
• Naso-labial angle 100 ± 10°—influenced by the degree of lip support derived from the upper incisors.
• Obtuse naso-labial angle associated with maxillary hypoplasia or upper incisor retroclination.
• Angulation of upper incisors to maxillary plane.
• Lip competency.
Mandible
• Can be normal, prognathic/progenic, and retrognathic/retrogenic. (Fig.5.3).
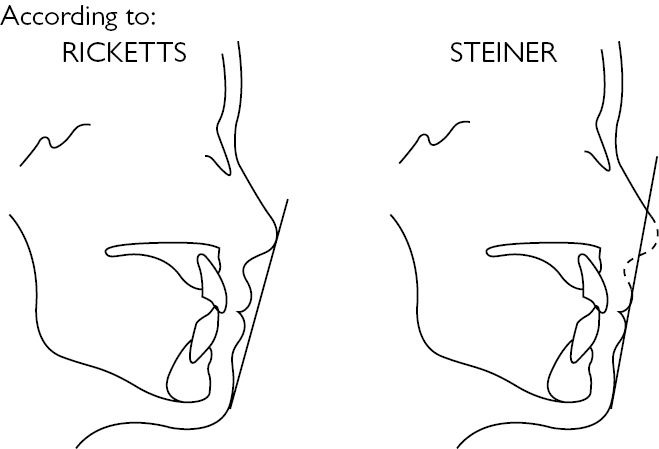
Fig. 5.3 Ricketts and Steiner’s lines. Allows an assessment of the antero-posterior relationships of the lips. Reproduced with permission from Henderson D. (1986). Colour Atlas and Textbook of Orthognathic Surgery. Book Medical Publisher Inc. with permission of Elsevier.
Vertical proportions
The normal face is divided into equal thirds (Fig. 5.4):
• Upper face: hairline to glabella.
• Mid-face: glabella to subnasale.
• Lower face: subnasale to soft tissue menton.
• The lower third of the face is further divided:
• upper third extending from subnasale to the upper lip stomion;
• lower two-thirds running from the lower lip stomion to the soft tissue menton.
• These vertical proportions are applied in both the frontal and profile views.
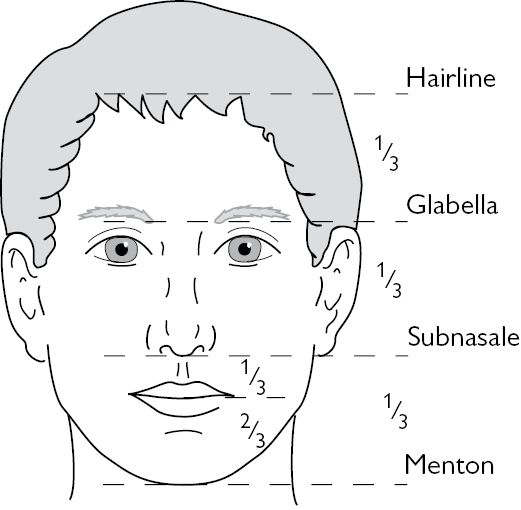
Fig. 5.4 Frontal view of the face showing division into thirds and further sub-division of lower third.
Vertical measurements
• Upper lip length.
• Alar base width = intercanthal distance = intercanine width.
• The inter-pupillary distance equals the width of the mouth.
Intra-oral examination
• Assess the general condition of the dentition and periodontal condition.
• Note the dental relationship, crowding, and spacing.
• Delineate the degree of dental compensation.
• Look for cross bites, and transverse arch discrepancies.
• Measure:
• overbite and overjet;
• upper incisor show at rest 2–3mm;
• upper incisor show when smiling;
• any occlusal cants;
• maxillary dental centre line position with relation to the facial midline;
• mandibular dental centre line position with relation to the facial midline;
• mandibular dental centre line position with relation to the central chin point.
• Check for displacements on closing, which may either mask or enhance the true degree of skeletal discrepancy.
Records
Photographs
Standard facial views include full face at rest and smiling, right and left lateral views, and three-quarter views. Include intra-oral views to show occlusion, frontal view of teeth in occlusion, right and left lateral views, and mirror shots of the upper and lower dental arches (Fig. 5.5).
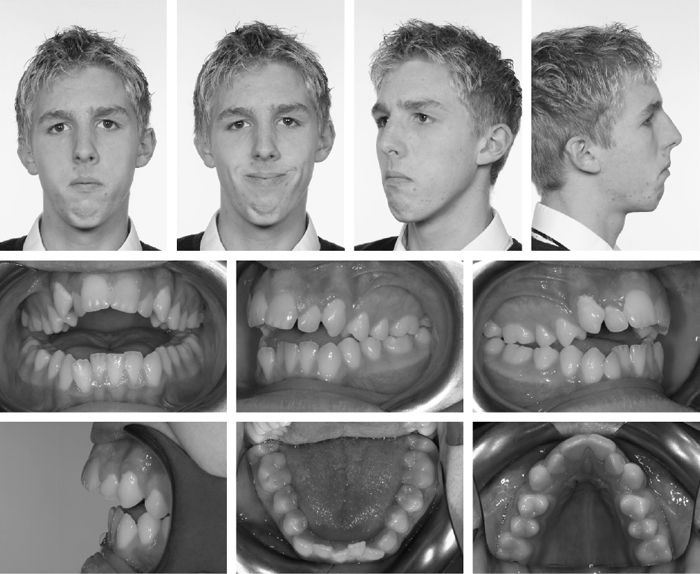
Fig. 5.5 Set of standard photographic views for orthognathic records.
Study models
Surgical planning for most procedures requires mounted models on some form of adjustable anatomical articulator.
Radiographs
• OPT: for pathology, wisdom teeth, etc.
• Lateral cephalogram for cephalometric analysis and treatment planning.
• Occlusal or peri-apical views as required.
• Postero-anterior (PA) cephalogram in cases of asymmetry.
• Special investigations.
Cephalometrics
• Cephalometric analysis (Fig. 5.6) forms the basis of orthognathic assessment and treatment planning, and underpins all current computer planning applications and profile prediction software.
• The lateral cephalogram:
• positioning with the Frankfort plane horizontal—essential that the patient does not posture the teeth into an abnormal position;
• avoid patient forward posturing the mandible—commonly seen in Class II patients.
• A multitude of different analyses are available and orthodontic texts should be consulted for more details.
• Most commonly used for orthognathic planning are those of the Eastman, Downs, and Rickets.
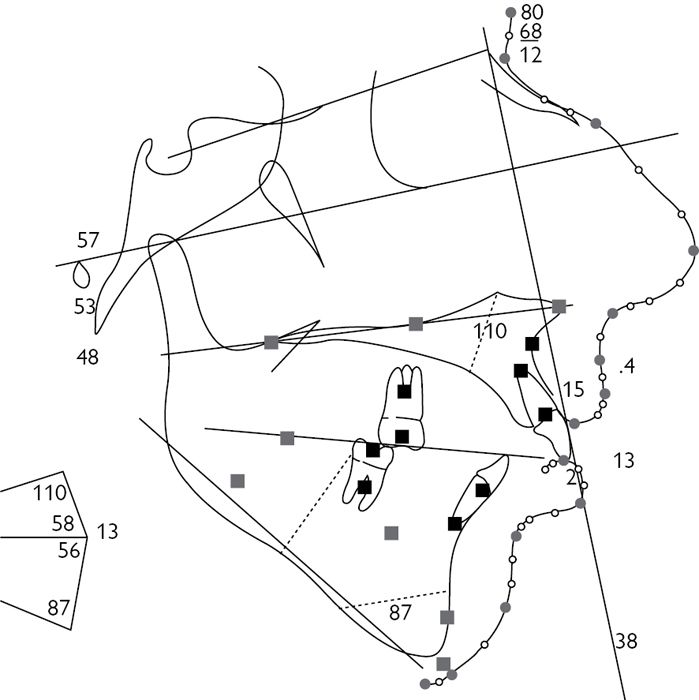
Fig. 5.6 Lateral cephalogram showing one of a number of available analyses.
Useful cephalometric relationships
• SNA is an indication of the relationship of the maxilla to the cranial base in the sagittal plane. Normal range 78–84°, mean 81°.
• SNB is an indication of the relationship of the mandible to the cranial base in the sagittal plane. Normal range 77–82°, mean 79°.
• ANB is an indication of the relationship of the mandible to the maxilla. Normal range 1–3° with A point anterior to B.
• SNPo is an indication of the relationship of the chin to the cranial base, independently of SNA/SNB.
• NPo is the facial plane and is an important reference plane for establishing facial convexity.
• Frankfort horizontal passes through both orbitale and porion. It has traditionally been used to define high- and low-angle cases relating the angle of the mandibular plane to the cranial base—the FM angle (high is >40°).
• SN–MP sella and nasion are reliable points subject to less plotting error than the Frankfurt horizontal hence SN–MP is a good index of the slope of the mandibular plane. Mean angle 32°.
Linear measurements
See Fig. 5.7.
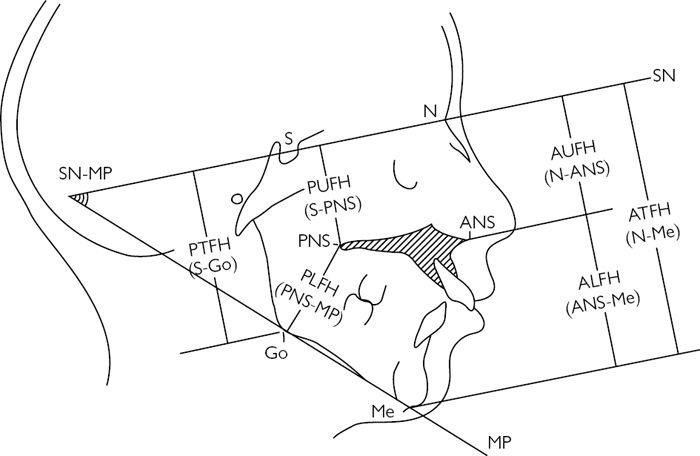
Fig. 5.7 Linear measurements. Traced lateral cephalogram showing anterior and posterior face heights, and the ratio of upper to lower face height. Reproduced with permission from Henderson D. (1986). Colour Atlas and Textbook of Orthognathic Surgery. Book Medical Publisher Inc. with permission of Elsevier.
Vertical proportions
ALFH is normally 55% of the total with AUFH being 45%.
Special investigations
In complex deformities, those with a significant asymmetry or a syndromic aetiology, CT scanning can be particularly useful. 3D-re-formatting allows a rapid appreciation of skeletal morphology.
Construction of accurate skeletal models facilitates both diagnosis and surgical planning. Bone scans may have a role to play in some cases (for example, condylar hyperplasia) to establish whether or not active growth is taking place.
Treatment planning
Checklist: essential clinical information for planning
• Class I/II/III occlusion.
• Skeletal base relationship.
• Maxilla AP—hypoplastic/normal.
• ?Vertical maxillary excess.
• Chin position normal/retrogenic/progeny.
• Upper incisor show at rest.
• Upper incisor show smiling.
• Centre lines—upper dental/lower dental/chin point.
• Overjet/overbite.
• Occlusal cant—yes/no?
• Naso-labial angle.
• Upper lip length.
• Alar base width.
Pattern recognition
Pattern recognition is important in orthognathic surgery. With experience one will learn to recognize a number of familiar presentations and these in turn suggest predictable treatment plans.
Common examples
• Class III patient with maxillary hypoplasia and mandibular prognathism with an average face height and no open bite—Tx: following pre-surgical orthodontic preparation, a maxillary advance and a mandibular set-back.
• Class III patient with a long face and high FM plane angle often with an open bite—Tx: following pre-surgical orthodontic preparation, maxillary impaction and advance with greater posterior impaction to correct open bite and mandibular set-back.
• Class II division 2 patient with retrogenia, a deep overbite, and a ↓ lower face—Tx: orthodontic conversion to a Class II division 1 malocclusion maintaining the curve of Spee and a subsequent mandibular advance to a three-point landing, which establishes a Class I occlusion and increases the lower anterior face height.
• Class II patients with a long face (vertical maxillary excess), retrogenia, and an anterior open bite—Tx: maxillary impaction (greater posterior than anterior) to close the open bite along with autorotation and advancement of the mandible.
• Class II patients with retrogenia and good maxillary position—Tx: simple mandibular advance.
• Severe class II patients with significant retrogenia and bird-face type deformity—Tx: depending on severity suggests mandibular advance with advancement genioplasty, inverted ‘L’ osteotomies or distraction osteogenesis.
Definitive surgical planning
Planning is essentially a clinical exercise and cannot be successfully achieved without the patient. A logical and systematic approach is essential and outlined is a scheme which can be universally applied to all cases. Whilst by no means exhaustive this scheme will give reliable results in the vast majority of patients and certainly be more than adequate for any exam situation.
Determine the position in which to place the upper incisor tip, defined in three dimensions (AP, vertical, and lateral)
• The vertical position of the incisor tip is defined by the degree of vertical maxillary excess and the upper incisor show at rest.
• Normal incisor show is 2–3mm.
• Advancement of the maxilla increases upper incisor show, any AP change in the maxilla must therefore be considered in relation to the desired vertical position of the incisor tip, i.e. a patient with normal incisor show of 3mm who requires a maxillary advance of 1cm will in addition require a degree of maxillary impaction in order to maintain the incisor show at current levels.
• The AP position of the incisor tip is determined by:
• AP position of the maxilla;
• naso-labial angle;
• degree of lip support;
• lateral relationship is determined by the upper dental centre line in relation to the facial mid-line. If correction of the maxillary dental centre line is required surgically one must consider whether to rotate the maxilla or move it bodily sideways. Introduction of a ‘yaw’ deformity may result in facial asymmetry or difficulties in positioning the mandible.
Next determine the position of the posterior maxilla
• AP movement and rotational movement of the posterior maxilla must equal the movement of the incisor tip (unless segmental surgery is being considered).
• Vertical movement of the maxilla, however, may differ between the anterior and posterior.
• In AOB cases a differential impaction with greater impaction of the maxilla posteriorly is often required.
• Differential posterior impaction may also be indicated to deliberately alter the maxillary occlusal plane.
• Lateral width discrepancies may be treated with:
• surgically-assisted rapid maxillary expansion (SARPE);
• maxillary midline widening;
• mandibular narrowing.
Finally determine mandibular movements
• Mandibular movements are those required to achieve a Class I relationship.
• Consider the lower dental centre line in relation to the upper dental centre line and facial midline.
• Note whether or not the lower dental centre line is coincident with the centre line of the chin. If they are coincident then aligning the dental centre lines will deliver the chin point to the facial midline. If they are not the chin point must be addressed separately.
Lastly look at the chin
• The chin position can be altered by genioplasty.
• Consider the movement required in three dimensions: AP, vertically, and laterally.
• The antero-posterior position of the chin can be influenced by the maxillary occlusal plane. In patients for whom advancing the mandible would be render them prognathic, one treatment strategy is to alter the maxillary occlusal plane. Posterior impaction of the maxilla forces clockwise rotation of the mandible and minimizes chin advancement.
Planning considerations in sleep apnoea
There are a number of decisions to be made specifically in relation to those patients with sleep apnoea. ![]() It is generally considered that to correct sleep apnoea it is necessary to advance the mandible by 1cm, although the literature to support this particular figure is somewhat lacking.
It is generally considered that to correct sleep apnoea it is necessary to advance the mandible by 1cm, although the literature to support this particular figure is somewhat lacking.
Sleep apnoea patients generally present at an older age than most orthognathic patients. They may or may not have any pre-existing malocclusion (indeed can have perfect class I occlusions) and often have no aesthetic concerns. There may be pressure to offer treatment as quickly as possible. Some of these patients may have limitations placed on their employment as a result of their sleep apnoea. This desire for expeditious treatment is at odds with a prolonged period of pre-surgical orthodontics. It is often wise in these patients to have had a trial of treatment with a mandibular advancement splint. If this is effective in managing their symptoms then it offers reassurance that surgical advance will be equally effective.
These patients must be assessed as would any other orthognathic patient. If per chance they are significantly retrognathic then mandibular advance may offer both resolution of their sleep apnoea as well as aesthetic improvement.
The fundamental decision in treatment planning is whether to go down a conventional orthognathic route with pre-surgical orthodontic preparation or simply to offer bimaxillary advance whilst maintaining their existing occlusion. If orthodontic preparation is undertaken the aim is to achieve an overjet which will allow either a 1cm advance of the mandible or an overjet which if combined with a small maxillary advance would facilitate the same. If patients are willing to combine orthodontics and surgery it is likely they may have a better aesthetic outcome. Accepting the existing occlusion and advancing both jaws may involve more of a compromise on the final facial aesthetics although this is often acceptable to this group of patients, particularly in view of the accelerated treatment.
Patients who have bimaxillary advance with the aim of maintaining their existing occlusion often adapt more slowly, perhaps because even the very smallest change in the occlusion is perceived to be different whereas if the occlusion is expected to change then adaptation appears quicker.
Hard to soft tissue relationships
Orthognathic surgery moves the bones of the facial skeleton, but the aesthetic result is determined by the soft tissue profile. An understanding of how the soft tissues move relative to the underlying bone is therefore of importance in the planning of surgery.
Nasal tip relative to A point
Moves in a ratio of approximately:
• 1:3 for osteotomies at the Le Fort I level.
• 1:2 for Le Fort II.
• 1:1 for Le Fort III.
Upper lip
• At the Le Fort I level the upper lip moves forward ~80% of the amount of maxillary advancement.
• When the maxilla is set-back the lip moves by ~50% of the skeletal move.
• For maxillary impaction the lip moves up between 10–40% of the bony impaction and lengthens by ~50% of any downward movement.
• The morphology of the lip will affect these predictions with a thick fleshy lip moving relatively less than a thin lip.
• A tight scarred lip as may occur in a cleft patient may move in a ratio of 1:1.
Lower lip
The movement of the lower lip is altered by many factors and does not follow the lower incisor teeth in any predictable pattern, although estimates of ~85% of the skeletal move in advancement and 60% with set-back are quoted.
Chin
Soft tissue pogonion moves consistently in a 1:1 fashion with either mandibular advance or set-back.
Adjuncts to planning
• The planning process can be refined by:
• cephalometric prediction tracing;
• photo-cephalometric planning;
• computerized programmes.
• Ensure that patients do not interpret these images as more than a prediction or imply any guarantee regarding the final outcome.
• Certain features are difficult to record accurately from the patient. One such example is a maxillary occlusal cant the true extent of which can be difficult to measure clinically. Planning using 3D reconstructions of CT data can offer significant benefits in these cases and facilitates accurate assessment of the true extent of any cant. Similarly, mid-line discrepancies can be accurately measured off the scan. This computer-assisted planning leads to greater fidelity in the planning of surgical moves, especially in complex cases.
• Computer-aided design/manufacturing (CAD/CAM) techniques allow the construction of skeletal models from CT data by procedures such as stereo-lithography or fused surface deposition. Such models greatly assist in the visualization of the true extent and location of abnormality and can be used to facilitate surgical planning.
• CAD/CAM technology now allows surgical wafers to be constructed directly from ‘virtual’ surgical plans. These modern techniques potentially eliminate the need for model-surgery.
Pre-surgical orthodontics
Orthodontic treatment carried out prior to jaw surgery to facilitate a correct jaw position, usually achieved with fixed appliances, which allow precise positioning of teeth in all dimensions. Orthognathic surgery patients should be assessed in multidisciplinary joint clinics.
The joint clinic
• Successful surgical correction of jaw discrepancy involves a close working relationship between surgeon and orthodontist.
• Patients should be assessed in joint clinics where an individualized treatment plan must be agreed with clear aesthetic and functional goals.
• Radiographs, plaster models and photographs must be available, including an appropriate tracing of lateral skull radiograph. Records are increasingly likely to be in digital format simplifying access and storage. The development of 3D imaging and CBCT is further advancing treatment planning.
• Develop a problem list matched to patient concerns and expectations.
• Consider ethnic facial morphology.
• Explain and record the risks vs benefits of treatment, and possible alternatives.
Pre-surgical preparation (12–18 months)
High-quality pre-surgical orthodontics is essential to obtaining good results from combined orthodontic/surgical treatment. Pre-surgical orthodontics should enable the desired skeletal and soft tissue changes to be achieved by the planned surgical procedures.
The aim of pre-surgical orthodontics is to eliminate any existing dental compensation and, hence, reveal the true jaw discrepancy in all three dimensions. Dental movements aim to align and upright teeth with respect to each arch using a period of fixed appliance therapy that permits full 3D control. If possible tooth movements are planned in the opposite direction to surgical movements to allow for post-surgical change, for example, it is prudent that any pre-surgical orthodontic preparation increases rather than decreases any open bite present at the beginning of treatment. In this way any orthodontic relapse will be in a beneficial rather than detrimental direction.
Pre-surgical orthodontics goals
• Relieve crowding.
• Level and align arches.
• Decompensate.
• Allow stable arch co-ordination.
• Achieve root divergence at the site of any segmental osteotomy.
Relieve crowding
• Crowding relieved by extractions, expansion, interproximal reduction, or a combination of approaches to achieve the pre-surgical objectives.
• Detailed analysis of space needed and discrepancies between tooth size and arch length carried out by the orthodontist.
Arch alignment
• Relief of crowding.
• Correction of rotations and occlusal interferences.
• Arch expansion or extractions.
Levelling
• Commonly accompanies arch alignment in conventional orthodontics but is not always desirable in surgical cases.
• By not levelling the arch and maintaining the curve of Spee one can achieve an increase in lower anterior face height when the mandible is advanced to a so-called ‘three-point landing’ with occlusal contact at the incisors and molars (leaving lateral open bites, which are closed down post-operatively by over-eruption).
• This manoeuvre is commonly adopted in Class II division 2 malocclusions and those with a ↓ lower anterior face height.
Decompensation
• In patients with severe Class III discrepancies the lower incisors are often retroclined and upper incisors are typically proclined.
• These incisor positions camouflage the underlying Class III jaw discrepancy.
• The upper jaw may be narrow with inclined upper molars. Correcting tooth positions will influence both AP and transverse relationships.
• The effect of a planned surgical move on the incisor angulation must also be borne in mind when planning the degree of decompensation.
• A differential posterior impaction of the maxilla is commonly carried out in open bite cases to upright the upper incisors. When this move is planned it is desirable to leave the upper incisors proclined and achieve full decompensation surgically.
• When planning the degree of decompensation the amount of labial bone is a key consideration. This may limit the degree of decompensation that can be achieved without moving the roots out of the available bone.
• It must be pointed out to patients that decompensation often exaggerates the pre-existing deformity and, therefore, makes them look worse as the pre-surgical orthodontics progresses. This effect is generally more obvious in Class III patients with an increase in reverse overjet and apparently greater chin prominence.
• In Class II cases lower incisor proclination and upper incisor retroclination can be present providing camouflage to the underlying skeletal pattern.
• Transverse dimension:
• Transverse decompensation of inclined molars is common. The upper jaw may be narrow with buccal inclined upper molars and the lower arch with lingual inclined molars. Pre-adjusted orthodontic appliances and rectangular wires can upright these molars to express a much larger discrepancy in transverse dimension;
• Post-surgical change in tooth positions following surgical correction can influence both AP and transverse relationship;
• Consider if orthodontic appliances alone can achieve stable transverse correction—is surgical expansion (either by SARPE or segmental osteotomy) indicated if dental expansion risks periodontal health and stability?
At the end of pre-surgical preparation study models, radiographs, and photographs are used to agree the final surgical plan. It is important to consider:
• What will the incisor inclination be post-surgery?
• Are changes in occlusal plane likely?
• Is maxillary width sufficient to accept the post-operative position of the mandible?
• Is surgical overcorrection planned?
Prior to surgery the orthodontist must ensure that:
• The overjet allows appropriate AP movement of upper and or lower jaw to achieve the desired aesthetic as well as occlusal result.
• Incisors are in the planned position.
• Arches are co-ordinated to create compatible inter-canine widths with coincident centrelines.
• Arches are stabilized with large rectangular archwire (minimum 019 × 025-inch stainless steel) 4–6 weeks prior to surgery.
• Surgical hooks are attached to the archwire to aid surgical inter-maxillary fixation (IMF) and post-surgical elastic traction.
Post-surgical orthodontics
Immediate review with the surgeon following operative intervention is important to plan the post-surgical phase of treatment. Teeth move rapidly in the post-operative phase and intermaxillary elastics can be used to refine jaw position. Initially, light elastics can be used and the patient reviewed at weekly intervals. It is important to consider force and direction.
After 6 weeks post-surgical orthodontic detailing commences. Usually, heavy rectangular archwires are replaced with lighter settling wires and intermaxillary elastics to fine tune the occlusion.
Surgical management
Timing of surgery
• Orthognathic surgical treatment is usually carried out at any time after the cessation of growth (prevents unfavourable post-operative change taking place as a result of further jaw growth).
• Growth usually ceases at the age of 17 in girls and 18 in boys.
• If growth has ceased, or there are extenuating social or psychological circumstances, consideration may be given to earlier surgery.
• In cases of condylar hyperplasia or asymmetrical growth, early intervention may be considered to reduce secondary occlusal changes.
Pre-operative assessment
• Routine haematological investigations should include a full blood count.
• Some units will recommend grouping and saving blood in maxillary surgery.
• Other pre-operative tests are ordered only if specifically indicated on the basis of the patient’s medical history.
Peri-operative management
• Antibiotic prophylaxis.
• Steroids: various regimens exist.
• DVT prophylaxis.
• Some advocate anti-fibrinloytics, e.g. tranexamic acid.
• Minimize intra-operative blood loss (also aids operative field):
• use of LA;
• cutting diathermy;
• hypotensive anaesthesia (may help to reduce post-operative oedema).
Post-operative care
• The advent of miniplate fixation means that rigid IMF is not required post-operatively. Benefits patients in terms of airway management, early function, and comfort.
• Most surgeons, however, advocate some form IMF often in the form of light guiding elastics.
• Nursing in the immediate post-operative period should ideally be carried out in a high dependency unit where close monitoring of the patient is possible. Invasive monitoring is not generally required.
Maxillary procedures
Maxillary osteotomies are based on the Le Fort fracture lines. Unlike fractures, however, osteotomies terminate at the posterior maxillary wall and aim to separate the pterygoid plates from the posterior maxilla (fracture lines run across the plates, see Fig. 5.8).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


