(1)
Dept. of Oral and Maxillofacial Surgery/Oral Pathology of the VU University Medical Center/ACTA, Amsterdam, The Netherlands
4.1 Introduction
Almost all lesions and diseases that may affect the oral mucosa may also occur on the tongue. On the other hand, there are some diseases that exclusively or almost exclusively affect the tongue. In this chapter, the emphasis is on the latter group of diseases.
4.2 Amyloidosis
Definition
Amyloidosis refers to the precipitation of certain proteins in various tissues of the body.
Classification
-
Primary amyloidosis (AL type), in which the protein fibrils consist of monoclonal light chain immunoglobulins
-
Secondary amyloidosis (AA type), in which there is an underlying disease; the proteins are derived from the acute phase of apolipoprotein precursors
-
Hereditary amyloidosis
-
Amyloidosis in chronic hemodialysis patients due to precipitation of β-2-microglobulins in the carpal ligaments
Etiology
The cause of the protein precipitation is unknown.
Epidemiology
Rather rare disease, mainly affecting people above the age of 60 years.
Clinical Aspects
Amyloidosis may present in the mouth as the first manifestation of the disease, most commonly by a slowly enlarging tongue. This may lead to difficulties with speech and swallowing (Fig. 4.1). In the majority of cases of oral amyloidosis, the patient is suffering from multiple myelomas (Kahler’s disease).


Fig. 4.1
Macroglossia due to amyloid deposition. Notice also the impressions from the teeth (“crenated tongue”)
The diagnosis of amyloidosis is based on histopathologic findings of a biopsy.
Histopathologic Examination
On histopathologic examination, amyloid presents as a hyaline-like, amorphous material. This amorphous material stains positive in a Congo red stain that shows a yellowish-greenish birefringence when using polarized light (Fig. 4.2).
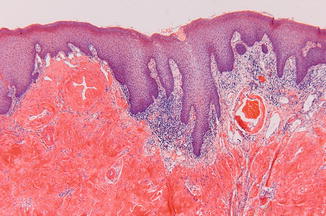
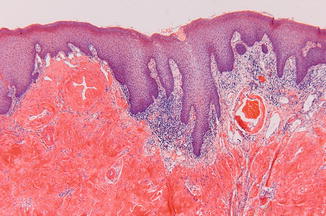
Fig. 4.2
Positive Congo red stain confirms the presence of amyloid deposition
Treatment
There is no effective treatment for primary amyloidosis. In secondary amyloidosis, the underlying disease should be treated, if feasible. In localized amyloid deposition, surgical excision may be considered.
4.3 Ankyloglossia (“Tongue Tie”)
Definition
Developmental disorder in which the frenulum of the tongue is shortened, thereby limiting the mobility of the tongue (Fig. 4.3).


Fig. 4.3
Ankyloglossia (“tongue tie”)
Epidemiology
Rather rare developmental phenomenon; there is no gender preference.
Clinical Aspects
Ankyloglossia rarely results in speech problems or eating problems.
Treatment
Surgical correction is rarely indicated and, if so, should in general not be performed before puberty. If performed, treatment consists of a Z-plasty; just cutting the frenulum is not effective and usually results in scar formation.
4.4 Atrophy of the Mucosa of the Dorsum of the Tongue
Definition
Atrophy of the epithelium of the lingual mucosa of the dorsal surface of the tongue.
Etiology
Atrophy of the lingual mucosa of the dorsal surface of the tongue is probably more or less an aging phenomenon and is rarely caused by an underlying disease, such as pernicious anemia.
Clinical Aspects
The dorsal surface of the tongue may show a rather smooth, depapillated aspect (Figs. 4.4 and 4.5). The color of the mucosa may vary from pale to fiery red. The patient may or may not complain of a burning sensation.

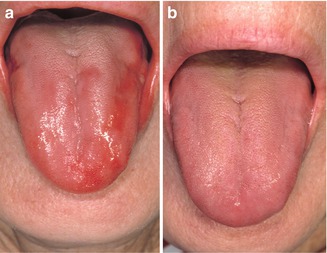

Fig. 4.4
Atrophy of the mucosal lining of the tongue. Notice also the presence of angular cheilitis in the corners of the mouth
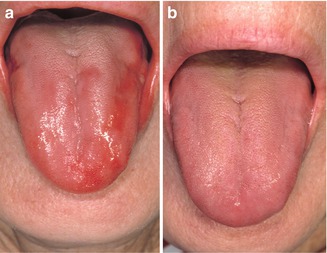
Fig. 4.5
Partly atrophic aspect of the lingual mucosa due to underlying pernicious anemia (a); normal aspect of the mucosa after vitamin B12 supplementation (b)
Treatment
In the absence of a treatable underlying disorder, there are no effective treatment modalities.
4.5 Ectomesenchymal Chondromyxoid Tumor
Definition
Rare, benign neoplasm that almost exclusively occurs on the dorsum of the tongue.
The exact origin of the neoplastic cells is unknown.
Clinical Aspects
Slow-growing swelling, usually on the anterior part of the dorsal surface, not characteristic otherwise (Fig. 4.6).


Fig. 4.6
Clinical nonspecific presentation of ectomesenchymal chondromyxoid tumor
Histopathology
Well-circumscribed neoplasm consisting of myxoid tissue in which monomorphic clear cells are dispersed (Fig. 4.7); these cells may mimic salivary gland cells but may also have a somewhat (rhabdomyo)sarcomatous appearance.
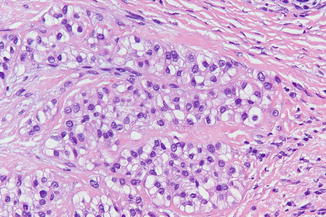
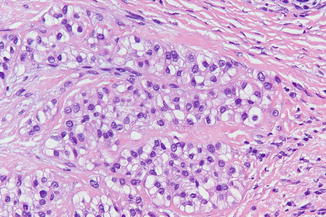
Fig. 4.7
Low-power view of ectomesenchymal chondromyxoid tumor
Treatment
Surgical excision; because of the rarity of reported cases, limited information of possible recurrences is available.
4.6 Fissured Tongue (Lingua Fissurata)
Definition
Presence of fissures in the dorsal surface of the tongue.
Etiology
Fissured tongue is to be regarded as a more or less anatomical variation and not as a disease.
Epidemiology
Common phenomenon; becomes usually not apparent before adulthood but may occasionally be encountered in children and adolescents.
Clinical Aspects
The pattern and the extent of the fissures may vary considerably (Fig. 4.8). Most patients are asymptomatic otherwise. May be associated with geographic tongue. Fissured tongue may be part of Melkersson-Rosenthal syndrome, the other features being granulomatous cheilitis and transient facial nerve paralysis; this triad is not necessarily present at the same time.


Fig. 4.8
Fissured tongue
Treatment
In case of symptoms, brushing the tongue twice a day may be helpful in some patients.
4.7 Geographic Tongue (Lingua Geographica; Migrating Glossitis)
Definition
Benign condition of the lingual mucosa characterized by migrating areas of smooth, reddish discolorations of the mucosal surface of the anterior tongue. The reddish areas are surrounded by a whitish border of desquamated epithelial cells.
Etiology
The etiology is unknown; stress has been mentioned as a possible predisposing factor. Due to the somewhat similar histopathologic aspects, a possible association with psoriasis has been suggested.
Epidemiology
The estimated prevalence is approximately 1 %. Geographic tongue may occur on all ages, even in young children.
Clinical Aspects
Smooth reddish changes on the dorsal surface of the tongue and sometimes also on the borders of the tongue, surrounded by a whitish slough (Figs. 4.9 and 4.10a, b). The reddish, depapillated areas will recover spontaneously in a matter of days, weeks, and sometimes months, showing up again at other sites of the tongue and, in rare instances, outside the tongue (“geographic stomatitis”, “ectopic geographc tongue”) (Fig. 4.11).



Fig. 4.9
Geographic tongue
Fig. 4.10
(a) Geographic tongue. (b) Same patient 1 month later; notice the different pattern

Fig. 4.11
Geographic stomatitis (“ectopic geographic tongue”) affecting the lower mucobuccal fold
Geographic tongue may cause symptoms of burning when using spicy food or drinking juices and may be associated with fissured tongue.
The diagnosis of geographic tongue is usually a clinical one, and there is rarely a need for a biopsy.
Histopathology
The histopathologic appearance is characterized by numerous polymorphonuclear leukocytes that migrate through the epithelium, giving rise to the formation of spongiform pustules or small abscesses, called Munro abscesses, in the upper epithelial layers (Fig. 4.12). The stratum spinosum may be thickened and edematous. In the smooth, red areas, the papillae of the connective tissue may reach high up close to the surface, mimicking to some extent the histologic appearance of psoriasis.
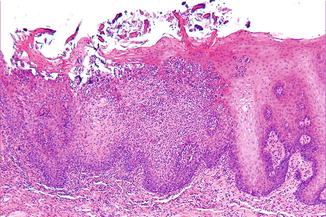
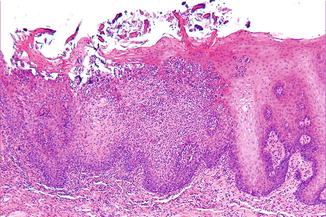
Fig. 4.12
Low-power view of geographic tongue
Treatment
There are no means to treat geographic tongue effectively. The condition probably persists lifelong, although there may be remissions for a long period of time.
4.8 Glossodynia and Burning Mouth Syndrome
Definition
Bilateral painful or burning sensation of the tongue and/or other oral mucosas in the absence of clinically visible lesions. Dry mouth (xerostomia) and taste disturbances may be accompanying symptoms. When only the tongue is involved, without other symptoms, the term glossodynia or glossopyrosis may be used. In case of other involved subsites, the term burning mouth syndrome (BMS) is used.
In case of a burning sensation of only the palatal mucosa in a denture wearer, without clinically visible abnormalities, the term denture sore mouth (DSM) is used, not to be mixed up with denture stomatitis in which there is a fiery red appearance of the palatal mucosa.
Etiology
The etiology of BMS is unknown. Although a variety of causes have been mentioned in the literature, the most common one being an underlying psychiatric disorder, there is no proven causative etiological factor. Burning mouth is rarely, if ever, based on hormonal disturbances, vitamin deficiencies, or side effects of medication.
Epidemiology
The estimated prevalence is less than 0.01 %. BMS rarely occurs below the age of 40 years and is much more common among women than men.
Clinical Aspects
Normal aspect of the mucosa (Fig. 4.13). In patients complaining of dry mouth, there may be a sufficient amount of saliva as being observed during oral examination. However, xerostomia refers to the subjective feeling of dryness as experienced by the patient, while hyposalivation refers to an objectively measured decrease of the salivary flow.


Fig. 4.13
Normal aspect of the tongue in patient with glossodynia
Laboratory Studies
Laboratory studies of whatever type (e.g., vitamin levels, iron, etc.) rarely if ever contribute to the management of the symptoms. Nevertheless, such studies can be performed in case of unusual BMS, e.g., occurring in patients below the age of 30 years (Table 4.1).
Table 4.1
Management of patients with symptoms of burning mouth syndrome
Management
Always perform a thorough examination of the mouth, even when the symptoms are highly suggestive of BMS. Occasionally, the burning sensation is caused by mucosal lesions or disorders such as erosive lichen planus or erythroplakia.
Take time for the patient to explain the complexity of this syndrome and avoid giving the patient the impression of suffering from a psychiatric disorder, since there is no evidence for such suggestion. Reassure the patient that the symptoms are not caused by an underlying systemic disease, including malignancy.
In the majority of patients, the burning sensation will disappear in a matter of years. Some patients may need professional support to learn to cope with these symptoms. In severe cases, the prescription of antidepressive drugs may be indicated. This such suggestion is usually declined by the patient.
Do not perform any dental or surgical procedures that are not truly indicated. Do not refer the patient unless you know a qualified colleague who is more knowledgeable in this particular subject.
4.9 Granular Cell Tumor
Definition
Benign neoplasm probably derived from Schwann cells or from neuroendocrine cells.
Etiology
Unknown.
Epidemiology
Rare tumor that may occur already in children, more often in females than in males.
Clinical Aspects
A granular cell tumor may occur everywhere in the body but most often affects the tongue.
It is usually a solitary tumor but multiple tumors may occur as well. The clinical presentation is that of a yellowish nodule of the tongue or, occasionally, of other oral sites, being asymptomatic otherwise (Fig. 4.14a, b). In an exceptional case, simultaneous granular cell tumors may occur elsewhere in the body, e.g., in the lungs.
Fig. 4.14
(a) Rather characteristic aspect of a granular cell tumor. (b) Multiple granular cell tumors in a child
Histopathology
Somewhat circumscribed but not encapsulated tumor consisting of large polygonal cells with a granular cytoplasm. The granular cells are positive for S-100 immunohistochemically. In the overlying epithelium, pseudoepitheliomatous hyperplasia may be encountered; this phenomenon may be mistaken for a squamous cell carcinoma (Fig. 4.15a, b).
Fig. 4.15
(a) Pseudoepitheliomatous hyperplasia overlying a granular cell tumor. (b) Low-power view of granular cell tumor
Treatment
Local excision usually suffices, although no true radicality may be obtained at the histopathologic level. Nevertheless, recurrences are rare.
4.10 Hairy Leukoplakia
Definition
Benign whitish change of the mucosa of the borders of the tongue in immunocompromised patients.
Note: The term “leukoplakia” for this condition is unfortunate since leukoplakia refers to a white lesion that cannot be identified as any other known white lesion. Hairy leukoplakia is a well-defined “known” lesion. Furthermore, “true” leukoplakia is premalignant, while hairy leukoplakia is not. In addition, the use of “hairy” may cause confusion with regard to hairy tongue and even with regard to the term hairy cell leukemia. Besides, the clinical aspect is not always “hairy.”
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


