Case History and Clinical Examination
Sven Poulsen, Hans Gjørup, and Dorte Haubek
The purpose of the present chapter is to describe the case history and the clinical examination of children and adolescents receiving pediatric oral health care. The chapter will not deal with details concerning signs and symptoms of specific conditions, such as caries and periodontal disease; these will be dealt with in subsequent chapters of this book. This chapter will merely describe the systematic approach necessary to collect data to arrive at a correct diagnosis for the individual patient.
A thorough case history and clinical examination is just as important for decisions on prescribing, for example, radiographic and laboratory examination and arriving at a proper diagnosis and an appropriate treatment plan in the pediatric dental patient as in the adult (Box 7.1). Figure 7.1 shows a flowchart illustrating the full procedure of anamnesis, clinical examination and suggestions for additional tests and information.
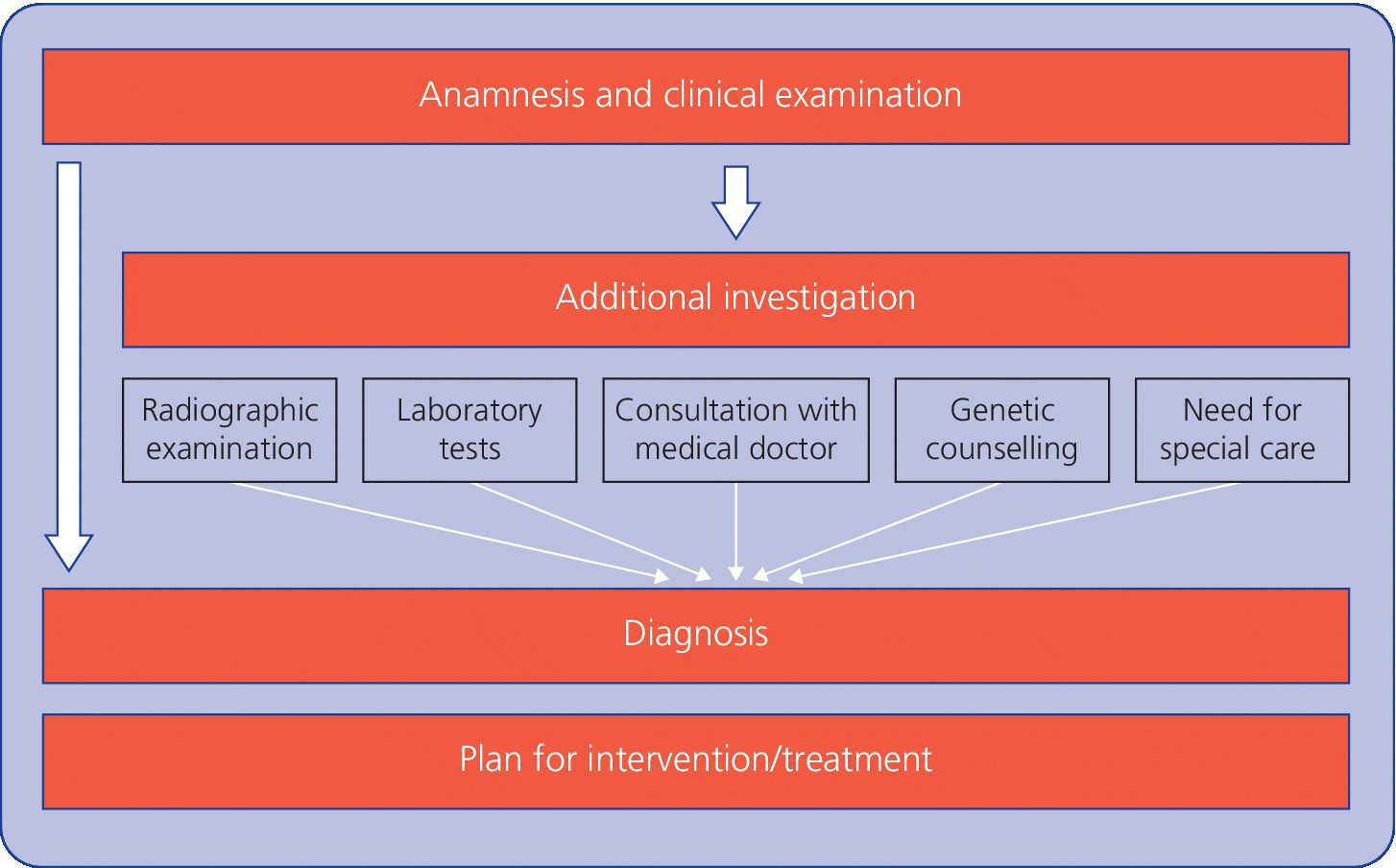
Figure 7.1 Flowchart illustrating the full procedure of anamnesis, clinical examination, and suggestions for additional tests and information.
Since child dental services in the Nordic countries cover the entire child population, the dentist is in many areas one of the health professional who sees the child most often; dentists should be aware of signs and symptoms of the most common acute and chronic conditions and diseases in childhood and adolescence in order to make appropriate referrals to other health professionals.
Furthermore, the case history and the clinical examination are often the initial and very important contact of a young child and its parents with the dental team and the clinical setting.
A thorough case history and clinical examination is not only mandatory at the child’s first visit to the dentist, but just as important at the start of later recalls and new treatment periods. Thus, it is important to remember to update the anamnesis at recall visits.
Case history
In contrast to taking the case history in an adult patient, the case history in children and especially in young children has to be taken through another person, often one of the parents. This has two important implications.
The information obtained from the accompanying person may not necessarily be a valid reflection of the situation of the child. Most often it is, but the dentist should keep in mind that the adult is talking on behalf of the child when evaluating pain, for example. In the case of traumatic injuries, the pediatric dentist should be especially aware of atypical lesions that do not seem to correspond with the information obtained in the history in order to identify, for example, cases of child abuse (see Chapter 26).
Telling the child that the dentist is going to talk to the accompanying person for a short while, before looking at the child’s teeth can avoid the child feeling overlooked.
It is important that the examination of the child is performed in a relaxed atmosphere. The dental team should be fully aware of meeting the child with child competence, i.e., using their knowledge, experience and skills in the interplay, management and treatment of the child. Both the child and the parents should be met with a respectful, warm and supportive attitude altogether aiming at the creation of a positive and reassuring atmosphere of the dental setting. It is important to focus on the child and parents as people and not primarily as patients. This also gives the dentist a good opportunity to form an impression of the general background of child and parents, their attitudes to dentistry, and their expectations.
The case history should start by obtaining the personal data of child and parents (name, age, etc.) and a description of the present complaint(s), if any, of the child, as well as the reason for the consultation.
At this point, it may be advantageous if the dentist takes a quick look at the child’s mouth and teeth. In practice, the case history should take the form of a comfortable conversation rather than an enquiry. Standardized forms to be filled in by the parents can be used to obtain part of the case history, but their use should always be followed by an interview.
The complete case history consists of a family history, a general medical history, and a dental history. Important information to be collected under each of these headings is shown in Box 7.2.
The family history
The purpose of the family history is to provide relevant information about the social background of the child and, most important, the family.
Such factors as the parents’ occupations, the number of children in the family, and the child’s attendance at day‐care institutions and schools, are important in selecting a realistic plan for preventive and restorative dental care.
The family history should also include the occurrence of inherited diseases, oral or general. It should be emphasized that the information required for an adequate family history is considered confidential by many parents. Thus, the dentist`s questions should be restricted to issues and diseases of relevance in the clinical situation. Some parts of such information may be considered confidential, and national guidelines on informed consent for transferal of information between health professionals should be observed.
General medical history
The general medical history should place the oral problems into a broader perspective of total patient care.
Congenital or acquired diseases or functional disturbances may, directly or indirectly, cause or predispose to oral problems (e.g., craniofacial syndromes, juvenile rheumatoid arthritis, diabetes, hematologic diseases; see Chapters 23, 24 and 25) or they may have effects on the delivery of care and treatment of oral disease in the individual child.
The general medical history includes information about pregnancy, delivery, the neonatal period, and early childhood. It should review hospitalizations, illnesses, traumatic injuries, and previous and current medical treatment. Information about infectious diseases (e.g., childhood diseases, otitis media), immunizations, allergies (including adverse reaction to drugs), and sleeping disturbances should be obtained.
As recent research has shown that lack of cooperation and behavior management problems during dental treatment may be due to specific child personality characteristics or to e.g. neuropsychiatric disorders, information on these child characteristics are important (see Chapters 6 and 24).
Finally, current and past problems as well as any current signs and symptoms of disease in the head, respiratory, cardiovascular, gastrointestinal, neuromuscular, and skeletal systems should be included in the general medical history. When necessary this information should be supplemented with information from hospital records and the family physician.
Dental history
At this point, the child`s opinion on their own teeth is reviewed. The dentist asks if the child feel any pain in the teeth or jaws, any functional limitations (chewing, biting, swallowing, talking, etc.), and if the temporomandibular joint is affected by pain, soreness, crepitation or clicking. Furthermore, the child is asked if it feels embarrassed by the appearance of his or her teeth and face. Finally, any subjective suspicion of diseases in the soft and hard oral tissues should be revealed.
The child’s past experience with dental services should be reviewed as well as the present dental problem(s). The kind of dental treatment received previously, including pain control measures and acceptance of earlier dental treatment, gives the dentist important background for the evaluation of the child’s past behavior in the dental situation and may reveal treatment procedures which have been especially demanding for the child. Factors of importance for the future oral health should be identified as part of the dental history, including day‐to‐day oral hygiene, dietary habits, and sucking habits. The history also aims at identifying etiologic explanations for such unusual conditions as early childhood caries, rampant caries, erosion, atypical tooth surface loss, gingival recession, and periodontitis noted during the initial, brief inspection.
In addition, a survey of the previous dental records and radiographs, if available, may give important information on the child`s dental history.
Clinical examination
General appearance
As mentioned earlier, the pediatric dentist is, in many cases, the medical professionals who see the child most frequently. Thus, the dentist has the opportunity to identify medical and functional problems that may have gone unnoticed and can contribute to an improved health service by making appropriate referrals.
Assessment of general appearance should start before the child is seated in the dental chair. To meet the child in the waiting room and walk together with it to the operatory gives the dentist an excellent opportunity to form a first impression of the child’s stature, body proportions, general posture, head posture, gait, and physical capability. This assessment may indicate growth disturbances, central nervous system disorders, neuromuscular disorders, or orthopedic problems worthy of further examination.
Examination of the skin for color, pigmented lesions, bullae, scarring, dryness, and scaling may indicate the presence of systemic disease. The hands should be examined with emphasis on e.g. webbing of fingers (indicative of a syndrome), and evidence of habits. The quality and the shape of the nails should be assessed. In ectodermal disorders the nails may be missing or be of poor quality. In chronic respiratory diseases or congenital heart disease, the fingernails may be markedly convex and the fingers clubbed.
Extraoral examination
The dentist should always note obvious deviations in the child’s face and head posture. If obvious deviations are noted, a systematic examination of the head and neck should be performed. The face is examined both en face and in profile. En face the facial symmetry is assessed, and asymmetries described as deviations of midline‐points in relation to the overall facial midline (e.g., deviation of the nose tip, the philtrum, the symphyseal midline, or the dental midlines). The facial height and proportions are assessed in both aspects (Figure 7.2). In the lateral aspect, the overall facial profile is assessed (as straight, concave or convex), and the degree of mandibular prognathism is characterized as normal, retrognathic, or prognathic. Finally, the presence of a mid‐face deficiencies or a prominent nose might be noticed. The extraoral examination includes the assessment of each anatomical structure for the integrity, function, development, and pathology. Minor anomalies should also be assessed since such anomalies are present in many multiple congenital anomalous syndromes and since it newborns with several minor anomalies, frequently also have major anomaly. Many anomalies and developmental problems are not identified until late in the childhood. Thus, the dentist should in all cases be aware of deviations from normal traits and mind the possibility of an undiagnosed general disease or developmental problem.
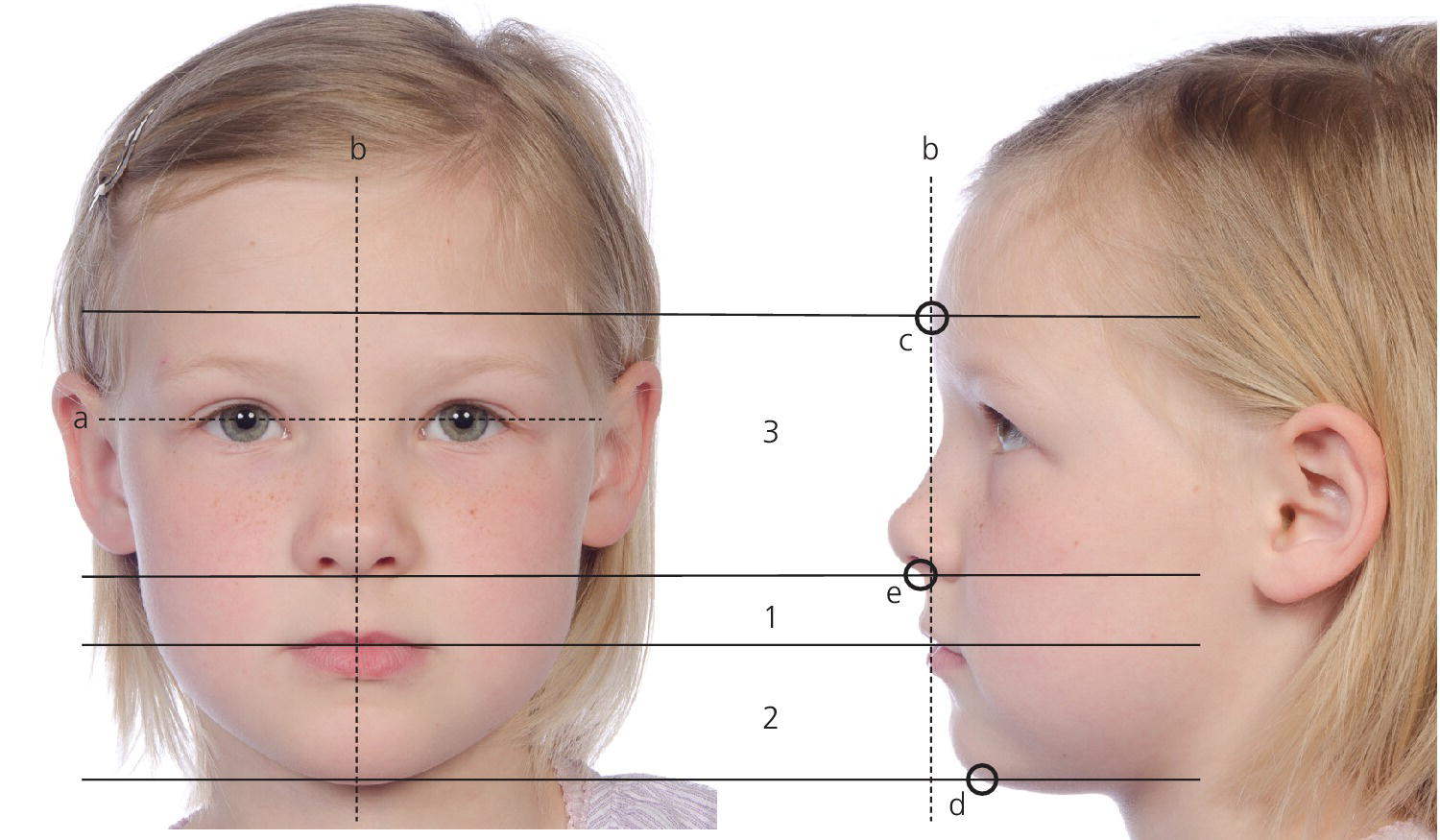
Figure 7.2 Assessment of the facial symmetry and proportions. The interpupillar line (a) defines the horizontal reference line. A perpendicular line (b) through the midpoint of the interpupillar line defines the midfacial line. The prominence of the forehead (glabella) (c) and the lower point of the chin (menton) (d) defines the total face height, which is divided into the upper face height and the lower face height, by a line plane tangent to the lower border of the nose (subnasal point) (e). The lower face height is divided into the upper lip and the lower lip by the horizontal contact line between the lips (stomion). Harmonious facial proportions are characterized by the upper face height equalizing the lower face height, and the height of the lower lip is double the height of the upper lip. Ideally, the midpoints of the nose, the lips, and the chin are on the midfacial line.
The examination of the face should also include an assessment of the length of the upper lip, the morphology of the lower lip, including the supramental groove, and the activity of the mentalis muscle. Lip closure and the tonus of the muscles in lips and cheeks are often insufficient in disabled children and may result in drooling.
The color, amount, and quality of the hair should be assessed. In certain types of ectodermal dysplasia and various metabolic diseases the hair is missing or sparse and thin (Figure 7.3).

Figure 7.3 Sparse eyebrows in a 12‐year‐old boy with ectodermal dysplasia.
Intraoral examination
For the young child, the intraoral examination may be the first experience of intraoral manipulations and the first contact with dental instruments. For this reason the dentist should use simple intraoral examination procedures to accustom the child to manipulations with mirrors, probes, and other instruments in the oral cavity. A “tell–show–do” technique (as described in Chapter 6) should be employed to its full extent. During and after the intraoral examination, the dentist should take the opportunity to show parents what has been found. Most parents welcome explanations and discussions on their children’s dental conditions.
The oral cavity should be examined in a systematic way in order to avoid omission of important conditions. The equipment needed for routine intraoral examination can be limited to a few instruments. The examination can almost always be performed with the child in the dental chair. In some cases, for example very small children, it may be an advantage to perform the examination with the child seated in the parent’s lap, similar to the position used when examining young children with traumatic injuries (see Figure 18.11).
Examination of the oral mucosa
The soft oral tissues are examined before the hard dental tissues. This part of the examination should also include an assessment of the tonsils (size and inflammation) (Figure 7.4). Metallic objects should be removed before the clinical examination (Figure 7.5).
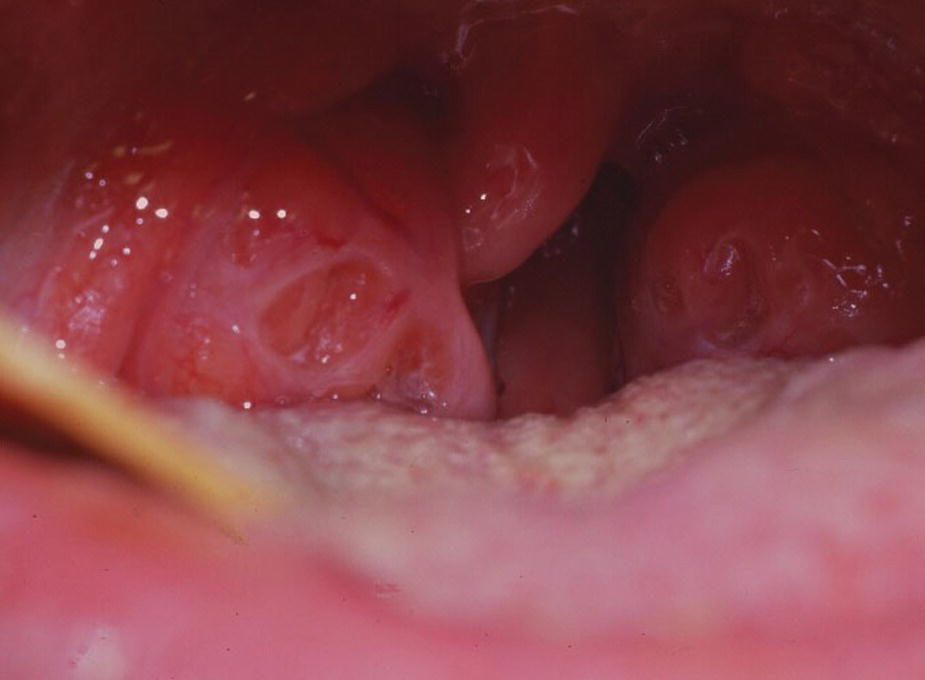
Figure 7.4 Inflamed tonsils in 13‐year‐old girl.

Figure 7.5 Piercing has become a part of teenage culture. Insertion of metallic objects in the tongue increases the risk of damage to the soft oral as well as the hard dental tissues. Such objects should be removed before the clinical examination of the oral mucosa.
The oral mucosa should be examined—being wiped off if necessary—starting with the inside of the lips and continuing to the mucosa on the inside of the cheeks, including the upper and lower alveolar sulci. The palate is inspected using a mirror. The mucosa of the tongue and the floor of the mouth are examined after careful retraction of the tongue.
During examination of the oral mucosa, which may include palpation and inspection, ulcerations, changes in color of surface, swellings, or fistulae are noted. When examining alveolar processes special attention should be given to any minor swellings or retraction of the gingival margin, which could be a sign of periapical or interradicular pathologic processes and, especially in older children and adolescents, a sign of marginal periodontal disease (see Chapter 14). Such findings will often indicate the need for radiographic examination (Figure 7.6).



Figure 7.6 Fistulae and abscesses due to caries in the primary dentition can vary from (a) a small sinus on the buccal mucosa, which can easily be missed during the clinical examination to (b) small abscesses, and (c) large swellings. Radiographic examination may be indicated.
The presence and attachment of frenulae should be examined with special emphasis on the possible complicating effects of high insertion of such frenulae on the periodontal tissues (see Chapter 15).
Examination of periodontal tissues
Periodontal tissues are examined for inflammatory changes. The gingival margin is gently checked with a blunt periodontal probe for edema, bleeding, and swelling.
A complete periodontal examination of all teeth for loss of attachment is hardly feasible on a routine basis. There is little reason to recommend periodontal probing in the primary dentition unless redness of the gingival margin, radiographic signs of bone loss or general medical conditions motivate this. In the permanent dentition, loss of attachment may be seen during the teenage years. Thus, if periodontitis is not suspected from radiographs, it seems reasonable to postpone systematic periodontal probing until 12 years of age.
Deposits on the teeth can be either hard or soft. Calculus is, however, not a common finding before the teens, although some cases of calculus in the primary dentition can be found on surfaces close to the orifices of the salivary gland ducts and occasionally on the proximal surfaces in the posterior region. The amount of deposits as well as the color should be noted.
Examination of teeth
The dental examination reveals:
- the developmental characteristics of the dentition
- any acquired injury or disease of the dentition.
The developmental characteristics include the number and types of erupted teeth, which has to be related to the chronologic age of the child. The normal development of the dentition from eruption of the first deciduous tooth, through a transient (mixed) dentition to a complete permanent dentition can be described using the dental stages described by Björk, Krebs, and Solow in 1964 [1] (Box 7.3). Asymmetry in the eruption of teeth (right versus left or upper versus lower jaw) may indicate impaction of teeth or other dental anomalies (Figure 7.7). At 6 years of age special attention to the first molar region is important in order to detect failure in eruption of the first molar. At 9–12 years of age special attention to the canine region of the upper jaw is important. If the contour of the canine crown is neither visible nor palpable buccally, an impaction of the canine has to be suspected. Thus, a radiographic examination is indicated. Deviations in the vertical position (infra‐ or supra‐position) of single teeth in relation to the occlusal plane are noted. Infraocclusion of deciduous teeth might indicate an eruption problem of the successor or other dental anomalies. Infra‐position of permanent teeth is an indication of a serious eruption problem.


Figure 7.7 Asymmetric eruption of incisors should always give rise to further examination. In the present case, (a) delayed eruption of 21 was due to (b) a mesiodens.

VIDEdental - Online dental courses


