Orthodontic Diagnosis
The Problem-Oriented Approach
Questionnaire/Interview
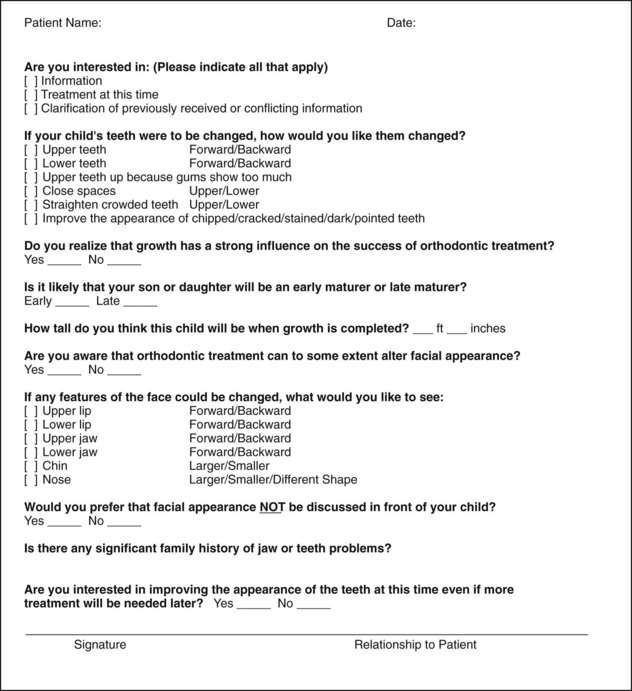
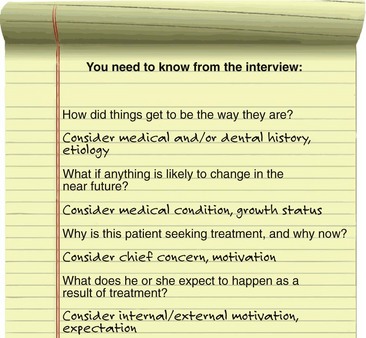
The goal of the interview process is to establish the patient’s chief concern (major reason for seeking consultation and treatment), and to obtain further information about three major areas: (1) medical and dental history, (2) physical growth status, and (3) motivation, expectations, and other social and behavioral factors. In orthodontic specialty practice, it can be quite helpful to send the patient an interview form to fill out before the first visit to the office. An example of a form focused on the chief concern, which could be sent to the patient in advance or used as an outline for the interview with the patient, is shown in Figure 6-1. Note its emphasis on learning the extent to which the parent or adult patient is concerned about facial appearance. A form to elicit the medical/dental history, which should be filled out in advance, would accompany it, but the medical history form becomes only an outline for discussion because so many parents and patients do not list things they think are of no concern to the orthodontist.
Chief Concern
As we have discussed in some detail in Chapter 1, there are three major reasons for patient concern about the alignment and occlusion of the teeth: impaired dentofacial appearance and a diminished sense of social well-being, impaired function, and impaired oral health. Although more than one of these reasons often may contribute to seeking orthodontic treatment, it is important to establish their relative importance to the patient. The dentist should not assume that appearance is the patient’s major concern just because the teeth appear unesthetic. Nor should the dentist focus on the functional implications of, for instance, a crossbite with a lateral shift without appreciating the patient’s concern about what seems to be a trivial space between the maxillary central incisors. For an individual with reasonably normal function and appearance and reasonable psychosocial adaptation, the major reason for seeking treatment may well be a desire to enhance appearance beyond the normal, thus potentially improving quality of life (QOL). The greater orientation of modern family practice toward cosmetic dentistry increases the chance that a patient may be referred to an orthodontist for comprehensive treatment simply to enhance dental and facial appearance.
Medical and Dental History
Orthodontic problems are almost always the culmination of a developmental process, not the result of pathology. As the discussion in Chapter 5 illustrates, often it is difficult to be certain of the etiology, but it is important to establish the cause of malocclusion if this can be done and at least rule out some of the possible causes. A careful medical and dental history is needed for orthodontic patients both to provide a proper background for understanding the patient’s overall situation and to evaluate specific concerns.
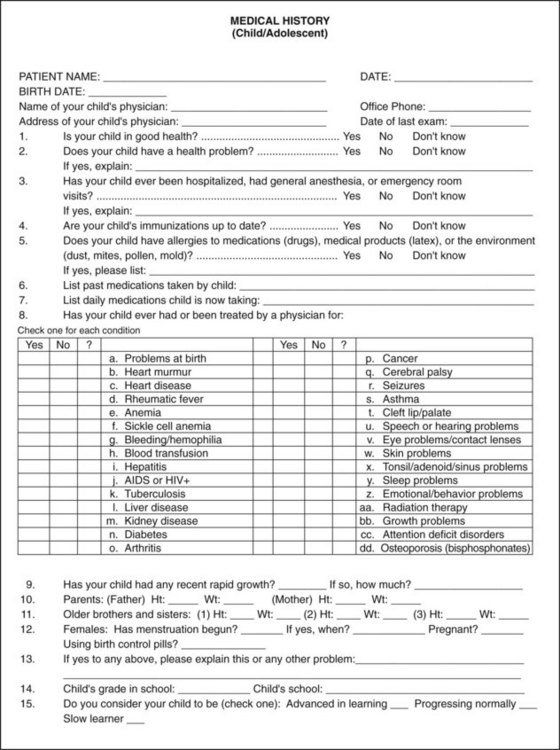
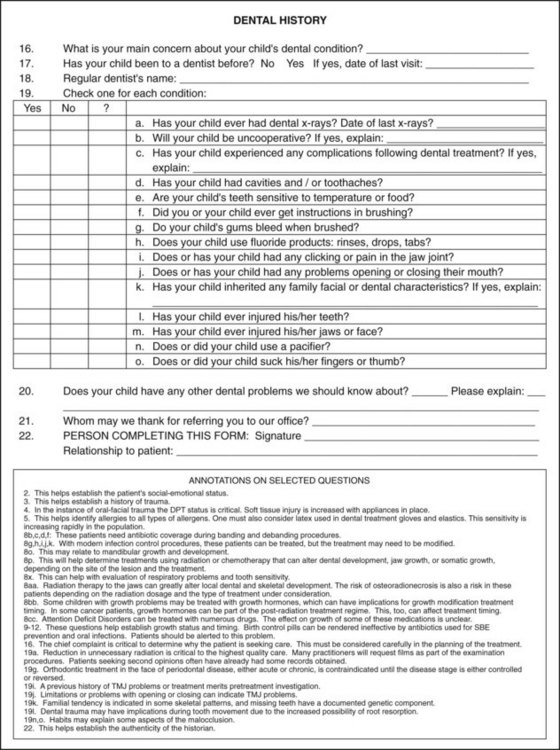
The outline of an appropriate medical and dental history is presented in Figure 6-2. A number of the items are annotated to explain their implications for an orthodontic patient.
Two areas deserve a special comment. First, although most children with a condylar fracture of the mandible recover uneventfully, remember that a growth deficit related to an old injury is the most probable cause of true facial asymmetry (Figure 6-3). It has become apparent in recent years that early fractures of the condyle occur more frequently than was previously thought (see Chapter 5). A mandibular fracture in a child can easily be overlooked in the aftermath of an accident that caused other trauma, so a jaw injury may not have been diagnosed at the time. Although old jaw fractures have particular significance, trauma to the teeth may also affect the development of the occlusion and should not be overlooked.
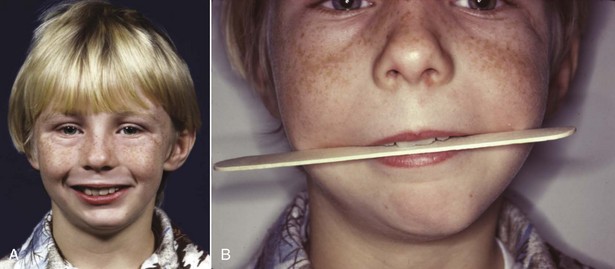
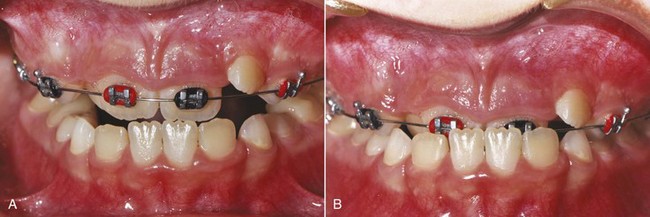
FIGURE 6-3 A, Facial asymmetry developed in this boy after fracture of the left mandibular condylar process at age 5 because scarring in the fracture area prevented normal translation of the mandible on that side during growth (see Chapter 2). B, Note the cant to the occlusal plane and the resulting roll deformity (illustrated in more detail in Figure 6-68). This develops as failure of the mandible to grow vertically on the affected side restricts eruption of both maxillary and mandibular teeth. Trauma is the most frequent cause of asymmetry of this type.
Second, it is important to note whether the patient is on long-term medication of any type and, if so, for what purpose. This may reveal systemic disease or metabolic problems that the patient did not report in any other way. Chronic medical problems in adults or children do not contraindicate orthodontic treatment if the medical problem is under control, but special precautions may be necessary if orthodontic treatment is to be carried out. For example, orthodontic treatment would be possible in a patient with controlled diabetes but would require especially careful monitoring, since the periodontal breakdown that could accompany loss of control might be accentuated by orthodontic forces (see Chapter 7). In adults being treated for arthritis or osteoporosis and now increasingly also in children with chronic disease treated with drugs (like glucocorticoids) that can be osteotoxic, high doses of resorption-inhibiting agents, such as bisphosphonates, often are used. This impedes orthodontic tooth movement and may increase the chance of complications (see Chapter 9). It may be necessary to ask specifically about these medications because parents sometimes do not mention things they think are not related to orthodontic treatment.
Physical Growth Evaluation
A third major area that should be explored by questions to the patient or parents is the individual’s physical growth status. This is important for a number of reasons, not the least of which is the gradient of facial growth discussed in Chapters 2 to 4. Rapid growth during the adolescent growth spurt facilitates tooth movement, but any attempt at growth modification will surely fail in a child who is beyond the peak of the adolescent growth spurt.
If a child is being followed for referral to an orthodontist at the optimum time or by an orthodontist for observation of growth before beginning treatment, height and weight changes can provide important insight into growth status (see Figure 2-4 for current charts). In many instances, height–weight records and the child’s progress on growth charts can be obtained from the pediatrician.
Occasionally, a more precise assessment of whether a child has reached the adolescent growth spurt is needed, and calculating bone age from the vertebrae as seen in a cephalometric radiograph can be helpful (see Figure 3-12). The primary indication for this is a child with a skeletal Class II problem who would benefit from orthodontic treatment to modify growth if that were possible. If the analysis of vertebral maturation shows delayed skeletal development, the growth spurt probably still is in the future; if the skeletal age indicates considerable maturity, adolescent growth of the jaws probably has already occurred.
Unfortunately, the stage of vertebral development is less useful in establishing other factors that sometimes are important clinically such as a patient’s position on the growth curve before or after puberty or whether jaw growth has subsided to adult levels in a teenager with mandibular prognathism. Hand–wrist radiographs are an alternative method for evaluating skeletal maturity, but these also are not an accurate way to determine when growth is completed.1 Serial cephalometric radiographs offer the most accurate way to determine whether facial growth has stopped or is continuing.
Social and Behavioral Evaluation
Cooperation is more likely to be a problem with a child than an adult. Two factors are important in determining this: (1) the extent to which the child sees the treatment as a benefit, as opposed to something else he or she is required to undergo; and (2) the degree of parental control. A resentful and rebellious adolescent, particularly one with ineffective parents, is especially likely to become a problem in treatment. It is important to take the time to understand what the patient perceives his or her problems to be and, if necessary, to help the patient appreciate the reality of the situation (see the final section of Chapter 2).
The important points to be evaluated at the interview of a prospective orthodontic patient are summarized in Figure 6-4.
Clinical Evaluation
Oral Health
In the periodontal evaluation, there are two major points of interest: indications of active periodontal disease and potential or actual mucogingival problems. Any orthodontic examination should include gentle probing through the gingival sulci, not to establish precise pocket depths but to detect any areas of bleeding. Bleeding on probing indicates inflammation that may extend into the periodontal ligament, and this must be brought under control before orthodontic treatment is undertaken. Fortunately, aggressive juvenile periodontitis (Figure 6-5) occurs rarely, but, if it is present, it is critically important to note this before orthodontic treatment begins. Inadequate attached gingiva around crowded incisors may lead to stripping of the gingiva away from the teeth when the teeth are aligned, especially if the dental arch is expanded (Figure 6-6). The interaction between periodontic and orthodontic treatment for both children and adults is discussed further in Chapter 7.
Jaw and Occlusal Function
In the evaluation of function, it is important to note in the beginning whether the patient has normal coordination and movements. If not, as in an individual with cerebral palsy or other types of severe neuromuscular disease, normal adaptation to the changes in tooth position produced by orthodontics may not occur, and the equilibrium effects discussed in Chapter 5 may lead to posttreatment relapse. Four aspects of oral function require evaluation: mastication (including but not limited to swallowing), speech, the possibility of sleep apnea related to mandibular deficiency, and the presence or absence of temporomandibular (TM) joint problems.
Patients with severe malocclusion often have difficulty in normal mastication, not so much in being able to chew their food (though this may take extra effort) but in being able to do so in a socially acceptable manner. These individuals often have learned to avoid certain foods that are hard to incise and chew and may have problems with cheek and lip biting during mastication. If asked, patients report such problems and usually indicate that after orthodontic treatment they can chew better. Unfortunately, there are almost no reasonable diagnostic tests to evaluate masticatory efficiency, so it is difficult to quantify the degree of masticatory handicap and difficult to document functional improvement. Swallowing is almost never affected by malocclusion. It has been suggested that lip and tongue weakness may indicate problems in normal swallowing, but there is no evidence to support this contention (see Chapter 5). Oral gymnastic tests (such as measuring lip strength or how hard the patient can push with the tongue) therefore add little or nothing to the diagnostic evaluation.
Speech problems can be related to malocclusion, but normal speech is possible in the presence of severe anatomic distortions. Speech difficulties in a child therefore are unlikely to be solved by orthodontic treatment. Specific relationships are outlined in Table 6-1. If a child has a speech problem and the type of malocclusion related to it, a combination of speech therapy and orthodontics may help. If the speech problem is not listed as related to malocclusion, orthodontic treatment may be valuable in its own right but is unlikely to have any impact on speech.
TABLE 6-1
Speech Difficulties Related to Malocclusion
| Speech sound | Problem | Related malocclusion |
| /s/, /z/ (sibilants) | Lisp | Anterior open bite, large gap between incisors |
| /t/, /d/ (lingua-alveolar stops) | Difficulty in production | Irregular incisors, especially lingual position of maxillary incisors |
| /f/, /v/ (labiodental fricatives) | Distortion | Skeletal Class III |
| th, sh, ch (linguodental fricatives [voiced or voiceless]) | Distortion | Anterior open bite |
Sleep apnea may be related to mandibular deficiency, and occasionally this functional problem is the reason for seeking orthodontic consultation. Both the diagnosis and management of sleep disorders requires an interdisciplinary team and should not be attempted without assessment, documentation, and referral from a qualified physician. Recent research suggests that oral appliances to advance the mandible can be effective, but only in patients with mild forms of sleep apnea, which must be established by polysomnography in a sleep laboratory before treatment in the orthodontic office begins2 (see further discussion in Chapter 7).
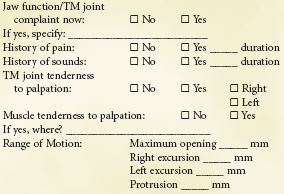
Jaw function is more than TM joint function, but evaluation of the TM joints is an important aspect of the diagnostic workup. A form for recording routine clinical examination of TM joint function is shown in Box 6-1. As a general guideline, if the mandible moves normally, its function is not severely impaired, and by the same token, restricted movement usually indicates a functional problem.3 For that reason, the most important single indicator of joint function is the amount of maximum opening. Palpating the muscles of mastication and TM joints should be a routine part of any dental examination, and it is important to note any signs of TM joint problems such as joint pain, noise, or limitation of opening.
Because the articular eminence is not well developed in children, it can be quite difficult to find the sort of positive “centric relation” position that can be determined in adults. Nevertheless, it is important to note whether the mandible shifts laterally or anteriorly when a child closes. A child with an apparent unilateral crossbite often has a bilateral narrowing of the maxillary arch, with a shift to the unilateral crossbite position. This is the most common cause of apparent but not true facial asymmetry. It is vitally important to verify this during the clinical examination or to rule out a shift and confirm a true unilateral crossbite. Similarly, many children and adults with a skeletal Class II relationship and an underlying skeletal Class II jaw relationship will position the mandible forward in a “Sunday bite,” making the occlusion look better than it really is. Sometimes an apparent Class III relationship results from a forward shift to escape incisor interferences in what is really an end-to-end relationship (Figure 6-7). These patients are said to have pseudo–Class III malocclusion.
Facial and Dental Appearance
1. Facial proportions in all three planes of space (macro-esthetics). Examples of problems that would be noted in that first step would be asymmetry, excessive or deficient face height, mandibular or maxillary deficiency or excess, and so on. In doing this, keep in mind that both the evolutionary and prenatal development of the face can provide additional insight into the origin and significance of unusual facial morphology.
2. The dentition in relation to the face (mini-esthetics). This includes the display of the teeth at rest, during speech, and on smiling. It includes such assessments as excessive gingival display, inadequate anterior tooth display, inappropriate gingival heights, and excessive or deficient buccal corridors.
3. The teeth in relation to each other (micro-esthetics). This includes assessment of tooth proportions in height and width, gingival shape and contour, connectors and embrasures, black triangular holes, and tooth shade.
Facial Proportions: Macro-Esthetics
The first step in evaluating facial proportions is to take a good look at the patient, examining him or her for developmental characteristics and a general impression. Humans are very adept at evaluating faces and in fact have a dedicated neural system for that purpose.4 Even so, with faces as with everything else, looking too quickly at the details carries the risk of missing the big picture. It is a mistake for any dentist to focus just on the teeth after a cursory look at the face. It is a disastrous mistake for an orthodontist not to evaluate the face carefully.
Assessment of Developmental Age: In a step particularly important for children around the age of puberty when most orthodontic treatment is carried out, the patient’s developmental age should be assessed. Everyone becomes a more or less accurate judge of other people’s ages—we expect to come within a year or two simply by observing the other person’s facial appearance. Occasionally, we are fooled, as when we say that a 12-year-old girl looks 15 or that a 15-year-old boy looks 12. With adolescents, the judgment is of physical maturity.
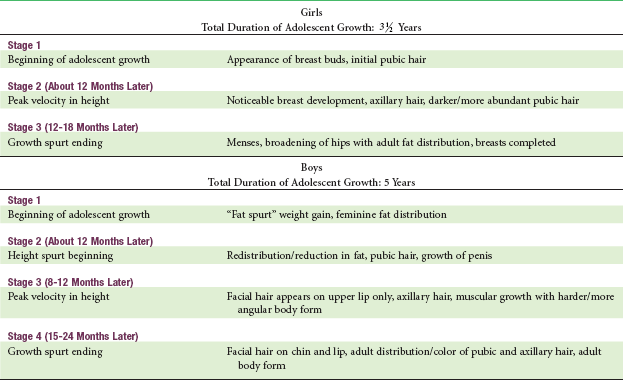
The attainment of recognizable secondary sexual characteristics for girls and boys and the correlation between stages of sexual maturation and facial growth are discussed in Chapter 4 and are summarized in Table 6-2. The degree of physical development is much more important than chronologic age in determining how much growth remains.
Facial Esthetics Versus Facial Proportions: Because a major reason for orthodontic treatment is to overcome psychosocial difficulties related to facial and dental appearance and enhance social well-being and QOL in doing so, evaluating dental and facial esthetics is an important part of the clinical examination. Whether a face is considered beautiful is greatly affected by cultural and ethnic factors, but whatever the culture, a severely disproportionate face becomes a psychosocial problem. For that reason, it helps to recast the purpose of this part of the clinical evaluation as an evaluation of facial proportions not esthetics per se. Distorted and asymmetric facial features are a major contributor to facial esthetic problems, whereas proportionate features are generally acceptable even if not beautiful. An appropriate goal for the facial examination therefore is to detect disproportions.
Frontal Examination: The first step in analyzing facial proportions is to examine the face in frontal view. Low-set ears or eyes that are unusually far apart (hypertelorism) may indicate either the presence of a syndrome or a microform of a craniofacial anomaly. If a syndrome is suspected, the patient’s hands should be examined for syndactyly, since there are a number of dental-digital syndromes.
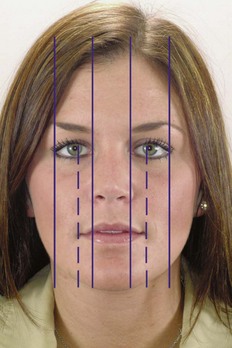
In the frontal view, one looks for bilateral symmetry in the fifths of the face and for proportionality of the widths of the eyes/nose/mouth (Figure 6-8). A small degree of bilateral facial asymmetry exists in essentially all normal individuals. This can be appreciated most readily by comparing the real full-face photograph with composites consisting of two right or two left sides (Figure 6-9). This “normal asymmetry,” which usually results from a small size difference between the two sides, should be distinguished from a chin or nose that deviates to one side, which can produce severe disproportion and esthetic problems (see Figure 6-3).
Prior to the advent of cephalometric radiography, dentists and orthodontists often used anthropometric measurements (i.e., measurements made directly during the clinical examination) to help establish facial proportions (Figure 6-10). Although this was largely replaced by cephalometric analysis for many years, the recent emphasis on soft tissue proportions has brought soft tissue evaluation back into prominence. Farkas’ modern studies of Canadians of northern European origin provided the data for Tables 6-3 and 6-4.5
TABLE 6-3
Facial Anthropometric Measurements (Young Adults)
| Parameter | Male | Female |
| 1. Zygomatic width (zy-zy) (mm) | 137 (4.3) | 130 (5.3) |
| 2. Gonial width (go-go) | 97 (5.8) | 91 (5.9) |
| 3. Intercanthal distance | 33 (2.7) | 32 (2.4) |
| 4. Pupil-midfacial distance | 33 (2.0) | 31 (1.8) |
| 5. Nasal base width | 35 (2.6) | 31 (1.9) |
| 6. Mouth width | 53 (3.3) | 50 (3.2) |
| 7. Face height (N-gn) | 121 (6.8) | 112 (5.2) |
| 8. Lower face height (subnasale-gn) | 72 (6.0) | 66 (4.5) |
| 9. Upper lip vermilion | 8.9 (1.5) | 8.4 (1.3) |
| 10. Lower lip vermilion | 10.4 (1.9) | 9.7 (1.6) |
| 11. Nasolabial angle (degrees) | 99 (8.0) | 99 (8.7) |
| 12. Nasofrontal angle (degrees) | 131 (8.1) | 134 (1.8) |
Measurements are illustrated in Figure 6-10.
Standard deviation is in parentheses.
Data from Farkas LG. Anthropometry of the Head and Face in Medicine. New York: Elsevier Science; 1991.
TABLE 6-4
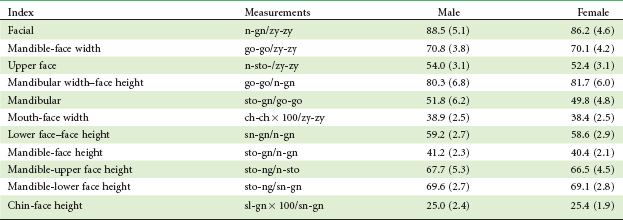
Standard deviation is in parentheses.
From Farkas LG, Munro JR. Anthropometric Facial Proportions in Medicine. Springfield, Ill.: Charles C Thomas; 1987.
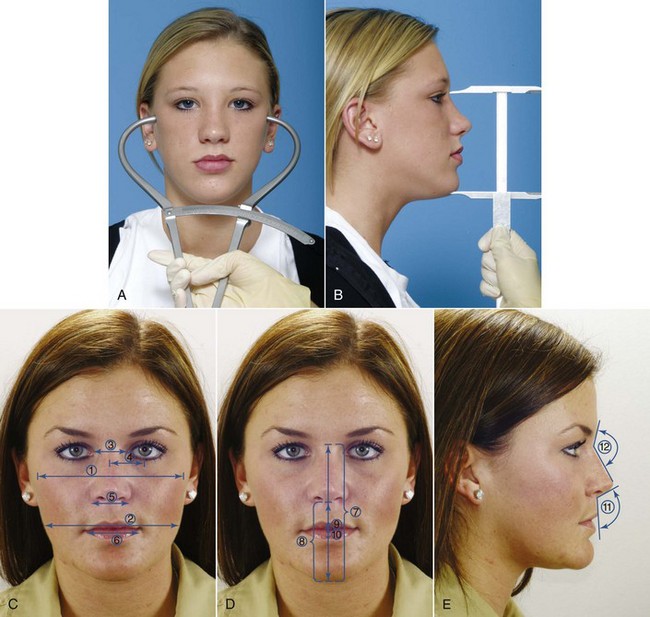
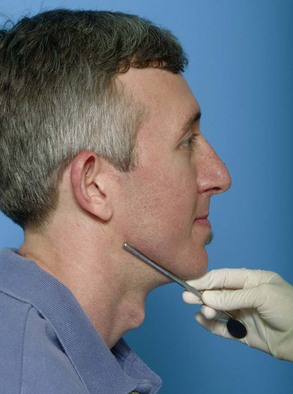
FIGURE 6-10 Facial measurements for anthropometric analysis are made with either bow calipers (A) or straight calipers (B). C to E, Frequently used facial anthropometric measurements (numbers are keyed to Table 6-3).
Note that some of the measurements in Table 6-3 could be made on a cephalometric radiograph, but many could not. When there are questions about facial proportions, it is much better to make the measurements clinically because soft-tissue proportions as seen clinically determine facial appearance. During the clinical examination, one can record measurements and literally digitize the face rather than later digitizing a cephalometric radiograph.
The normal values for the facial index and other proportions that may be clinically useful are shown in Table 6-4. Differences in facial types and body types obviously must be taken into account when facial proportions are assessed, and variations from the average ratios can be compatible with good facial esthetics. An important point, however, is to avoid treatment that would change the ratios in the wrong direction, for example, treatment with interarch elastics that could rotate the mandible downward in a patient whose face already is too long for its width.
Finally, the face in frontal view should be examined from the perspective of the vertical facial thirds. The artists of the Renaissance period, primarily da Vinci and Durer, established the proportions for drawing anatomically correct human faces (Figure 6-11). They concluded that the distance from the hairline to the base of the nose, base of nose to bottom of nose, and bottom of nose to chin should be the same. Farkas’ studies show that in modern Caucasians of European descent, the lower third is very slightly longer. The artists also saw that the lower third has a proportion of one-third above the mouth to two-thirds below, and the Farkas data show that this is still true.
It is important to note the cause of vertical problems such as excessive display of the maxillary gingiva, which is done best by examining the position of lips and teeth relative to the vertical thirds of the face (Figure 6-12). It also is important to keep in mind that different ethnic and national groups view facial esthetics somewhat differently (there are differences even in countries as closely matched as the United States and Canada) and that both gender and overall facial attractiveness influence how people are perceived. As the examining doctor, you need to notice and evaluate disproportions, even though you know that as treatment is planned, aspects of facial appearance that would be a problem for some individuals are not a problem for others with a different ethnic background.
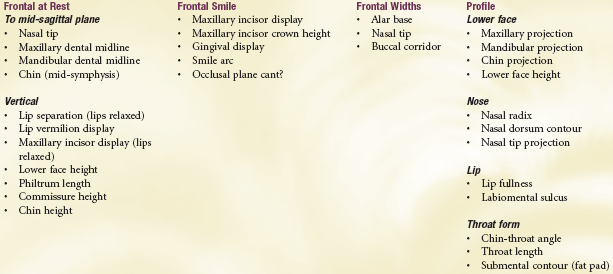
Dentofacial characteristics that should be noted as part of the facial examination are shown in Box 6-2. This checklist is just that: a list of things that should be noted systematically during the clinical examination. As in many other things, if you do not look for it, you will not see it. Precise measurements are not necessary, but deviations from the normal should be taken into account when the problem list is developed. Current computer programs already make it possible for an assistant to quickly enter positive findings as the doctor reviews them and have them “flow through” to the preliminary problem list.
Profile Analysis: A careful examination of the facial profile yields the same information, though in less detail for the underlying skeletal relationships, as that obtained from analysis of lateral cephalometric radiographs. For diagnostic purposes, particularly to identify patients with severe disproportions, careful clinical evaluation is adequate. For this reason, the technique of facial profile analysis has sometimes been called the “poor man’s cephalometric analysis.” This is a vital diagnostic technique for all dentists. It must be mastered by all those who will see patients for primary care in dentistry, not just by orthodontists.
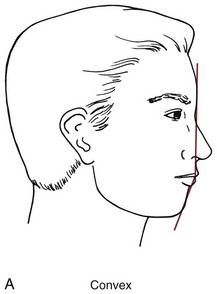
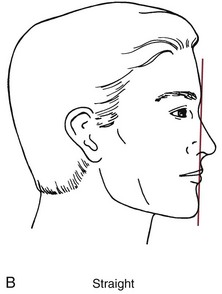
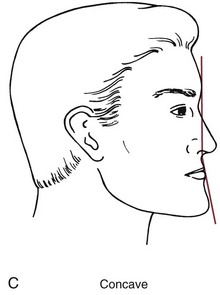
1. Establishing whether the jaws are proportionately positioned in the anteroposterior plane of space. This step requires placing the patient in the physiologic natural head position, which is the head position the individual adopts in the absence of other cues. This can be done with the patient either sitting upright or standing but not reclining in a dental chair and looking at the horizon or a distant object. With the head in this position, note the relationship between two lines, one dropped from the bridge of the nose to the base of the upper lip, and a second one extending from that point downward to the chin (Figure 6-13). These line segments ideally should form a nearly straight line, with only a slight inclination in either direction. A large angle between them (>10 degrees or so) indicates either profile convexity (upper jaw prominent relative to chin) or profile concavity (upper jaw behind chin). A convex profile therefore indicates a skeletal Class II jaw relationship, whereas a concave profile indicates a skeletal Class III jaw relationship.
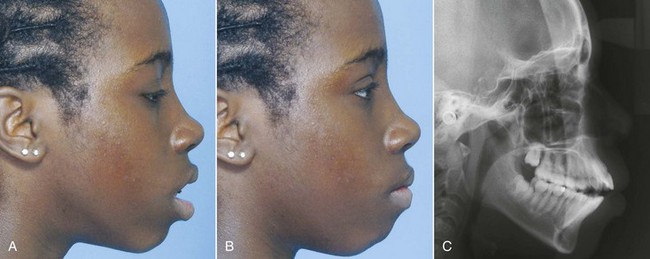
2. Evaluation of lip posture and incisor prominence. Detecting excessive incisor protrusion (which is relatively common) or retrusion (which is rare) is important because of the effect on space within the dental arches. If the incisors protrude, they align themselves on the arc of a larger circle as they lean forward, whereas if the incisors are upright or retrusive, less space is available (Figure 6-14). In the extreme case, incisor protrusion can produce ideal alignment of the teeth instead of severely crowded incisors, at the expense of lips that protrude and are difficult to bring into function over the protruding teeth. This is bimaxillary dentoalveolar protrusion, meaning simply that in both jaws the teeth protrude (Figure 6-15). Dentists often refer to the condition as just bimaxillary protrusion, a simpler term but a misnomer since it is not the jaws but the teeth that protrude. Physical anthropologists use bimaxillary protrusion to describe faces in which both jaws are prominent relative to the cranium, and the different terminology must be kept in mind when faces are described in the anthropology literature.
Determining how much incisor prominence is too much can be difficult, especially when changes over time in public preference for both lip and chin prominence are taken into account6 and ethnic differences are considered. This is simplified by understanding the relationship between lip posture and the position of the incisors. The teeth protrude excessively if (and only if) two conditions are met: (1) the lips are prominent and everted and (2) the lips are separated at rest by more than 3 to 4 mm (which is sometimes termed lip incompetence). In other words, excessive protrusion of the incisors is revealed by prominent lips that are separated when they are relaxed, so that the patient must strain to bring the lips together over the protruding teeth (see Figure 6-15). For such a patient, retracting the teeth tends to improve both lip function and facial esthetics. On the other hand, if the lips are prominent but close over the teeth without strain, the lip posture is largely independent of tooth position. For that individual, retracting the incisor teeth would have little effect on lip function or prominence.
Lip prominence is strongly influenced by racial and ethnic characteristics and to a considerable extent also is age-dependent (see Chapter 2). Whites of northern European backgrounds often have relatively thin lips, with minimal lip and incisor prominence. Whites of southern European and middle eastern origin normally have more lip and incisor prominence than their northern cousins. Greater degrees of lip and incisor prominence normally occur in individuals of Asian and African descent, so a lip and tooth position normal for Asians or blacks would be excessively protrusive for most whites.
Lip posture and incisor prominence should be evaluated by viewing the profile with the patient’s lips relaxed. This is done by relating the upper lip to a true vertical line passing through the concavity at the base of the upper lip (soft tissue point A) and by relating the lower lip to a similar true vertical line through the concavity between the lower lip and chin (soft tissue point B; Figure 6-16). If the lip is significantly forward from this line, it can be judged to be prominent; if the lip falls behind the line, it is retrusive. If the lips are both prominent and incompetent (separated by more than 3 to 4 mm), the guideline is that the anterior teeth are excessively protrusive. Is that a problem? It depends on both the patient’s perception and the cultural setting, not just on the objective evaluation.
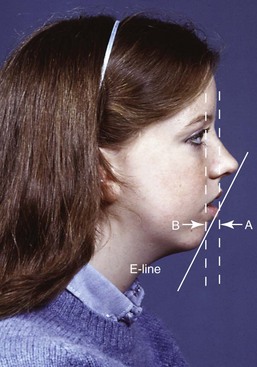
In evaluating lip protrusion, it is important to keep in mind that everything is relative, and in this case the lip relationships with the nose and chin affect the perception of lip fullness. The larger the nose, the more prominent the chin must be to balance it, and the greater the amount of lip prominence that will be esthetically acceptable. It can be helpful to look at lip prominence relative to a line from the tip of the nose to the chin (the E-line of cephalometric analysis, which can be visualized easily on clinical examination; Figure 6-17). Vertical facial and dental relationships also play a role here. Some patients with short lower face height have everted and protrusive lips because they are overclosed and the upper lip presses against the lower lip, not because the teeth protrude.
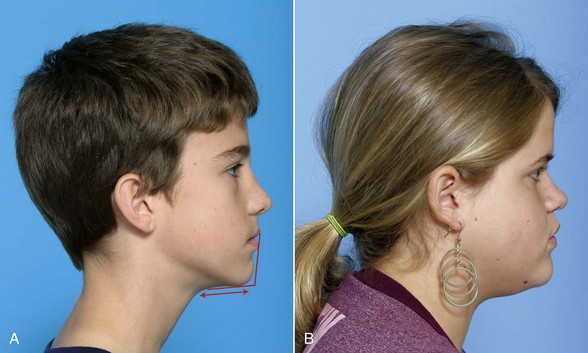
Not only the prominence of the chin but also the submental soft tissue contours should be evaluated. Throat form is an important factor in establishing optimal facial esthetics, and poor throat form is a major contributor to esthetic impairment in patients with mandibular deficiency (Figure 6-18).
3. Reevaluation of vertical facial proportions and evaluation of mandibular plane angle. Vertical proportions can be observed during the full-face examination (see previous section) but sometimes can be seen more clearly in profile. In the clinical examination, the inclination of the mandibular plane to the true horizontal should be noted. The mandibular plane is visualized readily by placing a finger or mirror handle along the lower border (Figure 6-19). A steep mandibular plane angle usually accompanies long anterior facial vertical dimensions and a skeletal open bite tendency, while a flat mandibular plane angle often correlates with short anterior facial height and deep bite malocclusion.
Tooth–Lip Relationships: Mini-Esthetics
Tooth–Lip Relationships: Evaluation of tooth–lip relationships begins with an examination of symmetry, in which it is particularly important to note the relationship of the dental midline of each arch to the skeletal midline of that jaw (i.e., the lower incisor midline relative to the midline of the mandible, and the upper incisor midline relative to the midline of the maxilla). Dental casts, even if mounted on an articulator, will show the relationship of the midlines to each other but provide no information about the dental-skeletal midlines. This must be recorded during the clinical examination.
A second aspect of dental to soft tissue relationships is the vertical relationship of the teeth to the lips at rest and on smile. During the clinical examination, it is important to note the amount of incisor display. For patients with excessive incisor display, the usual cause is a long lower third of the face, but that is not the only possibility—a short upper lip could produce the same thing (see Figure 6-12). Recording lip height at the philtrum and the commissures can clarify the source of the problem.
A third important relationship to note is whether an up-down transverse rotation of the dentition is revealed when the patient smiles or the lips are separated at rest (Figure 6-20). This often is called a transverse cant of the occlusal plane but is better described as a transverse roll of the esthetic line of the dentition (see the section in this chapter on classification by dentofacial traits). Neither dental casts nor a photograph with lip retractors will reveal this. Dentists detect a transverse roll at 1 mm from side to side, whereas laypersons are more forgiving and see it at 2 to 3 mm—but at that point, it is a problem.7
Smile Analysis: Facial attractiveness is defined more by the smile than by soft tissue relationships at rest. For this reason, it is important to analyze the characteristics of the smile and to think about how the dentition relates to the facial soft tissues dynamically, as well as statically. There are two types of smiles: the posed or social smile and the enjoyment smile (also called the Duchenne smile in the research literature). The social smile is reasonably reproducible and is the one that is presented to the world routinely. The enjoyment smile varies with the emotion being displayed (for instance, the smile when you are introduced to a new colleague differs from the smile when your team just won the year’s most important game). The social smile is the focus of orthodontic diagnosis.
In smile analysis, the oblique view and the frontal and profile views are important. The following variables need to be considered along with the viewing perspective (Box 6-3).
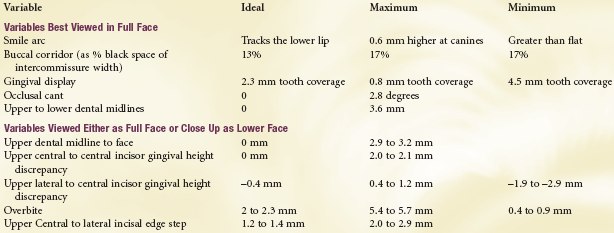
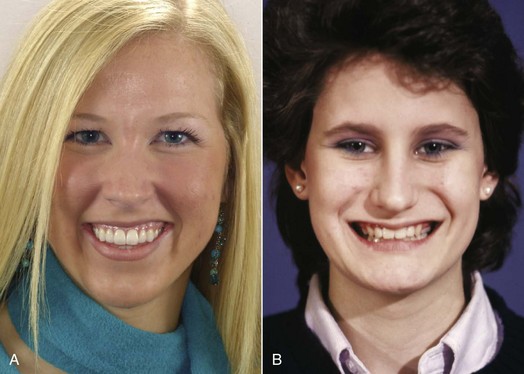
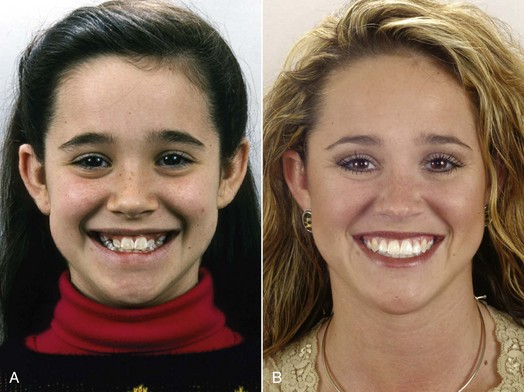
Amount of Incisor and Gingival Display: Using computer-altered photographs, recent research has established a range of acceptability for incisor and gingival display (Figure 6-21).8 Although some display of gingiva is acceptable and can be both esthetic and youthful appearing, the ideal elevation of the lip on smile for adolescents is slightly below the gingival margin, so that most of the upper incisor can be seen. More importantly, up to 4 mm display of gingiva in addition to the crown of the tooth, or up to 4 mm lip coverage of the incisor crown, is acceptable. Beyond that, the smile appearance is less attractive.
It also is important to remember that the vertical relationship of the lip to the incisors will change over time, with the amount of incisor exposure decreasing (see Chapter 4).9 This makes it even more important to note the vertical tooth–lip relationships during the diagnostic evaluation and to keep it in mind during treatment.
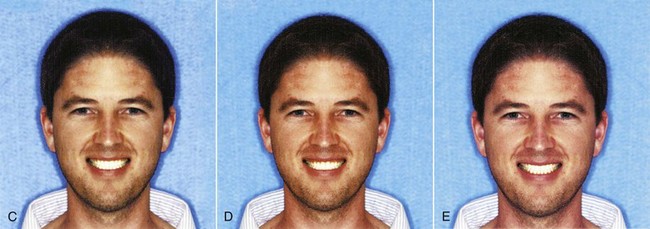
Transverse Dimensions of the Smile Relative to the Upper Arch: Depending on the facial index (i.e., the width of the face relative to its height), a broad smile may be more attractive than a narrow one—but what does that mean exactly? A dimension of interest to prosthodontists, and more recently to orthodontists, is the amount of buccal corridor that is displayed on smile, that is, the distance between the maxillary posterior teeth (especially the premolars) and the inside of the cheek (Figure 6-22). Prosthodontists consider excessively wide buccal corridors (sometimes called “negative space”) to be unesthetic, and orthodontists have noted that widening the maxillary arch can improve the appearance of the smile if cheek drape is significantly wider than the dental arch. Although minimal buccal corridors are favored by most observers, especially in females,10 the transverse width of the dental arches can and should be related to the width of the face (Figure 6-23). Too broad an upper arch, so that there is no buccal corridor, is unesthetic. The relationship of the cheeks to the posterior teeth on smile is just another way of evaluating the width of the dental arches.
The Smile Arc: The smile arc is defined as the contour of the incisal edges of the maxillary anterior teeth relative to the curvature of the lower lip during a social smile (Figure 6-24). For best appearance, the contour of these teeth should match that of the lower lip. If the lip and dental contours match, they are said to be consonant.
A flattened (nonconsonant) smile arc can pose either or both of two problems: it is less attractive and tends to make you look older (because older individuals often have wear of the incisors that tends to flatten the arc of the teeth). The characteristics of the smile arc must be monitored during orthodontic treatment because it is surprisingly easy to flatten it in the pursuit of other treatment objectives. The data indicate that the most important factor in smile esthetics, the only one that by itself can change the rating of a smile from acceptable to unesthetic, is the smile arc.8
It is important to keep in mind that these features of the smile are viewed differently by patients when the full face is the context (i.e., they are looking into a large mirror mounted so that they can see their whole face) instead of just seeing their lips and teeth (in a hand-held mirror that shows only part of the face). With the full-face view, the smile arc is judged most attractive when the upper incisal edges and canines parallel the curvature of the lower lip. The preferred buccal corridors are small, significantly smaller than when judged using the smaller mirror. A transverse cant of the occlusal plane is less tolerated in the full-face view, but more upper to lower midline discrepancy is acceptable.11,12 When patients have complaints about these specific smile components, it is best to have them point out what concerns them while they are looking into a large mirror that lets them see their entire face—just as others will view them in real life encounters.
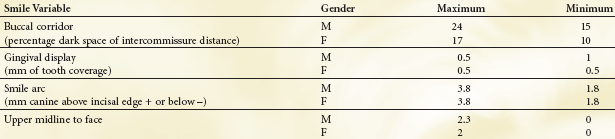
Because facial attractiveness and gender do make a difference for some of these features, Box 6-4 shows a range of acceptability for characteristics in which this is important. Although there are modest differences between ethnic groups13 and nationalities (even Canadians and Americans)14 in their judgment of smile esthetics, the safe ranges had some commonality for groups that were predominantly of European descent. Similar data for Asian and African groups do not exist at present.
Dental Appearance: Micro-Esthetics
Subtleties in the proportions and shape of the teeth and associated gingival contours have been emphasized in the burgeoning literature on “cosmetic dentistry” in recent years. A similar evaluation is necessary in the development of an orthodontic problem list if an optimal esthetic result is to be obtained. Treatment planning to correct problems of this type is discussed in Chapter 7.
Tooth Proportions: The smile, of course, reveals the maxillary anterior teeth, and two aspects of proportional relationships are important components of their appearance: the tooth widths in relation to each other and the height–width proportions of the individual teeth.
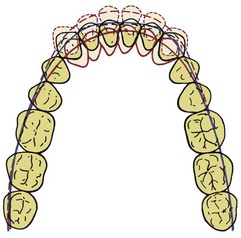
Width Relationships and the “Golden Proportion.”: The apparent widths of the maxillary anterior teeth on smile, and their actual mesiodistal width, differ because of the curvature of the dental arch. In particular, only a portion of the canine crown can be seen in a frontal view. For best appearance, the apparent width of the lateral incisor (as one would perceive it from a direct frontal examination) should be 62% of the width of the central incisor, the apparent width of the canine should be 62% of that of the lateral incisor, and the apparent width of the first premolar should be 62% of that of the canine (Figure 6-25). This ratio of recurring 62% proportions appears in a number of other relationships in human anatomy and sometimes is referred to as the “golden proportion.” Whether it has any mystical significance or not, it is an excellent guideline when lateral incisors are disproportionately small or (less frequently) large, and the width ratios of the central and lateral are the best way to determine what the posttreatment size of the lateral incisor should be. The same judgment is used when canines are narrowed to replace missing lateral incisors.
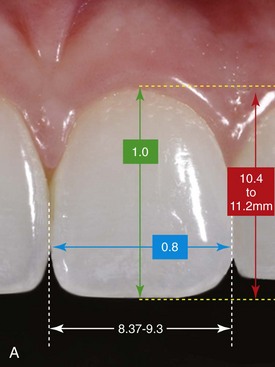
Height–Width Relationships: The range in height–width relationships for maxillary central incisors is shown in Figure 6-26. Note that the width of the tooth should be about 80% of its height. In examining an orthodontic patient, it is important to note both height and width because if disproportions are noted, this allows a determination of which is at fault. The central incisor seen in Figure 6-26, B, looks almost square. Its width measures 8.7 mm and its height 8.5 mm. From the table, the 8 mm width is in the middle of the normal range, and the height is short. There are several possible causes: incomplete eruption in a child, which may correct itself with further development; loss of crown height from attrition in an older patient, which may indicate restoration of the missing part of the crown; excessive gingival height, which is best treated with crown lengthening; or perhaps an inherent distortion in crown form, which suggests a more extensive restoration with facial laminates or a complete crown (see Chapter 18). The disproportion and its probable cause should be included in the patient’s problem list to focus attention on doing something about it before orthodontic treatment is completed.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses