Fundamentals of Tooth Preparation and Pulp Protection
Definition of Tooth Preparation
Much of the scientific foundation of tooth preparation techniques was presented by Black.1 Modifications of Black’s principles of tooth preparation have resulted from the influence of Bronner, Markley, J. Sturdevant, Sockwell, and C. Sturdevant; from improvements in restorative materials, instruments, and techniques; and from the increased knowledge and application of preventive measures for caries.2–6
In the past, most tooth preparations were precise procedures, usually resulting in uniform depths, particular wall forms, and specific marginal configurations. Such precise preparations are still required for amalgam, cast metal, and ceramic restorations and may be considered conventional preparations. Conventional preparations require specific wall forms, depths, and marginal forms because of the properties of the restorative material. The use of adhesive restorations, primarily composites and glass ionomers, has allowed a reduced degree of precision of tooth preparations. Many composite restorations may require only the removal of the defect (caries, fracture, or defective restorative material) and friable tooth structure for tooth preparation, without specific uniform depths, wall designs, retentive features or marginal forms. This simplification of procedures results in a modified preparation and is possible because of the physical properties of the composite material and the strong bond obtained between the composite and the tooth structure (Table 5-1).
Table 5-1
Tooth Preparation: Amalgam versus Composite
| Amalgam | Composite | |
| Outline form | Include defect | Same |
| May extend to break proximal contact | Same | |
| Include adjacent suspicious area | No | |
| Seal these areas | ||
| Pulpal depth | Uniform 1.5 mm | Remove defect; not usually uniform |
| Axial depth | Uniform 0.2-0.5 mm inside DEJ | Remove defect; not usually uniform |
| Cavosurface margin | Create 90-degree amalgam margin | ≥90 degrees |
| Bevels | None (except gingival) | Large preparation, esthetics, and seal |
| Texture of prepared walls | Smoother | Rough |
| Cutting instrument | Burs | Burs or diamonds |
| Primary retention form | Convergence occlusally | None (roughness/bonding) |
| Secondary retention form | Grooves, slots, pins, (bonding) | Bonding; grooves for very large or root-surface preparation |
| Resistance form | Horizontal floors, rounded angles, box-shaped (floors perpendicular to occlusal forces) | Same for large preparations; no special form for small- to moderate-size preparations |
| Base indications | Provide 2 mm between pulp and amalgam | Not needed |
| Liner indications | Ca(OH)2, for pulp exposures or near exposures RMGI in deep preparations | Same (also may use RMGI liner on root-surface extensions) |
| Desensitizer | Dentin desensitizer (5% glutaraldehyde + 35% HEMA) when not bonding | Sealed by bonding system used |
Ca(OH)2, calcium hydroxide; HEMA, 2-hydroxyethyl methacrylate; RMGI, resin-modified glass ionomer.
Need for Restorations
Teeth need restorative intervention for various reasons. Dental caries is an infectious disease, and prevention often requires prophylactic restorative procedures (see Chapter 2). Caries progression may cause destruction of tooth structure which requires repair. Another common need is the replacement or repair of restorations with serious defects such as improper proximal contact, gingival excess of restorative material, defective (open) margins, or poor esthetics. Restorations also are indicated to restore proper form and function to fractured teeth. Such teeth present with minor to major amounts of missing tooth structure or with an incomplete fracture (“greenstick fracture”), resulting in a tooth that has compromised function and often also associated pain or sensitivity. A tooth may require a restoration simply to restore form or function that is absent as a result of congenital malformation or improper position. Restorations also are required for teeth simply as part of fulfilling other restorative needs. When replacing a missing tooth with a fixed or removable partial denture, the teeth adjacent to the space may require some type of restorative procedure to allow for optimal placement and function of the prosthesis. Careful diagnosis and development of a comprehensive treatment plan must be accomplished before the restoration of individual teeth is pursued to ensure appropriate restorative intervention.
Factors Affecting Tooth Preparation
General Factors
Diagnosis
Restorative Material Factors
The choice of restorative material affects the tooth preparation and is made by considering many factors. The patient’s input into the decision is important. Economic and esthetic considerations are primarily patient decisions. The ability to isolate the operating area and the extent of the lesion or defect are factors that the operator must consider in presenting material options to the patient. Table 5-1 compares factors related to restorative choices when choosing between amalgam and composite materials.
Nomenclature
Caries Terminology
Location of Caries
Caries can be described according to location, extent, and rate.7
Primary Caries
Primary caries is the original caries lesion of the tooth. The etiology, morphology, control, and prevention of caries are presented in Chapter 2. Variations of this pathologic condition are associated with certain areas of teeth and fundamentally influence tooth preparation. Three morphologic types of primary caries are evident in clinical observation: (1) lesions originating in enamel pits and fissures, (2) lesions originating on enamel smooth surfaces, or (3) lesions originating on root surfaces. Also described in the following sections are backward caries, forward caries, and residual caries. Of these, the terms backward caries and forward caries are rarely used.
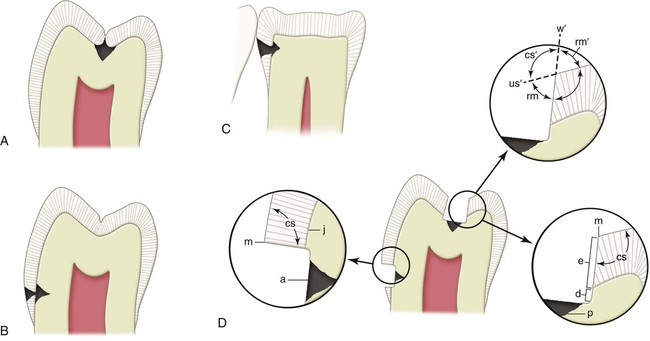
Caries of Pit-and-Fissure Origin
Complete coalescence of the enamel developmental lobes results in enamel surface areas termed grooves and fossae. Usually, these areas are not susceptible to caries because they are cleansed by the rubbing of food during mastication. Caries may develop in a groove or fossa, however, in areas of no masticatory action in neglected mouths. Imperfect coalescence of the developmental enamel lobes will result in enamel surface pits and fissures. When such areas are exposed to oral conditions conducive to demineralization, caries may develop (Fig. 5-1, A). The caries forms a small area of penetration in the enamel at the bottom of a pit or fissure and does not spread laterally to a great extent until the dentinoenamel junction (DEJ) is reached. Dentin caries initially spreads laterally along the DEJ and begins to penetrate the dentin toward the pulp via the dentinal tubules. This lateral and pulpal progression results in unsupported enamel. In diagrammatic terms, pit-and-fissure caries may be represented as two cones, base to base, with the apex of the enamel cone at the point of origin and the apex of the dentin cone directed toward the pulp. As caries progresses in these areas, sometimes little evidence is clinically noticeable until the forces of mastication fracture the increasing amount of unsupported enamel.
Caries of Enamel Smooth-Surface Origin
Smooth-surface caries does not begin in an enamel defect but, rather, in a smooth area of the enamel surface that is habitually unclean and is continually, or usually, covered by plaque (see Figs. 5-1, B and C). It is emphasized in Chapter 2 that plaque is necessary for caries and that additional oral conditions also must be present for caries to ensue. The enamel disintegration in smooth-surface caries also may be pictured as a cone, but with its base on the enamel surface and the apex at, or directed toward, the DEJ. The caries again spreads at this junction in the same manner as in pit-and-fissure caries. The apex of the cone of caries in the enamel contacts the base of the cone of caries in the dentin.
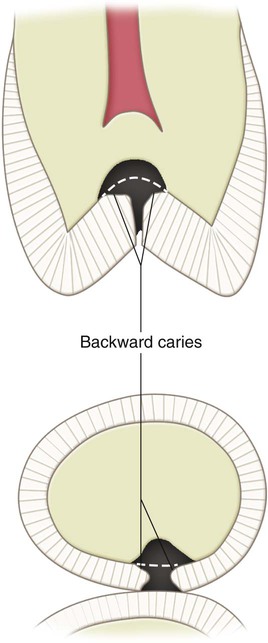
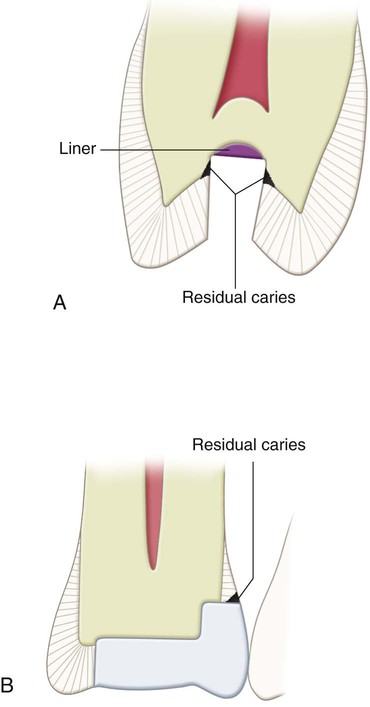
Residual Caries
Residual caries is caries that remains in a completed tooth preparation, whether by operator intention or by accident. Such caries is not acceptable if it is present at the DEJ or on the prepared enamel tooth wall (Fig. 5-3). It may be acceptable, however, when it exists as affected dentin, especially near the pulp (see the section Affected and Infected Dentin).
Root-Surface Caries
Root-surface caries may occur on the tooth root that has been exposed to the oral environment and habitually covered with plaque (Fig. 5-4). Additional oral conditions (discussed in Chapter 2) conducive to caries development also must be present and often are prevalent in older patients. Root caries is usually more rapid than other forms of caries and should be detected and treated early. Root caries is becoming more prevalent because a greater number of older individuals are retaining more of their teeth and experiencing gingival recession, both of which increase the likelihood of root caries development.
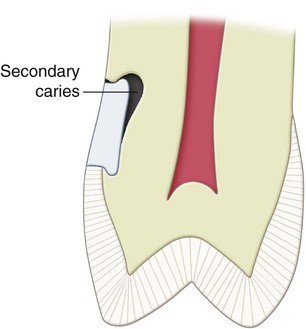
Secondary (Recurrent) Caries
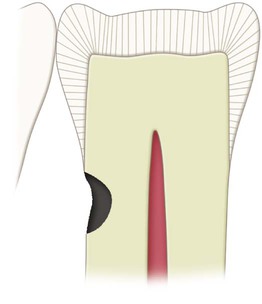
Secondary caries occurs at the junction of a restoration and the tooth and may progress under the restoration. It is often termed recurrent caries. This condition usually indicates that microleakage is present, along with other conditions conducive to caries development (Fig. 5-5).
Grooves and Fissures; Fossae and Pits
Chapter 1 presented information on the development of the enamel surface of the tooth. Anatomic depressions mark the location of the union of developmental enamel lobes. Where such union is complete, this “landmark” is only slightly involuted, smooth, hard, shallow, accessible to cleansing, and termed groove. Where such union is incomplete, the landmark is sharply involuted to form a narrow, inaccessible canal of varying depths in the enamel and is termed fissure. The distinction made between a groove and a fissure also applies to an enamel surface fossa, which is nondefective enamel lobe union, and a pit, which is defective. A fissure (or pit) may be a trap for plaque and other oral elements that together can produce caries, unless the surface enamel of the fissure or pit walls is fluoride rich.
Extension for Prevention
Black noted that in tooth preparations for smooth-surface caries, the restoration should be extended to areas that are normally self-cleansing to prevent recurrence of caries.1 This principle was known as extension for prevention and was broadened to include the extension necessary to remove remaining enamel defects such as pits and fissures. The practice of extension for the prevention on smooth surfaces virtually has been eliminated, however, because of the relative caries immunity provided by preventive measures such as fluoride application, improved oral hygiene, and a proper diet. This change has fostered a more conservative philosophy defining the factors that dictate extension on smooth surfaces to be (1) the extent of caries or injury and (2) the restorative material to be used. Likewise, extension for prevention to include the full length of enamel fissures has been reduced by treatments that conserve tooth structure. Tooth structure conservation ultimately leads to restored teeth that are stronger and more resistant to fracture. Such treatments are enameloplasty, application of pit-and-fissure sealant, and preventive resin or conservative composite restoration.9
Enameloplasty
Enameloplasty is the removal of a shallow developmental fissure or pit in enamel to create a smooth, saucer-shaped surface that is self-cleansing or easily cleaned. This prophylactic procedure can be applied not only to fissures and pits and deep supplemental grooves but also to some shallow, smooth-surface enamel defects (see Initial Tooth Preparation Stage later in the chapter).
Prophylactic Odontotomy
Prophylactic odontotomy is presented only as a historical concept.10 The procedure involves minimal preparation and amalgam filling of the developmental, structural imperfections of enamel, such as pits and fissures, to prevent caries originating in these sites. Prophylactic odontotomy is no longer advocated as a preventive measure.
Affected and Infected Dentin
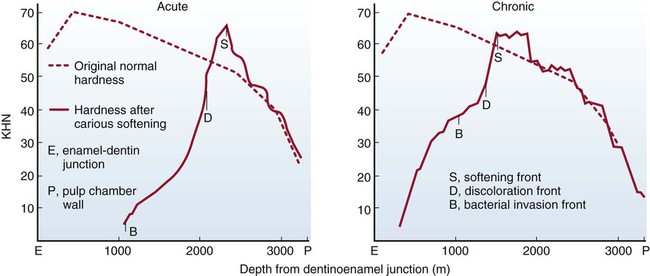
Fusayama reported that carious dentin consists of two distinct layers—an outer layer and an inner layer.11 This textbook refers to the outer layer as infected dentin and the inner layer as affected dentin. In tooth preparation, it is desirable that only infected dentin be removed, leaving affected dentin, which may be remineralized in a vital tooth after the completion of restorative treatment. This principle for the removal of dentinal caries is supported by the observation by Fusayama et al. that the softening front of the lesion always precedes the discoloration front, which always precedes the bacterial front.12
Infected dentin has bacteria present, and collagen is irreversibly denatured. It is not remineralizable and must be removed. Affected dentin has no bacteria, and the collagen matrix is intact, is remineralizable, and should be preserved. To clinically distinguish these two layers, the operator traditionally observes the degree of discoloration (extrinsic staining) and tests the area for hardness by the feel of an explorer tine or a slowly revolving bur. Some difficulties occur with this approach because (1) the discoloration may be slight and gradually changeable in acute (rapid) caries, and (2) the hardness (softness) felt by the hand through an instrument may be an inexact guide. To differentiate between remineralizable and non-remineralizable dentin, staining carious dentin was proposed by Fusayama.11 Caries-detecting dyes are not specific for infected dentin and will stain the slightly demineralized protein matrix of affected dentin as well as normal DEJ.13 Caries-detecting dyes should be used with caution and only as an adjunct to clinical evaluation.
In chronic caries, infected dentin usually is discolored, and because the bacterial front is close to the discoloration front, it is advisable, in caries removal, to remove all discolored dentin unless judged to be within 0.5 mm of the pulp (Fig. 5-6). Because the discoloration is slight in acute caries, and the bacterial front is well behind the discoloration front, some discolored dentin may be left, although any “clinically remarkable” discoloration should be removed.12
Non-carious Tooth Defects Terminology
Abrasion
Abrasion is abnormal tooth surface loss resulting from direct forces of friction between teeth and external objects or from frictional forces between contacting teeth components in the presence of an abrasive medium.8 Abrasion may occur from (1) improper brushing techniques, (2) habits such as holding a pipe stem between teeth, (3) tobacco chewing, or (4) vigorous use of toothpicks between adjacent teeth. Toothbrush abrasion is the most common example and is usually seen as a sharp, V-shaped notch in the gingival portion of the facial aspect of a tooth.
Abfraction
It has been proposed that the predominant causative factor of some cervical, wedge-shaped defects is a strong eccentric occlusal force (frequently manifested as an associated wear facet) resulting in microfractures or abfractures. Such microfractures occur as the cervical area of the tooth flexes under such loads. This defect is termed idiopathic erosion or abfraction.14
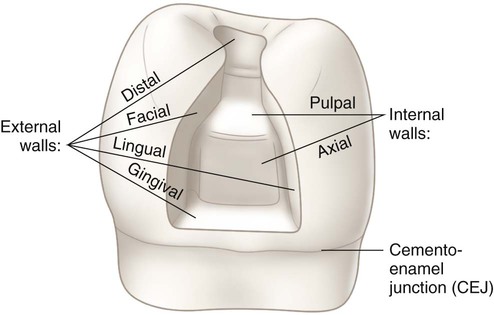
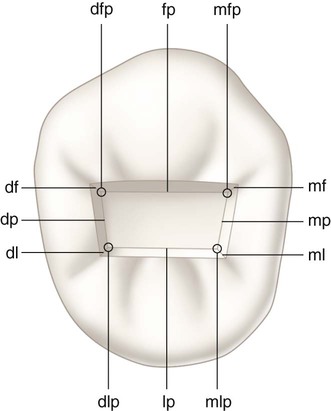
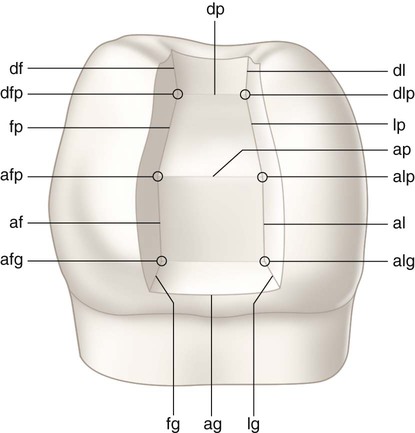
Tooth Preparation Terminology
Simple, Compound, and Complex Tooth Preparations
Tooth Preparation Angles
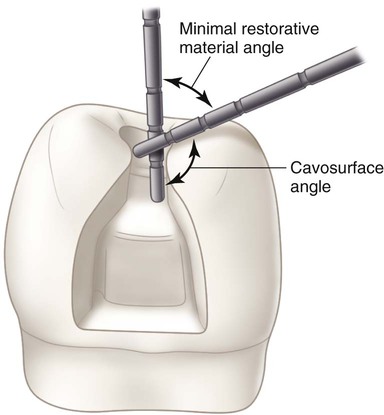
Cavosurface Angle and Cavosurface Margin
The cavosurface angle is the angle of tooth structure formed by the junction of a prepared wall and the external surface of the tooth. The actual junction is referred to as cavosurface margin. The cavosurface angle may differ with the location on the tooth, the direction of the enamel rods on the prepared wall, or the type of restorative material to be used. In Figure 5-1, D, the cavosurface angle (cs) is determined by projecting the prepared wall in an imaginary line (w′) and the unprepared enamel surface in an imaginary line (us′) and noting the angle (cs′) opposite to the cavosurface angle (cs). For better visualization, these imaginary projections can be formed by using two periodontal probes, one lying on the unprepared surface and the other on the prepared external tooth wall (Fig. 5-10).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses